Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.77 no.5 Johannesburg 2022
http://dx.doi.org/10.17159/2519-0105/2022/v77no5a5
REVIEW
http://dx.doi.org/10.17159/2519-0105/2022/v77no5a5
The Role of Community Health Workers in Oral Health Promotion and the Impact of their services in Sub-Saharan Africa: A Systematic Review
MA KhanI; BO OkeahII; EL MbivnjoIII; E KisangalaIV; AW PritchardV
IMohammed Azhar Khan: Unit B, 10 Barnard Road, Sherwood, Durban 4091, South Africa; Orcid": https://orcid.org/0000-0003-1812-8611
IIBernard Ojiambo Okeah: School of Medical & Health Sciences, Bangor University, LL57 2DG, Bangor, Gwynedd, Orcid: 0000-00022797-3377
IIIEtheldreda Leinyuy Mbivnjo: Biaka University Institute of Buea, Address: P.O. Box 77 Buea, Cameroon; Orcid ID: 0000-0002-26405693
IVEphraim Kisangala: Health Service and Population Research Department, Institute of Psychiatry, Psychology & Neuroscience, King's College London, UK, Orcid: 0000-00028466-8723
VAaron Wyn Pritchard: School of Medical & Health Sciences, Bangor University, Address: LL57 2EF Gwynedd, United Kingdom; Orcid ID: 0000-0003-4000-7170
ABSTRACT
Oral ailments are largely preventable but remain a significant public health concern afflicting nearly half the global population. These conditions account for 220 years of life lost per 100,000 people and about US$500 billion in health-related expenditures. Sub-Saharan Africa bears a significant burden of oral health problems thus exerting additional pressure on the scarce human resources for health. Community healthcare workers (CHWs) could be potentially utilised to bridge the shortage of oral health professionals in sub-Saharan Africa, hence, this systematic review that seeks to explore their current roles in oral health and potential impact on general physical health. This review follows the PRISMA guidelines and databases searched include PubMed, Web of Science, Medline, and CINAHL published between January 2010 and December 2019. Nine studies met the study eligibility criteria. The authors of this review established that CHWs perform variable roles cutting across primary, secondary, and tertiary prevention including providing oral hygiene education, recognising common pathologies, and treating oral lesions, administration of tooth extractions, dental pain management, and referral for advanced care. Although this could potentially improve oral health, our review did not establish the extent of the specific Impact on general physical health of patients and the burden of oral condition.
INTRODUCTION
"Oral health is multifaceted and includes the ability to speak, smile, smell, taste, touch, chew, swallow, convey a range of emotions through facial expressions with confidence and without pain, discomfort, and disease of the craniofacial complex1". Oral health is an important aspect of an individual's life, influencing general health/well-being, psychological, physiological and social functioning 1. Oral health is dynamic (subject to changes in an individual's expectations, perceptions, experiences and adaptability to conditions) and occurs along a continuum that is subject to the attitudes and values of individuals and communities 1.
Many diseases associated with poor oral health, like tooth decay (caries), are largely preventable; yet remain the most prevalent conditions affecting about half of the global human population 2. Oral diseases are also responsible for the loss of more than 220 healthy life years per 100,000 people 3. In addition, it is estimated that more than US $500 billion was spent globally on managing oral diseases in 2015 4. This amount of money represents a significant strain on the rural populations living where the greatest burden of oral diseases exists and the resource envelope is thin 2,5. In rural Sub Saharan Africa (SSA), the population experiences significant barriers that threaten the promotion of oral health 67.
These include scarcity of healthcare professionals with knowledge and skills in oral health 6, long distances to and high costs of accessing oral health services 6, ignorance of oral care 8 and unhealthy cultural practices and beliefs 9.
There is therefore a need for community-led public health intervention such as the use of community health workers (CHWs) that utilises a preventative approach to tackle the problem. There has also been advocacy for training of CHWs to increase the coverage of oral health programs and address the shortage of trained oral health professionals available to work at the community level10. The implementation of CHWs program can provide a triple benefit to the society including prevention of diseases, promotion of good health practices and basic curative services to the members of the community 11. The prospect of early identification and referral of HIV-related oral lesions in cHw led programmes could be key to determining antiretroviral treatment failure 12. The new framework for oral health definition emphasises access to care as a determining factor and highlights the moderating effect of cultural factors on an individual's self-evaluation of their oral health 1. Also, CHWs have been shown to improve the provision of culturally competent healthcare services1 and access to healthcare14. Considering the above, we conducted a systematic review of the literature to explore the roles of CHWs in promoting oral health in SSA and the effectiveness of their interventions.
