Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.77 no.4 Johannesburg Mai. 2022
RESEARCH
The prevalence and classification of mandibular third molar impactions and associated second molar pathology in a Gauteng population group. A retrospective study.
LM SykesI; TC PostmaII; L DawsonIII
IBSc, BDS, MDent, IRENSA, Dip Forensic Path, Dip ESMEA; Head of Department of Prosthodontics, Unversity of Pretoria. ORCID Number: 0000-0002-2002-6238
IIMChD, DHSM, PhD, Head Clinical Unit, Department of Dental Management Sciences
IIIBChD, Dip Oral Surgery., Department of Prosthodontics, University of Pretoria
INTRODUCTION
An impacted tooth is one that has not erupted or is unlikely to erupt into its functional position within the dental arch1, and which has remained embedded in the jawbone or mucosa for more than 2 years following its physiological eruption time2. It may be visible, not visible but palpable, or neither visible nor palpable but evident on a radiograph.1,3 Third molars are the most commonly impacted teeth followed by maxillary canines, with reported variations in prevalence amongst different population groups2,4' In 2000 The National Institute for Health and Clinical Excellence (NICE) issued guidelines stating that third molars should only be removed if there is evidence of pathology, and advocated that the practice of prophylactic removal be discontinued.1
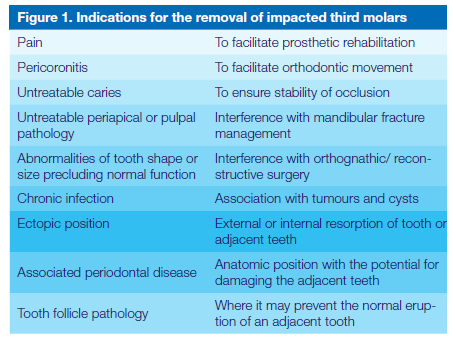
In 2007 The American Association of Oral and Maxillofacial Surgeons (AAOMS) published guidelines where extraction of third molars may be warranted as indicated in Figure 15.
In 2011 the AAOMS issued a position paper on third molar management that stated, "Predicated on the best evidence-based data, third molar teeth that are associated with disease, or are at high risk of developing disease, should be surgically managed. In the absence of disease or significant risk of disease, active clinical and radiographic surveillance is indicated"6. Based on this, all patients should be evaluated by an expert for third molar management and their problems assessed over time before any extractions take place.7 The South African Society of Maxillo-Facial and Oral Surgeons (SASMFOS), supported the AAOMS policy statement that "surgical management of impacted and erupted third molar teeth, even if asymptomatic, should only be carried out in the presence of and / or potential for pathology related to / or caused by the these teeth.8
Despite these recommendations, there is still controversy in the literature related to this issue and the practice has continued.
Literature review
The dental health of the population has improved in many countries resulting in a reduced incidence of early loss of first molars. This loss previously resulted in the second molars drifting forwards thus creating space for eruption of the third molars. With retention of the first molars, many patients now have insufficient space in their arches, which may contribute to higher levels of impacted 8's1,6.
