Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.77 no.5 Johannesburg 2022
http://dx.doi.org/10.17159/2519-0105/2022/v77no5a2
RESEARCH
http://dx.doi.org/10.17159/2519-0105/2022/v77no5a2
The accessibility to oral health services in Lesotho's public health sector
M MokhethiI; CME McCrindleII
ISchool of Health Systems and Public Health, Faculty of Health Sciences, University of Pretoria, South Africa; ORCID: 00000001-9744-6321
IIProf) School of Health Systems and Public Health; Faculty of Health Sciences, University of Pretoria, South Africa; ORCID: 0000-0002-4756-8969
ABSTRACT
INTRODUCTION: Lesotho is a land-locked mountainous country in Southern Africa. Both geography and poverty impact on dental health in low-income patients. Information on the number and function of dentists and dental therapists in public hospitals, are lacking
AIMS AND OBJECTIVES: The aim was to investigate accessibility to oral health services. Objectives were to investigate the number and geographical distribution of oral health personnel and document the availability of dental services in Lesotho.
DESIGN: A cross-sectional mixed methods study design was used
METHODS: Four dental therapists of the six employed by the government, participated in in-depth interviews. Questionnaires about access to oral health services were administered to government employed dentists. The Lesotho National Department of Oral Health provided information regarding dental patient statistics between 2017 and 2019
RESULTS AND CONCLUSIONS: It was found that 20 dentists and 10 dental therapists provided limited dental services in public facilities. In 2017, 2018 and 2019; the annual numbers of dental patients were 85 776, 75 148 and 97 425 respectively. Approximately 40% of patients visited two hospitals in Maseru. It was concluded that there was a shortage of oral health personnel, resulting in inadequate access to dental services, particularly in rural areas.
Keywords: Lesotho, Southern Africa, Oral Health, Dentist, Dental Therapist, Public Health
INTRODUCTION
The small mountain kingdom of Lesotho is entirely landlocked by the Republic of South Africa. It was founded in the early 19th century by King Moshoeshoe I and today functions as a constitutional monarchy with King Letsie III serving as the ceremonial head of state1. Since obtaining its independence from Great Britain in 1966, the country has seen episodic bouts of political instability. It has undergone three coups d'etat in the years 1978, 1986 and 1994.1 In 2014, the country survived another attempted coup d'etat.2 More recently, Lesotho has had three elections in a 5-year period (2012, 2015 and 2017), with no one party winning an outright majority, so the past three governments have been coalition governments.3 From May 2020, the ruling coalition government was replaced by a different coalition, following the resignation of the Prime Minister making it a fourth different government in a nine -year period with elections set for 2022.3
According to the Lesotho Bureau of Statistics, as of 2016, the population is just over 2 million people.4 The National Dental Database, on the other hand, includes only 30 dentists5, which means that there is one dentist for every 66 666 people. In the neighbouring country, South Africa, the ratio is considerably more favourable at 1:8900.6 By comparison, the dentist to patient ratio in developed countries is 1 dentist for every 2000 people.7 The actual picture in Lesotho is much grimmer, as some of these dentists work as educators at the National Health Training College, while others are in managerial, non-clinical roles. In addition, all those private dental practices registered with the Lesotho Medical Dental and Pharmacy Council are located within a 10 km radius of one another in the capital city, Maseru. This means that the rural population in Lesotho is reliant on only 22 practising dentists; all of whom are employed directly or indirectly by the government.5 A map of this mountain kingdom indicates the inaccessibility of the rural population and this is exacerbated in winter, when many villages are snowbound (https://www.worldometers.info/img/maps_c/LT-map.gif).
Approximately 70% of the population resides in rural areas4, while all the dentists and other oral health personnel are stationed in the more urban areas, which poses the problem of patients having to move vast distances to access a treatment centre. The Lesotho Bureau of Statistics estimates that only 31.7 percent of the population live in urban areas; while 62.9 percent of urbanites reside in the capital, Maseru.4 This shortage of oral health personnel, coupled with the unequal distribution of the few dental personnel, has created a crisis that needs to be addressed urgently to meet the dental needs of the Basotho people, particularly those living in rural areas.