OBJECTIVES
1. To assess the roles of CHWs in oral health in SSA.
2. To determine the impact of oral health services provided by CHWs.
METHODOLOGY
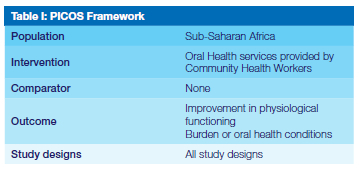
This systematic review was conducted in accordance with the PRISMA guidelines 15,16Electronic database searches were carried out to identify articles for review. The databases that were searched were PubMed, Web of Science, Medline, and CINAHL. MeSH search terms were used to complete the database searches and retrieved articles were assessed for eligibility using the PICOS (Population, Intervention, Comparator, Outcome, Study design) framework as outlined in Table I. The Medical Subject Heading (MeSH) terms were matched with phrases from the PICO framework in Table I and included in the search together with free text terms. MeSH terms are a library of medical headings that are used by the PubMed database to categorise research articles. Free text terms are synonyms, abbreviations and alternative spellings of the terms used in Table II. This list was compiled by the researchers and is displayed in Table II.
Updating searches
A database search to update results was carried out before the final analysis stage was completed. The initial database search took place in February 2020 while the final analysis of papers was completed in September 2020. An e-mail alert was set up with PubMed, Web of Science and Medline to ensure that the researchers are notified of new articles that would have shown up in the initial search.
A final search was run in December 2021 to ensure that relevant newly published articles are not missed from the review.
Managing references
Database search results were screened by title for inclusion independently by two researchers and stored electronically as an easier way to access articles electronically. The selected articles were exported to the researchers Mendeley account, checked for duplicated studies and stored for further screening.
Inclusion and exclusion criteria
Studies were assessed against the inclusion criteria namely language, population location, type of publication, year of publication, and country of study. Peer reviewed journal articles that were available in English, on study populations residing in SSA, and published between 2000 and 2019 were included. The inclusion and exclusion criteria are outlined in Table III.
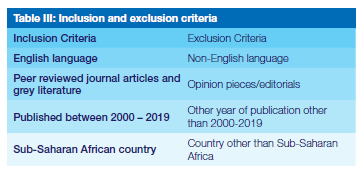
Abstract-only documents were not included in the systematic review as the details published in the full paper may differ from those in the abstract. There were no ongoing studies that matched all the other inclusion criteria found during the literature search.
Previous systematic reviews were excluded from this study to avoid replicating the findings of previous systematic reviews. Opinion pieces and editorials were also excluded from this systematic review. The study selection was reported using the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flowchart. PRISMA was developed to provide researchers with a transparent manner of reporting study selection16.
Data extraction
Data extraction was conducted to capture all necessary information from the studies identified from the selection process. The data extraction form was designed to record necessary information that relates to the topic and objectives of the study. This included the general identifying facts about an article such as the name of the researcher carrying out the data extraction, the date of data extraction, a code identifying the article, author name, article title, citation, type of publication, country where study was published/carried out and funding. Other details recorded during the data extraction process related to the characteristics of the study and population including aims and objectives of the study, study design, the inclusion and exclusion criteria, and comparators used. Furthermore, the form captured the setting of the intervention and any differences between the intervention and control groups.
Risk of bias (RoB)
The reviewers completed a risk of bias assessment using the corresponding RoB checklists produced by the US National Heart Lung and Blood Institute (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools). Only one study19 was of low quality; four studies were of moderate and the remaining four studies were of high quality. These are denoted in Table IV.
Analysis of findings
Subgroup analysis was based on the type of service provided (primary, secondary, tertiary preventive and curative or combination), and by programme aim/goal. The impact of CHWs services was assessed using the core elements of the novel definition for oral health care1 as improved physiological or psychological function or as a reduction in disease or condition status (severity). Disease reduction was measured as decrease in the burden (prevalence, incidence, morbidity/mortality) of any priority oral health condition: tooth decay and cavities (dental caries); gum (periodontal) diseases; oral cancers; noma; oral manifestations of HIV and AIDS; oro-facial trauma from accidents and violence; cleft lip and palate 17. An improvement in the oral health related quality of life was also used in measuring programme effectiveness 18.
