Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.77 no.5 Johannesburg 2022
http://dx.doi.org/10.17159/2519-0105/2022/v77no5a7
CASE REPORT
http://dx.doi.org/10.17159/2519-0105/2022/v77no5a7
Bilateral Radicular Cyst - A Rare Case Presentation
S KarpagavalliI; S SubramanianII; V VaishnaviIII; G SivadasIV
IShanmugasundaram Karpagavalli: (MDS) Prof & Head, Dept. of Oral Medicine & Radiology, Seema Dental College & Hospital, Rishikesh, Uttarakhand
IISathasiva Subramanian: (MDS) Prof & Head Dept. of Oral Medicine & Radiology , Faculty of Dental Sciences, Sri Ramachandra Unversity, Chennai, Tamil Nadu
IIIVedam Vaishnavi: (MDS) Senior Lecturer, Faculty of Dentistry, AIMST Unversity, Malaysia
IVGanapathy Sivadas: (MDS) Senior Lecturer, Faculty of Dentistry, AIMST University, Malaysia
ABSTRACT
Radicular cyst usually originates as a sequel to a periapical inflammatory process following an injury. This report presents a case of radicular cyst with "bilateral involvement" of permanent central incisors with an atypical radiographical finding and pathological picture that has been discussed. An extensive review of radicular cyst with rarity as seen in the present case was studied. Further importance on treatment with a long term following up of the patient was noted. A sound knowledge regarding the rarity of this lesion is necessary to aid in early diagnosis with an appropriate treatment plan for general practitioners.
Key words: Bilateral radicular cyst, inflammatory cyst, cell rests of malassez, cholesterol clefts
INTRODUCTION
Radicular cysts is the most common inflammatory epithelial cysts occurring in 7-54% of all jaw cysts.1 Synonymously, this lesion is termed by inflammatory periapical cyst, dental cyst and root end cyst. Varied etiologies like dental caries-pulp necrosis, trauma, tooth fracture, improper restoration, infection and long term chronic periapical granuloma may result in the formation of this radicular cyst.2 Frequently, these asymptomatic lesions are diagnosed on routine clinical and radiographic examination.3
These lesions are afterward confirmed on pathological examination correlating to the preexisting radiographic and clinical aids by the clinician. The purpose of this article is to report the occurrence of a relatively rare case of radicular cyst involving two adjacent teeth exhibiting an atypical radiographic and histopathological appearance. This article also highlights the etiopathogenesis, clinical, radiographic and histopathology picture, with various modes of treatment.
CASE PRESENTATION
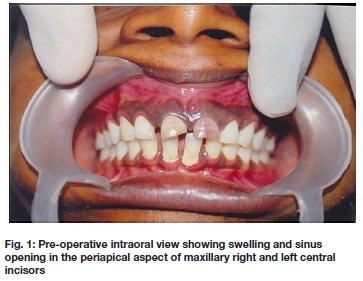
A twenty-six-year-old female reported with a complaint of mobile upper front teeth for the past two years. Her history revealed that she suffered trauma to these teeth during a bicycle accident sixteen years earlier, following which she noticed fractures of these teeth. The patient was symptomatically treated with medications in a local hospital, but eventually the teeth started to discolor and pus drained from apical fistulae. On intraoral examination, there was a soft, fluctuant non-tender diffuse swelling in relation to the discolored mobile upper central incisor teeth (Fig. 1). Pus discharge in the periapical aspect of the same teeth was also noticed. There were no other abnormalities seen.
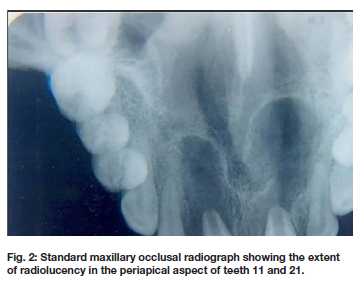
Vitality test of the maxillary central incisors was negative. Fine needle aspiration (FNAC) collected 0.5 ml of straw-colored fluid, presumed to be pus with blood content. Radiographs (intraoral periapical radiograph and standard maxillary occlusal radiograph) revealed an osteolytic radiolucency which was well-delineated around the roots of the teeth, and had a radio-opaque sclerotic border (Fig. 2). Based on the history as well as the clinical-and laboratory findings, a provisional diagnosis of an infected radicular cyst associated with the fractured upper central incisors was made. Then, preoperative recommendations and laboratory blood tests (complete blood count and activated partial thromboplastin time (APTT) was performed before the surgical intervention. Treatment consisted of cyst enucleation and extraction of the upper central incisors followed by suturing and wound care. The specimens were fixed in 10% formalin and sent for routine microscopic examination to confirm the provisional diagnosis of a radicular cyst.