Previous studies have indicated that tooth loss was more prevalent in individuals of lower social classes and this pattern has persisted over a long period of time.8-9 In Lesotho, individuals who have a tertiary education have been shown to have a greater knowledge about oral health than those without a university qualification10; and are likelier to retain their natural teeth for longer.
Oral health is an important indicator of overall well-being and should begiven more attention.11 Dental caries in permanent teeth, has been estimated as the most common disease globally; affecting an average of 2.44 billion people in 2016.12 This is half a billion more people than the next most common disease, which is latent tuberculosis infection. Overall, the combination of diseases affecting the oral cavity, which range from dental caries, periodontitis and head and neck cancer; affect a staggering 3.58 billion people worldwide12, which was about half of the world's population in 2016.
Periodontitis, the second most common oral disease12 is also a major source of discomfort, pain and tooth loss. It not only affects the oral cavity, but is also linked with a number systemic complications.13 Periodontitis, like Type 2 diabetes mellitus, has chronic inflammation as the underlying pathophysiological mechanism; and studies have shown that the effective management of periodontitis plays a significant role in glycaemic control.14-16 Five percent of all the dental patients who were seen over the past year in Lesotho had some form of periodontal disease as their presenting complaint and dental extraction was also a common procedure.17
In Lesotho, it is common practise for dental assistants to carry out some of the clinical work and they all receive appropriate in service training for this.18 Lesotho also employs dental therapists to complement the oral health workforce.19 This practice is in line with several other Commonwealth countries.20 The literature reports that 33 members (Lesotho not included) of the 55 Commonwealth countries employ dental therapists.20 Dental therapists provide basic to intermediate level dental care at some hospitals and health centres in Lesotho.21 Studies in the UK reported that only 10% of the general population were familiar with dental therapists as distinct dental professionals, but none of them could correctly identify any of the procedures that fall within the scope of the dental therapist.22 Dental therapists have been practising in the UK since July 200223 .However, anecdotal reports in Lesotho suggest that they have been employed by the government since 1996.24 In the neighbouring country, South Africa, the need for mid-level dental workers in the form of dental therapists was first realised in 1975; and the government made provisions for their training at Ga-Rankuwa Hospital soon thereafter.25 The dental therapy programme was eventually offered as a distinct degree at Sefako Makgato Health Sciences University (Formerly Medunsa) 25.
The two most common oral diseases (dental caries and periodontitis) are to a large extent preventable, through relevant education and techniques, which can be provided by an oral health worker. The evidence in Lesotho suggests that despite the general knowledge of the public regarding oral health, patients only go to the dentist when there is a perceived need, usually when they experience dental pain18, although the cost of treatment in Lesotho is heavily subsidised by the government.19
As of 2016, the Government of Lesotho, through the National Health Training College (NHTC) has started training dental therapists in a 3-year post high school degree programme.26 This aimed at improving access to healthcare, especially among marginalised communities; in keeping with the principles of primary health care.
The Lesotho Medical, Dental and Pharmacy Council (LMDPC) was created by Order 13 of 1970 (Medical, Dental and Pharmacy Order of 1970) to regulate the practise of dental professionals.27 The Order, however, has not been updated since 1970 and does not make provision for mid-level health workers like dental therapists, who did not exist in Lesotho at the time the legislation was promulgated. The rationale of this study is therefore to investigate the number; and map out the geographical distribution; of oral health personnel in Lesotho and document the availability of dental services across the country.
METHODS
Study design
This was a cross-sectional mixed methods survey of oral health providers in Lesotho. It used descriptive statistics to analyse data. Data sources included a document review, observations, a thematic review of in-depth interviews; as well as categorical and numeric data obtained from questionnaires.