RESULTS
Selection of studies
The PRISMA flow diagram in figure 1 outlies the process followed during the selection of studies for this review.
This review included nine studies from different countries namely Cameroon 19, 20, Gambia 21, South Africa 22-24, Kenya 12, Zimbabwe 25, and Uganda 26. The study designs used across the included studies varied and included case con-trol12, cross-sectional19,20,22,23, prospective observational21, experimental25,26, and qualitative24 study designs. Due to the diverse nature of the study designs, targeted population, settings, interventions, and outcomes, a meta-anal-ysis was excluded and results analysed through narrative synthesis.
Results synthesis
Various personnel providing oral health services across sub-Saharan African countries met the criteria for inclusion as community health workers. Based on studies conducted in Cameroon, Uganda, and South Africa, personnel providing oral health services at the community have been referred to as traditional healers 19, 20, 22,23,26,27. Additional titles used to refer to these personnel include community health workers in Kenya12, community oral health workers in Gambia21, caregivers22 and oral health promotion officers in South Africa 24. There was no standardised pre-service training for CHWs on oral healthcare, hence, they had diverse qualifications, training, and scope of their roles. A total population of 215 CHWs were involved across five studies 19,20,22,23,26 while the remainder of the studies did not specify the numbers of CHWs involved in provision of the oral health services 12, 21,24,25,27.
Training of CHWs
CHWs training and/ or level of education varied across the included studies with 77.8% of the interventions involving some formal training while 22.2% lacked a formal training component. The studies 12,19-22,24,25 with a training component prior to the CHWs performing their roles aimed at improving the knowledge and skills of CHWs in undertaking oral health interventions whereas the remaining studies 7, 11 only observed the behaviour, knowledge, and practices without a training intervention for the CHWs. Only four studies specified the training duration for the CHWs prior to their roles and this ranged from a day up to 90 days 21,22,25,26. The training for the CHWs was delivered through workshops that entailed focus group discussions, demonstrations including the use of pictorials, and role plays.
The largest (79.87%) improvement in the knowledge of CHWs on common health conditions was reported from a workshop training intervention involving traditional healers in Cameroon20. Improvement in CHWs knowledge on common oral conditions was also reported by a Kenya-based study that trained CHWs on recognizing oral lesions associated with HIV infection12 and a Uganda-based study whereby traditional healers participated in FGDs and workshops on false teeth "ebino" extractions 26 but this improvement was not specified in absolute proportions 12,26
Roles performed by CHWs in oral health.
The findings of this review indicate that CHWs perform a wide range of roles in oral health spanning across the three levels of disease prevention namely primary 23-26, secondary12,22,23 and tertiary prevention 19-21,23,27 as shown in Figure II and Table IV. The roles undertaken by CHWs generally include screening, diagnosing, treating common dental problems (e.g., oral candidiasis, dental caries, oral lesions, ulcers, Karposis Sarcoma, etc), pain management, atraumatic restorative treatment, teeth extractions, providing health education, basic oral hygiene services, and referring patients for advanced dental services.
Primary prevention
A Zimbabwe-based experimental study involved school teachers who were trained on prevention and treatment of dental caries and periodontal disease, dental fluorosis, and emergency tooth care at school with emphasis on plaque control through the use of the toothbrush and chewing stick in combination with fluoridated toothpaste 25. Subsequently, the trained teachers organized regional oral health workshops with 965 school children who were then followed-up in subsequent years to assess for plaque accumulation25Another study involved 46 traditional healers and 1874 local women in Uganda who participated in focus group discussions and an education session on extraction of false teeth "ebino"26. The causes, management, and alternatives to "ebino" extractions were also discussed through role plays, dialogues, and pictorials.
The third study involved ten health promotion officers in South Africa who went through a formal training session at Wits University on a revised health promotion curriculum before being subjected to qualitative telephone interviews 24. The revised training curriculum was aimed at integrating oral health literacy in the activities of health promoters in the Gauteng region of South Africa 24. A study based in South Africa assessed the knowledge, attitudes and practices of 83 traditional healers with regards to their oral health interventions 23. This was a multi-level prevention intervention that entailed primary, secondary, and tertiary prevention activities. The traditional healers provided health education to their patients on tooth brushing, diagnosed common oral conditions, and provided appropriate treatments using "muti" (traditional medicine). Furthermore, the traditional healers also referred the patients for advanced management for their oral conditions 23.