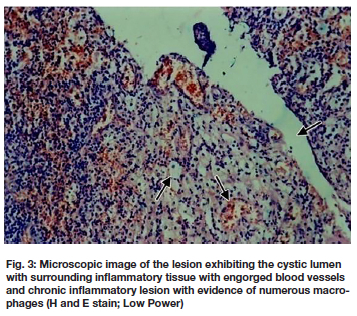
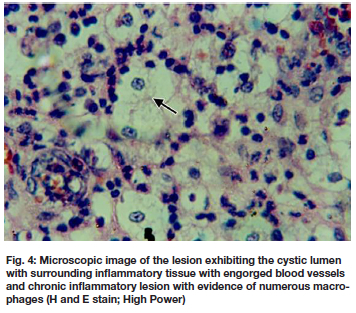
Histologic examination of both tissue specimens exhibited similar picture: a cystic lumen lined by varying thickness of non-keratinized stratified squamous epithelium with an arcading appearance (Fig. 3). The surrounding connective tissue capsule was severely infiltrated by chronic inflammatory cells, Rushton bodies, foam cells, cholesterol clefts, and numerous blood capillaries and extravasated RBCs (Fig. 4). These findings confirmed the diagnosis of radicular cyst. No complication or residue was seen on a 2-year follow-up.
DISCUSSION
Radicular cysts are one of the frequently seen jaw cysts in the oral and maxillofacial region. Demographically, these lesions occur in the third to fourth decades of life with a slight male predominance (3:2). Most of the radicular cysts are found in the maxilla, especially around incisors and canines (3:1).4 The prevalence rate varies between 8.7% to 37.7% of all chronic inflammatory lesions.5 Radicular cysts slowly increase in size to eventually cause cortical plate expansion, which is characterized by egg-shell crackling. Pain is possible if the lesion becomes secondarily infected.
Radio graphically, radicular cysts may mimic a Dentigerous cysts, Odontogenic keratocysts, and Odontogenic tumors such as Ameloblastoma, Pindborg tumor, Odontogenic fibroma, and Cementomas.7 The common signs of radicular cysts are buccal cortical plate expansion, well defined radiolucency, thin reactive cortex and displacement of adjacent permanent teeth. The radiographical picture in our case resembles the literature findings, but with a slightly varied presentation. This case represents two separate radiolucent lesions involving permanent maxillary right and left central incisors with each lesion surrounded by a separate well-defined radio-opaque border.
The etiopathogenesis of radicular cysts still remains controversial. Various theories have been proposed, such as epithelial colonization, epithelial cavitations, and microabscess formation.8 Among them, the most accepted theory suggests that the accumulated epithelial cells of the existing periapical granulomas undergo degeneration and necrosis due to the decreased vascularization resulting in a central area of the cyst surrounded by the arcading pattern of proliferating epithelium. These lesions start proliferating from the epithelial remnants of cells of Malassez (periodontal ligament), the sinus lining or lining of fistulous tracts depending on various sites of occurrence.9
The pathogenesis of cysts has been described in three phases. Initially, the epithelial cell rests of Malassez begin to proliferate as a direct result of the inflammation and are subsequently altered by bacterial antigens, epidermal growth factors, metabolic and cellular mediators. Predominantly, these lesions present with prostaglandins (PGs), interleukin-1 (IL-1), Il-3, IL-4, IL-6, interferon (IFN), tumor necrosis factor-alpha (TNF-a), and transforming growth factor-alpha (TGF-a) and chemokines - RANTES, IP-10, and MCP-1as chemical mediators for epithelial proliferation.10 In the second phase, a cavity is formed, lined by epithelium and in the third phase, the cystic growth due to osmosis is evident. This cystic growth and expansion occur due to the release of histamine, hydrolytic enzymes (matrix metalloproteinases) and bone-resorbing factors. In our present case, the traumatic incident with chronic inflammatory lesion at the periapical aspect of central incisors evoked a stimulation of epithelial rests of malassez. Continued activation of the inflammatory mediators had resulted in enlargement of the lesion to the present state.