Study population and sample size
This study population consisted of 4 out of the 6 dental therapists who were employed by the Government of Lesotho and all (22) of the dentists who work in the public sector providing clinical services were invited to take part in an online questionnaire.
Data Collection
Semi-structured face to face, in-depth interviews related to the study were carried out with the dental therapists (n=4). Quantitative data were accessed from the Lesotho Ministry of Health, Oral Health Departmental records. Updated records of dental personnel employed by the government of Lesotho, as well as statistics of dental patient numbers and dental procedures carried out nationwide between 2017 and 2019, were also accessed. Data management and analysis
The data from the interviews were transcribed verbatim and thematic analysis was carried out.28 The Quantitative data were captured and analysed using Microsoft Excel (Microsoft Office 2016)
RESULTS
Qualitative data
The responses below encapsulate some of the themes that emerged during the in-depth interviews with the four dental therapists, who agreed to be interviewed:
Theme 1: Health centres very far, oral health services limited to the rural population
Interviewee 2: In terms of drive it's almost 3 hours' drive to Ketane, but the furthest facility is not accessible by road. I went using the helicopter from flying doctors and camped there for a week... even the nurses there say that we are neglecting them, you need a week to be there, when you arrive they mobilise the patients then you see the patients over 3 days or so, so it's not something that can be done more often.
Theme 2: Inadequate remuneration Interviewee 3: The remuneration is low as compared to the region if we're looking at other countries that are using the same currency, because Swaziland is offering M19 000 almost M20 000, also transport allowance
Theme 3: Lack of transport to facilities impairs the provision of oral health services Interviewee 4: I've realized that when you go with the vehicle for partners; sometimes they may also have their own priority area, they have their own activities that they may want to do with that same vehicle. So it will be the time factor, they'll drop you there where you're going to work; then the vehicle can go to another place. So if I'm having a specific vehicle for oral health I may go to an outreach, when I finish with oral health education screening and promotion, I can move on to a school within the same catchment area; so there is limitation of my activities. I'm very restricted because of the vehicle that I'm having. That's where I feel that we need our own vehicle.
Theme 4: Not much of a difference in the roles of dentists and dental therapists in Lesotho Interviewee 2: I desire to see a situation whereby each professional works hard towards their scope, so that it makes a difference. A dental therapist for example, isn't trained to do endodontics and prosthodontics and all; so we don't want the situation whereby a dentist spends his or her training doing extractions... Why should a dentist spend time doing extractions in the clinic, when the assistant is also trained in doing extractions. If we don't draw lines, we won't professionalise, let's draw lines.
Quantitative data
The number of dentists currently working in the public sector, was cross matched with the list of dentists registered with the Lesotho Medical Dental and Pharmacy Council. These 18 dentists represented 14 health facilities, out of a total of 22 hospitals in the country. These are the dentists employed, either directly or indirectly, by the government. They serve just over 2 million of the population in Lesotho. The number of dentists in the public sector; as well as the population served, per district, are shown in Table I.
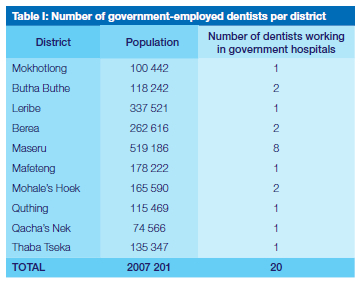
A retrospective analysis of the National dental patient records was done to determine the total number of dental patients seen per facility for 3 years between 2017 and 2019 (See Fig 1 above).
The two hospitals in Maseru, Queen Mamohato Memorial Hospital (QMMH) and Queen Elizabeth II; attended to the highest number of patients (17 636 and 20 076 respectively) in 2019. This accounted for 38.7% of all dental patients. Both hospitals are located in Maseru within a 7 km radius of each other. There are two additional dental hospitals in Maseru. These are St Joseph Hospital and Scott Hospital; both of which are operated by the Christian Health Association of Lesotho (CHAL).