There is no general consensus in the literature regarding prophylactic removal of impacted third molars. On the one hand the SASMFOS, AAOMS and JCDA (Journal of the Canadian Dental Association) recommend early removal of all third molars during adolescence, before completion of root formation. It was suggested that this may result in less postoperative complications and morbidity than that seen in patients who had extractions after the age of 25. 9,10 However, others are opposed to this as one of the most common complications of impacted third mandibular molar removal is injury to the inferior alveolar nerve bundle (IANB) which has resulted in countless medico legal issues against the dentists.11-13
The standard diagnostic preoperative assessment tool for the risk of IANB injury is a panoramic radiograph or the more modern cone-beam computed tomography (CBCT).11,14
Monaco et al. suggested that in those cases where the roots were close to the IANB, neurologic complications could be avoided or reduced by performing a coronectomy procedure. They advocated that this would result in minimal postoperative complications of which most were migrated root rests.15-17
Coronectomy was first proposed in 1984 by Ecuyer and Debien to decrease the risk of nerve damage in cases with IMTM roots in close proximity to the mandibular canal. Monaco et al. did a follow up study in 2019 regarding the success rate of coronectomy in IMTM cases with close relations to IANC and concluded : "no cases of neurologic lesions, a low rate of immediate postoperative complications, and no cases of late infection of the retained roots from the third to fifth year of follow-up. This technique should be planned before surgery and after an accurate diagnosis is made using CBCT to reduce intraoperative root mobilisation. Further investigations should include a follow-up study at 10 years and more research about the mechanism of pulp healing." 16,17 Monaco et al. did caution that no matter what procedure was used, it is of utmost importance to adequately inform patients of the associated surgical risks prior to considering any form of impacted molar extraction.15,18
Numerous studies have investigated reasons for prophylactic extraction of impacted third molars.12-16 The most commonly grounds for the high rates were their association with pericoronitis, caries in the third or second molars, periodontal defects distal to the second molar, various odontogenic tumours and cysts and mandibular incisor crowding.19-23 Other studies have found that a semi-impacted third mandibular molar with a mesial angulation and in contact with the adjacent second molar often results in carious lesions developing on the distal root surface of the second molar. This was postulated to be due to the impacted third molar resulting in a deficient gingival collar around the second molar thus exposing the distal surface of the root to the oral cavity. This area is extremely difficult to keep clean, and may warrant third molar extraction for both hygiene purposes as well as to enable restoration of the second molar. If left untreated, the destruction could progress to the point where both teeth need to be extracted.13, 24, 25
McArdle et al. agreed that prophylactic removal of partially erupted third mandibular molars with a mesial inclination is indicated in order to prevent potential distal carious lesions developing on the second molars. However, the limitations of their study were that the cost-benefit aspect wasn't considered, nor possible other complications associated with impacted third mandibular molar removal.1,25
Polat et al (2008) noted that one should take the impaction depth and angulation of impacted third mandibular molars into consideration when an extraction decision is needed. They suggested that mesially and horizontally angulated (especially class A depth) impacted third mandibular molars could be prophylactically extracted.26
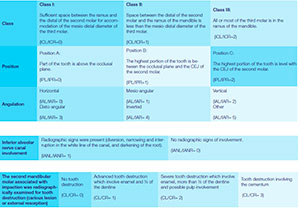
In this study the Pell and Gregory's classification27 was used for all visually confirmed impactions: In this system teeth are classified according to Class, position, and angulation. Rood and Shehab's classification was used to determine inferior alveolar nerve involvement28. The conditions are classified as follows:
Problem statement
Clinicians are often confronted with patients presenting with pathology related to impacted third molars. This may include conditions such as pericoronitis, trismus, and carious or periodontally involved second molars. They may be reluctant to extract the third molars, especially if the Orthopantomogram (OPG) indicates a close relationship to the inferior alveolar nerve canal. Many times they will manage these symptomatic patients by prescribing antibiotics and analgesics and referring them to a specialist for treatment. However, once the pain and symptoms subside a number of patients will not follow this route due to fear of surgery, time or financial constraints, long waiting periods before getting an appointment, or the belief that the problem has been resolved.
The prevalence of patients presenting with carious second molars and / or external resorption associated with impacted mandibular third molars has not been widely studied, especially amongst a South African population. A high incidence of such impacted third molar related pathology, could influence the treatment decision regarding prophylactic extraction of third molars, as well as the education of students and patients in this field.
Objectives.
1. Quantitatively determined the number of patients that presented with impacted mandibular molars for treatment at an Oral and Dental Hospital in Gauteng.
2. Quantitatively determined the number of patients that presented with carious/ external root resorption on second molars associated with mesially angulated impacted mandibular third molars (IMTM).
3. Determined the age and gender of patients with carious second molars associated with IMTM.
4. Determined the classification type according to the Pell and Gregory22 Classification (Class, Position and Inferior Alveolar Nerve Canal involvement 23) of impacted teeth that had associated carious second molars.
MATERIALS AND METHODS
Study design.