Secondary prevention
A case-control study based in Kenya involved CHWs trained on the recognition of oral lesions associated with HIV infection 12. In turn, the trained CHWs would undertake patient assessment within community settings based on the patient's histories and presenting complaints 12. Subsequently, the CHWs identified high-risk patients and referred them appropriately for further testing 12. Another study in South Africa also focussed on the oral manifestations of HIV infections where 32 traditional healers and 17 caregivers were part of a focus-group discussion on oral lesions22. The study participants completed a pre- and post-training survey on recognizing oral lesions associated with HIV based on A4-size photographs. In addition, the researchers also assessed the competence of the participants in oral hygiene (tooth brushing skills) 22.
Tertiary prevention
A cross-sectional study assessed the knowledge and practices of 21 traditional healers in north-west Cameroon following a training workshop on diagnosing, treating, and referring patients with common oral problems 20. A follow-up session after three months assessed the knowledge and practices of these traditional healers functioning as CHWs in diagnosing dental caries, oral candidiasis, aphthous ulcers, Kaposi's sarcoma, and oral cancers as well as the treatments they offered and the associated costs 20. Another study based in Cameroon examined the practices of 16 traditional healers regarding tooth extractions in a sample of 150 patients 19. The researchers observed the traditional healers while collecting herbs, applying on the patient's tooth, extracting the tooth, conducting observations post-tooth extraction, and providing post-op instructions 19. The traditional healers were then asked to complete a questionnaire on the anatomy of the tooth, post extraction instructions, management of complications and prevention of infection 19. The researchers also administered questionnaires to patients immediately after undergoing treatment 19. In Gambia, community oral health workers (COHWs) were trained for three months on atraumatic restorative treatment (ART) and supervised to provide the treatments 21. The ARTs were performed by groups of 10 COHW trainees, and patient outcomes after twelve months compared with ARTs performed by groups of 7 experienced COHWs or 2 dentists 21.
Impact of CHWs interventions
The researchers examined various outcomes to determine the impact of CHWs interventions in oral health. The specific outcomes across the studies included CHWs knowledge on common oral conditions, patients screened for oral ailments, patients referred, common oral conditions recognised by CHWs, oral health literacy, patients treated, pain management, patients with complications, preference for CHWs services, patients satisfied with CHWs services, and the burden of dental diseases. Table V summarises the key outcomes as reported across the included studies and these formed the basis for assessing the impact of the roles performed by CHWs in the oral health of the service users.
A study on the knowledge, diagnostic, and treatment practices of CHWs in Cameroon reported a 69% preference and 67.3% satisfaction with services offered by traditional healers due to ease of accessibility and low cost compared to conventional dental services 20. Similarly, 60% of patients preferred to have their teeth extracted by traditional healers in Cameroon with an estimated 93.3% patient satisfaction and only 4.7% of the patients reporting complications afterwards19. A Kenyan-based study reported an improvement in the number of patients screened for oral conditions as well as improved referral of patients for further testing12. Following two days training and focus group discussions, the proportion of oral lesions recognised by CHWs in South Africa based study involving traditional healers and caregivers increased by 22.4-71.4%. A Uganda-based study on management of false teeth by traditional healers and local women reported a reduction in hospital referrals for children with complications of false teeth extractions 26. The reduction in referrals in this study was desirable because the rampant "ebino" extractions contributed to a high number of admissions for complications from the procedures undertaken by traditional healers and local women 26.
A training intervention on ART reported no significant differences in ARTs performed by a group of 10 community oral health worker trainees and a comparative group of seven experienced community oral health workers. There was no significant difference in plaque accumulation amongst school children over four years after participating in an oral health workshop facilitated by school teachers in Zimbabwe compared to the control group 24. A knowledge and practices assessment for 83 traditional healers based in South Africa revealed that half of their clients presented with various complaints namely tooth aches, oral candidiasis, and swollen gums 22. Subsequently, 90% of them could correctly identify dental caries, gingivitis and oral candidiasis on A4 sized photographs while approximately 82% of the traditional healers referred their patients for advanced treatment in public health facilities 22. Following the intervention, the study reported an improvement in the recognition of oral lesions by traditional healers and an 84% improvement in the referral of patients for further specialised treatment 22.