The total number of dental patients seen in 2019 across all public hospitals was 97 425; a nearly 30% increase from the previous year. Some hospitals (Mount Tabor, St. Joseph and Tebellong) did not treat any dental patients, during periods when no oral health personnel were employed. The total number of oral cancer patients seen in 2019, is shown in Table II.
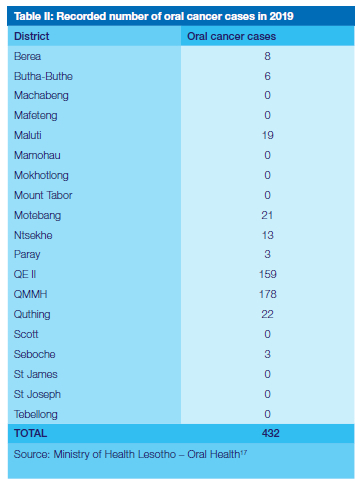
In 2019, a total of 432 cases of orofacial cancer were reported, 78% of whom were seen at QMMH and Queen Elizabeth II in Maseru. This number however does not only represent new diagnoses, but also repeat patients. The same patient could have been counted multiple times, with each visit to a dental facility. Thus, using the current data collection tools; it is not possible to determine the number of new diagnoses each year. The current data collection tools also do not allow for the determination of the cases of Oral Squamous Cell Carcinoma (OSCC) case fatality rate in Lesotho. There are currently no oncology services in Lesotho; so every suspected cancer patient is referred to the tertiary hospital, QMMH, where a biopsy will be taken for confirmation and positive cases would be to Bloemfontein, across the border in South Africa, for oncology treatment. The dentists interviewed, were also presented with a list of dental procedures/services; then asked to report which of the services they offered at their respective facilities (See Table III)
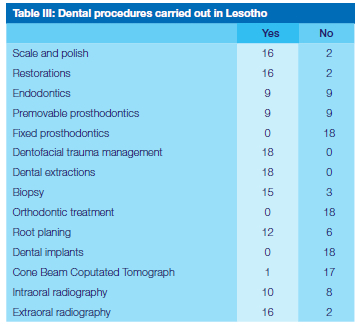
Table III shows the dental procedures carried out by dentists working in government hospitals. These ranged from 0% for some specialist services like orthodontics to 100% for dental extractions.
DISCUSSION
Data analysis showed the perceived shortage of oral health personnel, particularly dental therapists, in the public sector of Lesotho. Due to the mountainous terrain in Lesotho, the lack of infrastructure, many rural settlements and the low socioeconomic status of most the population; dental therapists have become an indispensable part of the oral health team in Lesotho.
When the country entered into a public private partnership for the building and running of the new referral hospital, QMMH, the agreement was also for Tsepong (Pty) Ltd to build/refurbish four filter clinics to decrease the number of patients who would go directly to the hospital.29 These would serve as primary care facilities. Tsepong also recruited and employed all staff required for the filter clinics and the hospital. Unlike the health centres run by the government, where dental and other health services have always been free; these filter clinics would charge a subsidised dental fee; similar to fees charged at all the other hospitals. The four filter clinics each have a dental clinic, staffed by a dental therapist and dental assistant, and, like the main hospital, have a cap on the number of dental patients seen daily. Data on patients seen at the clinics were added to that of QMMH and recorded as a total; which meant the hospital itself actually saw far fewer patients than the Maseru district hospital, Queen Elizabeth II hospital (see Fig 1).
Since government employed dental therapists have to go out into the community to provide oral health services, there is a need for reliable daily transport provision. Ideally, the task of ensuring that there are adequate transport services for dental therapists to carry out work in the community belongs to the state. Dental therapists reported that the government is frequently unable to meet this demand for transport services. As a result, rural communities suffer, because visits by the dental therapists are rare. This is problematic, as it limits both the number and the duration of visits to the rural mountainous areas in Lesotho, where dental therapists; rather that dentists, provide dental services. Dental therapists often have to rely on transport facilities provided non-governmental organisations (NGOs) in their respective districts.