A Retrospective, analytic, cross-sectional study was performed using data from a three-month period. A daily report of all patients who had consulted in the Maxillo-facial and Oral Surgery Department during a three-month period from the 1 April to 30 June 2018 was generated on the GoodX Dental Studio system. During this time, 2250 had presented for oral surgery treatment. Patient file numbers that occurred more than once were eliminated manually. The random function in Microsoft Excel was utilised to randomly select half of the patients from the list and to generate a final sample size of 959 patients.
The files were examined and only those with an OPG not older than two years old (using 30 June 2016 as the cutoff date) were included in the study. Those that had been taken on the Sidexis system were categorised as O=1; those generated on Cliniview as O=2, and files with no / old / poor quality radiographs as O=0. The researcher was calibrated prior to radiographic examinations. The presence of impacted mandibular third molars (IMTM) on either of both sides was visually confirmed by the researcher. These were then all classified according to the Pell and Gregory's classification system, with the inferior alveolar nerve canal involvement being classified according to Rood and Shehab's guidelines as described above.
All the second mandibular molars associated with impactions were radiographically examined for any signs of tooth destruction (carious lesion or external resorption). They were then charted as those with No tooth destruction (CL/CR= 0); more advanced tooth destruction involving enamel and V2 of the dentine (CL/ CR= 1); Severe tooth destruction (Figure 1) involving enamel, more than 1/2 of the dentine and possible pulp involvement (CL/CR= 2) and tooth destruction involving the cementum (CL/CR= 3). Finally the age and gender of all patients who had been identified with IMTM was captured from the GoodX Dental Studio records using their file numbers for patient identification.
Repeatability was tested by having the primary researcher repeat the data extraction of 25 cases identified with the Random function of Microsoft Excel on a separate occasion without looking at the original data. Reliability was verified by having a second, experienced clinician carry out the same procedure on these 25 cases.
Data obtained from the data extraction sheet was captured on Microsoft Excell and imported into IMB SPSS statistics version 24 (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp) by Prof TC Postma who acted as the bio statistician. Approval to conduct the study was obtained by the Research committee of the school (RESCOM) as well as the ethics committee of the faculty (REC). Patients' identification was kept anonymous as only file numbers were used in the study. Confidentiality was maintained throughout the study.
RESULTS
Of the 959 patient file numbers selected, 238 (24.8%) had OPGs taken with the Sidexis system and 354 (36.9%) with Cliniview. Three hundred and sixty five (38.3 %) of the patients had no OPG that were older than 30 June 2016. Thus a total of 592 (61.7%) patient files were available for examination. From these a total of 100 (16.9%) and 112 (18.9%) were identified having IMTM on the left and right hand sides respectively.
Mesially angulated Class II Position A impactions constituted 32 (28.6%) out of 112 impactions on the right and 19% on the left. Mesially angulated Class II Position B impactions constituted 29 (25.9%) out of 112 impactions on the right and 20% on the left (Table 1). All other classification permutations rendered a very low prevalence.
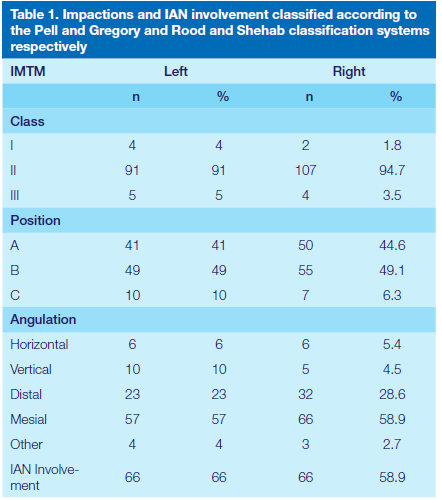
There was possible IAN involvement in 66 (66%) of 100 impactions on the left and 66 (58.9%) of 112 on the right. Of all the patients that presented with impactions 50.4% (67) were female and 49.6% were male. Indicating no gender predilection. The mean age of the sample was 31.15 (SD:11.12, 95%CI: 29.24-33.06) years old.