DISCUSSION
Summary of evidence
Our review established that oral health services at community level in sub-Saharan Africa are provided by various groups of personnel namely traditional healers, health promotion officers, caregivers, or simply community healthcare workers. We categorised all the aforementioned personnel as CHWs in accordance with a recent systematic review that defined a CHW as a paraprofessional or lay person who understands the local culture, might have received some form of training and provides basic health services within their community 28.
Notably, we found no uniformity in the level of training, qualifications, experience, and the roles undertaken by the CHWs based on the included studies. In more than three quarters of the studies, persons undertaking the roles of CHWs in oral health had some form of training leading to their roles. The findings of this review further revealed that the roles undertaken by CHWs in oral health span across all the levels of disease prevention namely primary, secondary, and tertiary prevention.
The primary prevention roles performed by CHWs in oral health include providing oral health education on oral hygiene, tooth brushing skills, organising workshops to promote oral health literacy, managing false teeth. The secondary prevention roles performed by community healthcare workers in SSA countries include assessing patients' histories, screening, and recognising oral lesions and referring high-risk patients for further testing and/ or treatment. In tertiary prevention, the reviewed evidence shows that CHWs perform dental extractions, atraumatic restorative therapy under supervision, and providing pain relief for patients with dental problems. The CHWs also play a role in referring patients who require advanced dental interventions to dental specialists in the formal healthcare service. We also observed that CHWs could potentially play a role in promoting oral health literacy through health education which might have an influence on overall health outcomes 24 25.
The impact of the CHWs interventions were assessed using the key outcomes of included studies to determine whether there was an improvement in the physiological or psychological functioning of patients or a reduction in the burden and severity of oral conditions. According to the reviewed evidence, CHWs interventions appear to improve access to screening, diagnostic, and treatment services for oral conditions. However, due to the limited number of studies, we could not determine the lasting impact of these improvements on oral health or to what extent they influence the overall burden of oral conditions in the respective study settings. Improvements in the referral of patients for advanced management reported across two studies ranged between 62.5% and 84%. The researchers further observed that training of CHWs could potentially improve their diagnostic skills as reported in one study where CHWs recognised an additional 22.4-71.4% of oral lesions following a two-day training through focus group discussions 22.
We also observed a higher (60-69%) preference for CHWs services in comparison to the formal dental services and a resultant 67.3%-93.3% satisfaction for services provided by CHWs 19,20. The higher preference for CHWs services was motivated by their closer proximity within the community, the cost, and effectiveness of their services as perceived by the community members in comparison to the formal dental health service providers. The rate of complications reported from CHWs interventions appears to be low (4.7%) but this was only reported in one study where traditional healers performed tooth extractions 19. It is not clear based on the reviewed evidence to ascertain the impact of CHWs interventions on the severity of the oral conditions they managed or the physiological functioning of their patients.
Practice and research implications
The roles played by CHWs with respect to oral health and hygiene are considerably varied between countries and contexts. Their scope may include providing oral hygiene education, through to diagnosing common pathologies, and treating oral lesions. In some circumstances trained provision of tooth extractions, pain management, and referral for advanced care are functions of CHWs reported across included studies.
Such remit may have a significant impact on oral health and on the burden of oral conditions. Although we could not establish the extent to which these services impacted the general physical health of patients and the overall burden of diseases, scientific evidence shows that such services significantly improve people's overall quality of life 29, 30. Similarly, a study based in Brazil examined the effectiveness of a CHW program on oral health promotion and reported improvements in oral health knowledge, tooth-brushing practices, self-efficacy in oral hygiene, and utilisation of existing dental services 31. Despite this evidence, there is still need for more robust studies to better understand the specific impact of the oral health services provided by CHWs including on the physiological functioning of the service users as well as the overall burden of oral health conditions in SSA. It may also be worth exploring measures that could be applied to standardise the quality of oral health services provided by CHWs in SSA.