These NGOs include: Solidarmed, Riders for Health, Partners in Health (PIH), Baylor International Paediatric AIDS Initiative (BIPAI), Elizabeth Glaser Paediatric AIDS Foundation (EGPAF), World Vision and University Research Council (URC). They also assist oral health departments in various districts with resources such as toothbrushes and toothpaste. These resources are also given to the community during oral health activities; especially during the oral health awareness (campaign) week, held once a year across Lesotho. Each of the NGOs have their own specific mandate, especially dealing with HIV/AIDS; so oral health services tend to feature lower down on their list of priorities. Dental therapists interviewed reported that their current salaries in the government are lower than what they would deem to be adequate. Respondents have practised in Lesotho for between two and 10 years.
The entry level pay grade for a dental therapist in Lesotho is Grade F, which is similar to other similarly qualified cadres; such as laboratory technicians and pharmacy technicians. This is the entry level salary grade for the most junior degree holders in the government. Research with dental therapists in South Africa, also showed that they regarded inadequate remuneration as one of the main reasons impacting their level of job satisfaction.30 However, due to their lower cost of training and the scope of primary dental procedures that they can carry out, dental therapists remain affordable and widely accepted as part of the oral health team in many other countries.20 The array of dental procedures offered to the citizens of Lesotho (Table III) is also only a portion of the total number of procedures that could be made available, if the Ministry of Health decided to provide more comprehensive dental health care. There are two forms of treatment, which are offered by all dentists who took part in the questionnaire, were dental extractions and the management of orofacial trauma. Dentists in Lesotho carry out basic extractions, scaling and polishing as well as restorations. All these procedures, which encompass the vast majority of dental procedures, also fall within the scope of dental therapists.21 It would perhaps be more sensible to shift almost all of these procedures to dental therapists, while specifying the schedule of medications they are allowed to prescribe. Dentists, although they can perform all those routine procedures; should be involved more in the fields of endodontics; fixed and removable prosthodontics; taking and interpreting radiographs; root planing and some forms of periodontal surgery, among others. These functions could be prescribed; under regulations pertaining to National Legislation.
None of the dentists surveyed mentioned that they performed any services in the fields of fixed prosthodontics, orthodontics or implantology. This is not surprising, given that there are no clinical dental specialists in the country; except for one oral and maxillofacial surgeon at the referral hospital, QMMH, in Maseru. There is a similar debate in South Africa as to whether dentists are perhaps overqualified to be doing basic extractions; when they could actually be doing more specialised work.31 Four hospitals in Lesotho have dental laboratories; which would enable them to carry out removable prosthodontics.17
In 2019, it was observed that only QMMH seemed to be providing this service (according to official records), perhaps due to their more efficient procurement processes, which ensure that they are never out of stock with regards to dental supplies. In 2016, the National Oral Health Office made available to all dentists, a standardised document of dental consumables. According to email records, the national office has been procuring some dental consumables at a central level and distributing them to different facilities.