Signs of tooth destruction of the second mandibular molars on the left side (37) associated with IMTM were as follows:
None 59 (59%), Advanced 16 (16%), Severe 20 (20%), Cementum 5 (5%).
On the right (47) the results were: None 64 (57.1%), Advanced 9 (8%), Severe 21 (18.8%), Cementum 18 (16.1%) The relationship of IMTM classification components and tooth destruction on the distal surface of adjacent second molars is presented in Table 2.
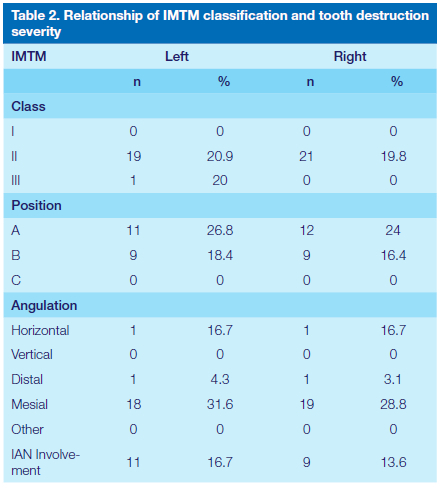
Severe caries was detected on the distal surface of the second molar in relation to 10 out of 32 (31.3%) mesially angulated Class II Position A impactions on the right side and 5 out of 19 (26.3%) on the left. Severe caries was detected on the distal surface of the second molar in 9 (31.3%) out of 29 mesially angulated Class II Position B impactions on the right side, and 3 (15.0%) out of 20 on the left. It should be noted that the prevalence of severe caries in relation to other impaction classification permutations is not reported due to very low prevalence (prevalence count of one or less) detected during this study.
DISCUSSION
The results showed that there was no gender predilection for third molar impactions. Most of the patients who presented with these were between the age of 24 and 33 years old, highlighting that clinicians should consider investigating for these when examining patients within this age group. Mesially angulated Class II Position A and Position B impactions were the most common and constituted 28.6% and 25.9% on the right and 19% and 20% on the left respectively. Of greater significance is that of all the impacted mandibular third molars approximately 2/3 (66% on the left and 58.9% on the right) had IAN involvement on radiographic examination. Thus the taking of OPG and careful radiographic examination is essential and justified when planning removal of IMTM in order to minimise or prevent IANC damage. One should also consider taking an additional CBCT in high risk cases of IANC damage to make a more accurate location of the IANC.
These results differed slightly from those of Mitra et al, who found that the majority of patients presenting with IMTM were males between the age of 21-25 years, and the least were females older than 45 years. However they too found the Mesioangular impactions to be the most common type.29 These results correspond closely with studies done in other populations as well. Polat et al found that amongst their Turkish population group, those between the ages of 26 and 35 years showed a high number of associated dental and orofacial complications if their impacted third molars had been retained. They also found there to be caries in 5.3% of the impacted lower third molars. In the same study teeth with horizontal and mesio-angular impactions had more associated pathological conditions than other types, most especially in the class A group with deeply seated teeth20. However these results should be viewed with caution and do not automatically indicate the need for prophylactic extraction of all IMTM. Both angulation and impaction depth of impacted lower third molars should be taken into consideration when making a decision as to whether or not to extract. Khawaja et alstudied a Saudi Arabian population group and found a high frequency of caries, external bone resorption and periodontitis in the second molars that were in close proximity to retained mesio-angular and horizontally tilted impacted third molars10.
In the present study only adjacent teeth showing signs of severe tooth destruction were reported as it is difficult to state categorically whether the mild tooth surface loss and cementum radiolucency is tooth destruction or radiographic cervical burnout. However, severe radiolucency can be distinguished from burnout and is thus undisputed. This could mean that the reported tooth destruction rates of 20% on the left and 18.1% on the right second mandibular molars associated with IMTM is an underestimation, and more than likely some of the milder cases those with cementum radiolucency did in fact have tooth destruction.