Considering the reviewed evidence, CHWs could provide a readily available pool of workers that can be capacitated to improve access to oral health services in resource limited settings. Our findings suggest that screening for oral conditions, diagnosis of common dental ailments, and basic treatment services for oral problems could potentially benefit from strengthening the services provided by CHWs. We observed an increase in the detection of oral lesions and referrals for advanced management following a training intervention for CHWs 12, 19, 22 but could not ascertain the statistical significance of these increases. This finding is consistent with recent evidence from a cross-sectional study based in India which revealed that trained CHWs were able to consistently diagnose oral lesions in comparison with an onsite specialist 32. Sub-Saharan African countries have acute shortages for healthcare workers including dental specialists 33. In some instances, populations travel long distances to access the limited dental services translating into huge out-of-pocket healthcare costs and wastage of time in search of essential services further exacerbating health inequalities. CHWs have already shown greater promise for bridging the chronic health human resources challenges based on their application across other services including provision of anti-retroviral treatments (ART) for HIV/AIDs, diabetes, and malaria interventions 34 35 and could be beneficial in providing oral health services.
The findings of our review show that there is considerable heterogeneity in terms of the role and function and expectation of CHWs with reference to oral healthcare provision. Current research evidences that in those contexts where CHWs are most comprehensively trained, they may be equipped with skills to perform essential dental procedures including tooth extractions, and simple pain relief (following a period of formal training and supportive supervision). We observed that CHWs were able to effectively provide atraumatic restorative therapy without complications for the service users following a three months training programme21. As such, capacity building the CHWs to provide quality oral health services could help overcome accessibility, affordability, and acceptability barriers to dental health services in impoverished and marginalised communities. This is further reinforced by a pilot study that demonstrated a higher acceptability for CHWs oral interventions amongst Chinese Americans 36. Our findings also revealed a higher preference for and satisfaction with CHWs services owing to their proximity within communities and affordability of their services. In certain communities, CHWs may be the only accessible healthcare provider, hence, an invaluable resource for bridging the disparities in oral health services by providing culturally competent oral health services 37.
Limitations
This review retrieved a small number of studies which were diverse in their study designs and settings. Consequently, the researchers could not ascertain the impact of CHWs interventions, and neither are the findings generalizable.
Author contributions:
1. Mohammed Azhar Khan: 20%
2. Bernard Ojiambo Okeah: 20%
3. Etheldreda Leinyuy Mbivnjo: 20%
4. Ephraim Kisangala: 20%
5. Aaron Wyn Pritchard: 20%
REFERENCES
1. Glick M, Williams DM, Kleinman D V., Vujicic M, Watt RG, Weyant RJ. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. Am J Orthod Dentofac Orthop. 2017 Feb;151(2):229-31. [ Links ]
2. WHO. Oral health [Internet]. World Health Organisation. 2018. Available from: https://www.who.int/health-topics/oral-health#tab=tab_1 [ Links ]
3. Marcenes W, Kassebaum NJ, Bernabé E, Flaxman A, Naghavi M, Lopez A, et al. Global burden of oral conditions in 1990-2010: A systematic analysis. J Dent Res. 2013;92(7):592-7. [ Links ]
4. Fonseca EP da. Oral Health Challenges: Global Burden of Disease as Information Resource for Policy-Making and Health Situation Analysis. Dent Case Rep. 2018 Feb;2(1). [ Links ]
5. Skillman SM, Doescher MP, Mouradian WE, Brunson DK. The challenge to delivering oral health services in rural America. Vol. 70, Journal of Public Health Dentistry. 2010. [ Links ]
6. Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Vol. 83, Bulletin of the World Health Organization. World Health Organization; 2005. p. 661-9. [ Links ]
7. Barnett T, Hoang H, Stuart J, Crocombe L. The relationship of primary care providers to dental practitioners in rural and remote Australia. BMC Health Serv Res. 2017 Aug 1;17(1):1-13. [ Links ]
8. Chhabra N, Chhabra A. Parental knowledge, attitudes and cultural beliefs regarding oral health and dental care of preschool children in an Indian population: A quantitative study. Eur Arch Paediatr Dent. 2012 Apr;13(2):76-82. [ Links ]
9. Swati J, Ashish S, Basavaraj P, Hansa K, Khushboo S, Shilpi S. Assessing the influence of culture on oral health-a review. J PEARLDENT. 2014 Jan;2:1-8. [ Links ]
10. Smit DA, Barrie RB, Louw AJ. The burden of dental caries in the Western Cape and a recommended turn-around strategy. S. Afr. dent. j. [Internet]. 2017 Sep [cited 2022 Apr 17] ; 72( 8 ): 360-365. Available from: http://www.scielo.org.za/scielo.php?script=sci_arttext&pid=S0011-85162017000800005&lng=en.http://dx.doi.org/10.17159/2519-0105/2017/v72no8a3 [ Links ]
11. Ministry of Health - Uganda. Ministry of health Community Health Extension Workers Strategy in Uganda. 2016. p. 64. [ Links ]
12. Koyio LN, Van der Sanden WJM, Van der Ven A, Mulder J, Creugers NHJ, Merkx MAW, et al. A community-based oral health promotion model for HIV patients in Nairobi, East District in Kenya: a study protocol. J Public health Res. 2013 Jun;2(1):5. [ Links ]
13. Handtke O, Schilgen B, Mósko M. Culturally competent healthcare - A scoping review of strategies implemented in healthcare organizations and a model of culturally competent healthcare provision. Todd CS, editor. PLoS One [Internet]. 2019 Jul [cited 2020 Feb 1];14(7):e0219971. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6667133/ [ Links ]
14. Perry HB, Zulliger R, Rogers MM. Community Health Workers in Low-, Middle-, and High-Income Countries: An Overview of Their History, Recent Evolution, and Current Effectiveness Keywords. Annu Rev Public Heal. 2014;35:399-421. [ Links ]
15. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev [Internet]. 2015 Dec 1 [cited 2019 Jul 24];4(1):1. Available from: https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/2046-4053-4-1 [ Links ]
16. Liberati A, Altman DDG, Tetzlaff J, Mulrow C, Gotzsche PC, loannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions. PLoS Med [Internet]. 2009 Jul 21 [cited 2019 Jul 11];6(7):e1000100. Available from: https://insights.ovid.com/bmj/bmjd/2009/07/250/prisma-statement-reporting-systematic-reviews-meta/24/00002591 [ Links ]
17. WHO Regional Office for Africa. World Health Organization. Int Organ [Internet]. 1960;14(1):212-4. Available from: https://www.afro.who.int/ [ Links ]
18. Baiju R, Peter E, Varghese N, Sivaram R. Oral health and quality of life: Current concepts. J Clin Diagnostic Res. 2017 Jun 1;11(6):ZE21-6. [ Links ]
19. Agbor AM, Naidoo S, Mbia AM. The role of traditional healers in tooth extractions in Lekie Division, Cameroon. J Ethnobiol Ethnomed. 2011 May 30;7. [ Links ]
20. Agbor AM, Naidoo S. Knowledge and practice of traditional healers in oral health in the Bui Division, Cameroon. J Ethnobiol Ethnomed. 2011 Jan 15;7. [ Links ]
21. Jordan RA, Gaengler P, Markovic L, Zimmer S. Performance of Atraumatic Restorative Treatment (ART) depending on operator-experience. J Public Health Dent. 2010 Jun;70(3):176-80. [ Links ]
22. Rudolph MJ, Ogunbodede EO, Mistry M. Management of the oral manifestations of HIV/AIDS by traditional healers and care givers. Curationis [Internet]. 2007 [cited 2020 Oct 6];30(1):56-61. Available from: http://curationis.org.za/index.php/curationis/article/view/1051 [ Links ]
23. Lewis HA, Rudolph MJ, Mistry M, Monyatsi V, Marambana T, Ramela P. Oral health knowledge and original practices of African traditional healers in Zonkizizwe and Dube, South Africa. SADJ [Internet]. 2004 [cited 2020 Oct 31];59(6). Available from: https://europepmc.org/article/med/15457910 [ Links ]
24. Molete MP, Daly B, Hlungwani TM. Oral health promotion in Gauteng: A qualitative study. Glob Health Promot [Internet]. 2013 [cited 2020 Oct 6];20(1):50-8. Available from: http://www.sagepub.co.uk/journalsPermissions.navDOI:10.1177/1757975913476906http://ped.sagepub.com [ Links ]