Previous studies conducted on the utilisation of dental services reported that 16% of the population made use of dental services with a range of 4.7%-40.9%.32 Given that a total of 97 425 patients attended dental facilities in Lesotho in 2019 (Fig 1), it means that less than 5% of the population made use of dental facilities, only a fraction of the global average. This excludes the relatively smaller number of individuals who accessed dental services from the handful of dentists practising privately in Maseru. It also excludes patients seen by dental therapists at the primary level, whose data are not recorded in the same way that other dental hospitals record their patients. They are classified purely as community dentistry / outreach patients, despite some of the clinical work that is done on oral health. The majority of oral health personnel in Lesotho are employed by the government, followed by CHAL, and are located at each of the district and CHAL hospitals. In the neighbouring South Africa however, 90% of dentists work in the private sector, which caters for only 16 percent of the population.31
It was also noted during this research, that there were no active oral cancer screening programmes. This may lead to a late diagnosis of oral cancer, which in turn may result in an increasingly poor prognosis. This problem could be alleviated; if there were enough primary healthcare workers to provide education and basic screening for potentially malignant lesions, particularly in the oral cavity. Given the current oral health staff complement, it is not possible to effectively educate and screen the optimal number of individuals for oral cancer, which could be a probable reason why potentially malignant lesions in the oral cavity are not picked up as early enough to prevent mortality
CONCLUSIONS
Lesotho is in dire need of more oral health personnel and dental clinics / hospitals. The highest need is in the form of dental therapists whose scope of practise includes going into the community to provide primary oral care services to the most rural and destitute inhabitants of Lesotho. The fact that some dentists have to see a few thousand patients every year and dental therapists on occasion have to trek 3-5 hours to reach some low-income rural areas high in the mountains; shows the importance of having more oral health personnel. Focus should be shifted towards preventive dentistry, in order to decrease the rate of dental extractions. These issues need to be addressed at a policy level, to ensure that oral health services reach all the people of Lesotho. It is disconcerting that more than 40 years after the Alma Ata Declaration, the maxim 'health for all' is still a long way from being achieved in Lesotho.
ETHICS
Ethical approval for this research was given by the Ethics Committee of the Faculty of Health Sciences at the University of Pretoria
Conflict of interest declaration
None
Acknowledgements
The authors wish to thank the National Research Foundation (NRF) for their financial support towards the cost of this study
Author contributions:
1. Maluke Mokhethi: 60%
2. Cheryl M E McCrindle: 40%
REFERENCES
1. Shale I [Internet] Update: The law and legal research in lesotho. 2014 [cited 2019 July 24]. Available from: https://www.nyulawglobal.org/globalex/Lesotho1.html. [ Links ]
2. Reuters [Internet] Lesotho pm says army staged coup, flees to south africa. 2014 [cited 2020 June 16]. Available from: https://www.reuters.com/article/us-lesotho-coup/lesotho-pm-says-army-staged-coup-flees-to-south-africa-idUSKBN0GU04U20140830. [ Links ]
3. Fogelman C [Internet] It's the end of an era in lesotho. Mail & Guardian; 2020 [cited 2020 June 18]. Available from: https://mg.co.za/africa/2020-05-13-its-the-end-of-an-era-in-lesotho/. [ Links ]
4. Lesotho Government. Census 2016. In: Bureau of Statistics. Maseru: Government Printing; 2016. [ Links ]
5. LMDPC. Lesotho medical dental and pharmacy council statistics [Unpublished]. 2019. [ Links ]
6. Bhayat A, Chikte U. The changing demographic profile of dentists and dental specialists in south africa: 20022015. International Dental Journal. 2018; 68(2):91-6. [ Links ]
7. WHO [Internet] Oral health services. 2019 [cited 2019 15 June]. Available from: https://www.who.int/oral_health/action/services/en/. [ Links ]