The reported rates of caries in the second molars associated with IMTM vary widely from as little as 1%20 to the 31.3% found in the present study. Thus caries alone should not be used as an indication for prophylactic third molar extractions. Other factors such as the extent of damage, the likelihood of its progression, and the potential for IAN damage during third molar removal need to be carefully considered when making a treatment decision. The latter is extremely important given that the present study found 66% of patients with IMTM on the left and 58.9% with it on the right had associated IAN involvement.
CONCLUSION
This study found no gender predilection with regards to IMTM, with most patients who presented with symptoms being 24 and 33 years of age. The most common type of impactions were mesially angulated, class II, position A and B. These were also associated with a higher level of tooth destruction on adjacent second molars as well as IAN involvement. The results help justify the taking of OPGs and an additional CBCT to evaluate IANC position associated with IMTM's in young patients with suspected IMTM and highlight the need for careful clinical examination of the associated second molars in order to prevent future tooth surface loss and other associated pathoses. While the study found that mesially angulated class II, position A and B IMTM have an increased risk of causing tooth destruction on the adjacent second molars, the significance is too small to justify prophylactic surgical extraction of impacted third molars alone, and the decision needs to be weighed up against the risks of possible IAN damage. This highlights the importance of annual dental visits to evaluate IMTM using OPGs and decide the need for an additional CBCT.14
REFERENCES
1. McArdle LW, Renton T. The effects of NICE guidelines on the management of third molar teeth. British Dental Journal. 2012 14 May; 213:E8. [ Links ]
2. Al-Zoubi H, Alharbi AA, Ferguson DJ and Zafar MS. Frequency of impacted teeth and categorization of impacted canines: A retrospective radiographic study using orthopantomograms. Eu J Dent. 2017; 11 (1):117-121. [ Links ]
3. Bagheri SC, Bel RB, Khna HA. Current Therapy in Oral and Maxillofacial Surgery. 1st ed. St Louis: Elsevier Saunders; 2012. [ Links ]
4. Pedro FL, Bandeca MC, Volpata Le et al. Prevalence of impacted teeth in a Brazilian subpopulation. J Contemp dent Pract. 2014;15:209-213. [ Links ]
5. American Association of Oral and Maxillofacial Surgeons : Parameters of care: clinical practice guidelines for oral and maxillofacial surgery. 2007. American Association of Oral and Maxillofacial Surgeons Rosemont, Ill [ Links ]
6. Moynihan P and Petersen PE. Diet, nutrition and the prevention of dental diseases. Public Health Nutrition: 2004; 7(1A), 201-226 DOI: 10.1079/PHN2003589 [ Links ]
7. American Association of Oral and Maxillofacial Surgeons White Paper: Management of Third Molar Teeth, 2016. [ Links ]
8. SASMFOS [Internet] SASMFOS Position Statement on Third Molar (Wisdom teeth) Surgery. [cited 2018 April 3]. Available from: http://sasmfos.org/files/sasmfos_third_molar_policy.pdf. [ Links ]
9. American Association of Oral and Maxillofacial Surgeons. White paper on why, when and how to treat third molar teeth (2011).Accessed at: https://www.prnewswire.com/news-releases/aaoms-white-paper-discusses-why-when-and-how-to-treat-third-molar-teeth-135889358.html; Accessed on 07-08-2020 [ Links ]
10. Khawaja NA, Khalil H, Parveen K, Al-Mutiri A, Al-Mutiri S, Al-Saawi A. A Retrospective Radiographic Survey of Pathology Associated with Impacted Third Molars among Patients Seen in Oral & Maxillofacial Surgery Clinic of College of Dentistry, Riyadh. Journal of International Oral Health 2015; 7(4):13-17. [ Links ]