25. Frencken JE, Borsum-Andersson K, Makoni F, Moyana F, Mwashaenyi S, Mulder J. Effectiveness of an oral health education programme in primary schools in Zimbabwe after 3.5 years. Community Dent Oral Epidemiol. 2001;29(4):253-9. [ Links ]
26. Jamieson L. Using qualitative methodology to elucidate themes for a traditional tooth gauging education tool for use in a remote Ugandan community. Health Educ Res [Internet]. 2006 [cited 2020 Oct 6];21(4):477-87. Available from: https://academic.oup.com/her/article/21/4/477/573165 [ Links ]
27. Braimoh OB, Umanah AU. Basic package of oral care: a veritable tool for promotion of primary oral health care by community health officers. Odontostomatol Trop [Internet]. 2014 [cited 2020 Oct 6];37(147):51-6. Available from: https://europepmc.org/article/med/25975068 [ Links ]
28. Olaniran A, Smith H, Unkels R, Bar-Zeev S, van den Broek N. Who is a community health worker? - A systematic review of definitions. Vol. 10, Global Health Action. Co-Action Publishing; 2017. [ Links ]
29. Svensson L, Hakeberg M, Wide U. Dental pain and oral health-related quality of life in individuals with severe dental anxiety. Acta Odontol Scand [Internet]. 2018 Aug 18 [cited 2021 Feb 11];76(6):401-6. Available from: https://www.tandfonline.com/doi/full/10.1080700016357.2018.1473892 [ Links ]
30. Tjakkes GHE, Reinders JJ, Tenvergert EM, Stegenga B. TMD pain: The effect on health related quality of life and the influence of pain duration. Health Qual Life Outcomes [Internet]. 2010 May 2 [cited 2021 Feb 11];8(1):1-8. Available from: https://link.springer.com/articles/10.1186/1477-7525-8-46 [ Links ]
31. Frazão P, Marques D. Effectiveness of a community health worker program on oral health promotion. Rev Saude Publica. 2009;43(3):463-71. [ Links ]
32. Birur Np, Gurushanth K, Patrick S, Sunny S, Raghavan S, Gurudath S, et al. Role of community health worker in a mobile health program for early detection of oral cancer. Indian J Cancer [Internet]. 2019 Apr 1 [cited 2021 Feb 11];56(2):107-13. Available from: http://www.indianjcancer.com/text.asp?2019/56/2/107/257547 [ Links ]
33. Willcox ML, Peersman W, Daou P, Diakité C, Bajunirwe F, Mubangizi V, et al. Human resources for primary health care in sub-Saharan Africa: Progress or stagnation? [Internet]. Vol. 13, Human Resources for Health. BioMed Central Ltd.; 2015 [cited 2021 Feb 11]. p. 76. Available from: http://human-resources-health.biomedcentral.com/articles/10.1186/s12960-015-0073-8 [ Links ]
34. Hermann K, Van Damme W, Pariyo GW, Schouten E, Assefa Y, Cirera A, et al. Community health workers for ART in sub-Saharan Africa: Learning from experience - Capitalizing on new opportunities [Internet]. Vol. 7, Human Resources for Health. BioMed Central Ltd.; 2009 [cited 2021 Feb 11]. p. 1-11. Available from: https://link.springer.com/articles/10.1186/1478-4491-7-31 [ Links ]
35. Kisia J, Nelima F, Otieno DO, Kiilu K, Emmanuel W, Sohani S, et al. Factors associated with utilization of community health workers in improving access to malaria treatment among children in Kenya. Malar J [Internet]. 2012 Dec 30 [cited 2021 Feb 11];11(1):248. Available from: https://malariajournal.biomedcentral.com/articles/10.1186/1475-2875-11-248 [ Links ]
36. Northridge ME, Wu Y, Troxel AB, Min D, Liu R, Liang LJ, et al. Acceptability of a community health worker intervention to improve the oral health of older Chinese Americans: A pilot study. Gerodontology [Internet]. 2020 Dec 27 [cited 2021 Feb 11];ger. 12522. Available from: https://onlinelibrary.wiley.com/doi/10.1111/ger.12522 [ Links ]
37. Mobula LM, Okoye MT, Ebony Boulware L, Carson KA, Marsteller JA, Cooper LA. Cultural competence and perceptions of community health workers' effectiveness for reducing health care disparities. J Prim Care Community Heal [Internet]. 2015 Jan 1 [cited 2021 Feb 11];6(1):10-5. Available from: http://journals.sagepub.com/doi/10.1177/2150131914540917 [ Links ]
 Correspondence:
Correspondence:
Mohammed Azhar Khan
Dr. M A Khan Dental Practice
Address: Unit B, 10 Barnard Road, Sherwood, Durban 4091, South Africa
Email: mazhar015@gmail.com