On histopathological examination, a cystic lumen lined by epithelium is seen. The epithelium varies from the most common non-keratinized stratified squamous epithelium to varying degrees of columnar ciliated epithelium or muco-secretory cells (maxillary sinus or the nasal cavity). The cystic wall exhibits peculiar features of an abundant degree of inflammation (T-cells and B-cells), macrophages, Rushton bodies, cholesterol clefts, and an endothelial response. The present case matches this microscopic appearance. The uniqueness of the present case lies in the pathologist's opinion as to the separate enucleated tissues adjacent to the permanent maxillary right and left central incisors exhibits a similar histopathology picture.
Treatment of all odontogenic cysts include complete local surgical excision, decompression, marsupialization (large lesions, lesions close to vital structures) and finally extraction of the offending teeth. Also, over a 2-year follow up, no malignant transformation was noticed. In such lesions, patients and clinicians combined effort is needed for success of treatment.
CONCLUSION
The present case report demonstrates a radicular cyst invading the periapical region maxillary anterior teeth in a unique manner. The radio graphical appearance and a similar pathology picture of the two separate cysts adjacent to each other could be used as an interesting data due to its rarity. Although radicular cysts appear as common cystic lesions of the jaws, a sound knowledge of this atypical presentation of bilateral radical cyst should be at the back of the clinician mind to set apart the aggressiveness of this lesion. It is mandatory for all the pathologists to have an in depth knowledge about the lesion and also other lesions which have similar presentations, in order to correctly diagnose the lesion.
Acknowledgements: None Conflicts of interest
The author has no conflict of interest to declare.
Author Contributions:
1. Shanmugasundaram Karpagavalli: 25%
2. Sathasva Subramanian: 25%
3. Vedam Vaishnavi: 25%
4. Ganapathy Sivadas: 25%
REFERENCES
1. Toomarian L, Moshref M, Mirkarimi M, Lotfi A, Beheshti M. Radicular cyst associated with a primary first molar: A case report. J Dent (Tehran). 2011;8(4):213-217. [ Links ]
2. Cawson RA, Odell EW dan Porter S. Cawson's Essential of Oral Pathology and Oral Medicine 7th Ed. Edinburgh: Churchill Livingstone, 2002; 103-108. [ Links ]
3. Saquete R, Brasileiro BF, Rabello M. Radicular cyst in maxilla. Clinic surgical case report. 2009; 182-191. [ Links ]
4. Radicular and residual cysts. Mervyn Shear & Paul Speight. Cysts of the Oral and Maxillofacial Regions. Fourth edition Wiley-Blackwell Publishers 2007; 123 -142. [ Links ]
5. Pekiner, Filiz Namdar et al. "Clinical and radiological features of a large radicular cyst involving the entire maxillary sinus." Journal of Marmara University Institute of Health Sciences 2 (2012): 31-36. [ Links ]
6. Stuart C. White, Michael J. Pharoah. Oral Radiology Principles and Interpretation 8th edition Mosby Publishers 2019; 387-410. [ Links ]
7. Adel B, Kawthar S, Souha B. Extensive periapical cyst in the maxillary sinus 'a case report'. International dental journal of student's research: case report. 2012; 1:14-24. [ Links ]
8. Venkateshwar G, Girotra C, Mandlik G. Extensive radicular cyst of the mandible: a rare case report. International Journal of Medical Dentistry 2013; 1:7175. [ Links ]
9. Muglali M, Komerik N, Bulut E, Yarim GF, Celebi N, Sumer M. Cytokine and chemokine levels in radicular and residual cyst fluid. J Oral Pathol Med 2008; 37:185-9. [ Links ]
10. Hayashi M, Ohshima T, Ohshima M. Profiling of Radicular Cyst and Odontogenic Keratocyst Cytokine Production Suggests Common Growth Mechanisms. J Endod 2008; 34:14 -21. [ Links ]
 Correspondence:
Correspondence:
Dr.Vaishnavi Vedam
Senior Lecturer (Oral Pathology), Faculty of Dentistry, AIMST University
Malaysia Ph No: +60 1764 47 178 Email: vaishnavivedam@gmail.com