11. Susarla SM, Dodson TB. Preoperative computed tomography imaging in the management of impacted mandibular third molars. Journal of Oral and Maxillofacial Surgery. 2007;65:83. [ Links ]
12. Friedman JW. The prophylactic extraction of third molars: a public health hazard. Am J Public Health. 2007; 97:1554-1559. [ Links ]
13. Ye Z, Qian W, Wu Y, Sun B, Zhiyao L, Ling F, Xiang F, Zhu M, Zhang Y. Is prophylactic extraction of mandibular third molar indicated? A retrospective study. Research Square. 2020 [ Links ]
14. Saha N, Kedarnath NS, Singh M. Orthopantomography and Cone-Beam Computed Tomography for the Relation of Inferior Alveolar Nerve to the ImpactedMandibular Third Molars. Ann Maxillofac Surg 2019;9:4-9. [ Links ]
15. Monaco G, De Santis G, Pulpito G, Gatto MRA, Vignudelli E, Marchetti C. What Are the Types and Frequencies of Complications Associated With Mandibular Third Molar Coronectomy? A Follow-Up Study. Journal of Oral and Maxillofacial Surgery. 2015 Jul; 73(7): 1246-1253. [ Links ]
16. Ecuyer J, Debien J. Surgical deductions. Actual Odontostomatol. 1984; 148: 695. [ Links ]
17. Monaco G, D'Ambrosio M, De Santis G, Vignudelli E, Gatto MRA, Corinaldesi G. Coronectomy: A Surgical Option for Impacted Third Molars in Close Proximity to the Inferior Alveolar Nerve-A 5-Year Follow-Up Study. Journal of Oral and Maxillofacial Surgery. 2019; 77:1116-1124. [ Links ]
18. Ruga E, Gallesio C, Boffano P. Mandibular Alveolar Neurovascular Bundle Injury Associated With Impacted Third Molar Surgery. Journal of Craniofacial Surgery. 2010 Jul ; 21(4): 1175-1177. [ Links ]
19. Da Costa MG, Pazzini CA, Pantuzo MCG, Jorge MLR, Marques LS. Is there justification for prophylactic extraction of third molars? A systematic review. Braz Oral Res. 2013 Mar-Apr;27(2):183-8 . [ Links ]
20. Laskin DM. Evaluation of the third molar problem. J Am Dent Assoc. 1971 Apr;82(4):824-8. [ Links ]
21. Schulhof RJ. Third molars and orthodontic diagnosis. Journal of Clinical Orthodontics. 1976 Apr;10(4):272-81. [ Links ]
22. Lysell L, Rohlin M. A study of indications used for removal of the mandibular third molar. Int J Oral Maxillofac Surg. 1988 Jun;17(3):161-4. [ Links ]
23. Stanley HR, Alattar M, Collett WK, Stringfellow HR Jr, Spiegel EH. Pathological sequelae of "neglected" impacted third molars. J Oral Pathol. 1988 Mar;17(3):113-7. [ Links ]
24. McArdle LW, Renton TF. Distal cervical caries in the mandibular second molar: an indication for the prophylactic removal of the third molar? British Journal of Oral and Maxillofacial Surgery. 2006;44:42-5. [ Links ]
25. McArdle LW, McDonals F, Jones J. Distal cervical caries in the mandibular second molar: an indication for the prophylactic removal of third molar teeth? Update. British Journal of Oral and Maxillofacial Surgery 2014: 185-189. [ Links ]
26. Polat HB, Ozan F, Kara I, Ozdemir H, Ay S. Prevalence of commonly found pathoses associated with mandibular impacted third molars based on panoramic radiographs in Turkish population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:e41-e47. [ Links ]
27. Pell GJ, Gregory GT. Impacted mandibular third molars: Classification and modified technique for removal. The Dental Digest 1933 Sep; 39(9): 325-338. [ Links ]
28. Rood JP, Shehab BA. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 1990;28:20-5. [ Links ]
29. Mitra R, Prajapti VK, Vinayak KM, Nath S, Sharma N. Prevalence of Mandibular Third Molar Impaction. International Journal of Contemporary Medical Research. 2016;3(9): 2625-2626. [ Links ]
 Correspondence:
Correspondence:
Leanne Sykes
E-mail: Leanne.sykes@up.ac.za
Author contributions:
1 . LM Sykes: 30%;
2 . TC Postma: 30%,
3 . L Dawson: 40%,