8. Bernabé E, Sheiham A. Tooth loss in the united kingdom-trends in social inequalities: An age-period-and-cohort analysis. Plos one. 2014; 9(8):e104808. [ Links ]
9. McGrath C, Bedi R. Severe tooth loss among uk adults-who goes for oral rehabilitation? Journal of oral rehabilitation. 2002; 29(3):240-4. [ Links ]
10. Mndzebele SL, Kalambay JM. The influence of oral health knowledge and perceptions on dental care behaviours amongst adults attending treatment at berea hospital, lesotho : Dental public health. African Journal for Physical Health Education, Recreation and Dance. 2014; 20(sup-1):385-95. [ Links ]
11. Sheiham A. Oral health, general health and quality of life. SciELO Public Health; 2005. [ Links ]
12. Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the global burden of disease study 2016. The Lancet. 2017; 390(10100):1211-59. [ Links ]
13. Linden GJ, Lyons A, Scannapieco FA. Periodontal systemic associations: Review of the evidence. Journal of periodontology. 2013; 84:S8-S19. [ Links ]
14. D'Aiuto F, Gkranias N, Bhowruth D, Khan T, Orlandi M, Suvan J, et al. Systemic effects of periodontitis treatment in patients with type 2 diabetes: A 12 month, single-centre, investigator-masked, randomised trial. The Lancet Diabetes & Endocrinology. 2018; 6(12):954-65. [ Links ]
15. Correa FO, Gongalves D, Figueredo CM, Bastos AS, Gustafsson A, Orrico SR. Effect of periodontal treatment on metabolic control, systemic inflammation and cytokines in patients with type 2 diabetes. Journal of clinical periodontology. 2010; 37(1):53-8. [ Links ]
16. Tsai C, Hayes C, Taylor GW. Glycemic control of type 2 diabetes and severe periodontal disease in the us adult population. Community dentistry and oral epidemiology. 2002; 30(3):182-92. [ Links ]
17. Kalambay J. Lesotho oral health statistics [Unpublished]. 2019. [ Links ]
18. Linjewile-Marealle N. Factors influencing utilization of oral health services in lesotho [Unpublished]. University of Western Cape: University of Western Cape; 2017. [ Links ]
19. Lesotho Go. Annual joint review 2017-18. In: Health Mo, editor. Maseru2018. [ Links ]
20. Nash DA, Friedman JW, Mathu-Muju KR, Robinson PG, Satur J, Moffat S, et al. A review of the global literature on dental therapists. Community Dentistry and Oral Epidemiology. 2014; 42(1):1-10. [ Links ]
21. PublicService. Dental therapist scope of practise [Unpublished]. Public Service Commission; 2017. [ Links ]
22. Dyer T, Robinson P. Public awareness and social acceptability of dental therapists. International journal of dental hygiene. 2009; 7(2):108-14. [ Links ]
23. Ward P. The changing skill mix-experiences on the introduction of the dental therapist into general dental practice. British dental journal. 2006; 200(4):193. [ Links ]
24. Morojele D. First dental therapists in lesotho. 2019. [ Links ]
25. SMHSU [Internet] Oral health sciences. 2019 [cited 2019 July 29]. Available from: https://www.smu.ac.za/schools/oral-health-sciences/. [ Links ]
26. NHTC. National health strategic plan 2017-2022. In: Health Mo, editor. 2016. [ Links ]
27. NationalAssembly [Internet] Legal document: The medical, dental and pharmacy order 1970. 1970 [cited 2019 July 28]. Available from: https://www.lesothotradeportal.org.ls/index.php?r=site/display&id=48. [ Links ]
28. Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: Striving to meet the trustworthiness criteria. International journal of qualitative methods. 2017; 16(1):1609406917733847. [ Links ]
29. Webster PC. Lesotho's controversial public-private partnership project. The Lancet. 2015; 386(10007):1929-31. [ Links ]
30. Singh PK. Job satisfaction among dental therapists in south africa. J Public Health Dent. 2014; 74(1):28-33. [ Links ]
31. Bhayat A, Chikte U. Human resources for oral health care in south africa: A 2018 update. Int J Environ Res Public Health. 2019; 16(10):1668. [ Links ]
32. Bhandari B, Newton JT, Bernabé E. Income inequality and use of dental services in 66 countries. Journal of dental research. 2015; 94(8):1048-54 [ Links ]
 Correspondence:
Correspondence:
Cheryl M E McCrindle
Faculty of Health Sciences, University of Pretoria, South Africa
Tel: 27 12 356 3272; Email: cheryl.mccrindle@up.ac.za. / cheryl.mccrindle@gmail.com














