Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.77 no.3 Johannesburg Abr. 2022
http://dx.doi.org/10.17159/2519-0105/2022/v77no3a5
RESEARCH
Evolution of Sialendoscopy in clinical practice: Survey of attending practitioners
SH MaharajI; NO KanaII; Z CassimIII; S MungulIV
IMBBCH, MMED, FCORL (SA), Head of Academic Department, Department of Otorhinolaryngology, University of the Witwatersrand, Johannesburg, South Africa. ORCID Number: 0000-0002-2118-2400
IIIMBChB, MMED, FCORL(SA), Otorhinolaryngologist in private practice at Netcare Milpark Hospital, Johannesburg, South Africa. ORCID Number: 0000-0001-8902-2684
IIIBA (Speech Pathology and Audiology), MA (Audiology), Unversity of the Witwatersrand, Johannesburg, South Africa, Johannesburg South Africa, South Africa, ORCID Number: 0000-0001-8075-335X
IVMBBCH, MMED, FCORL (SA), Department of Otorhinolaryngology, University of the Witwatersrand, Johannesburg, South Africa. ORCID Number : 0000-0003-2553-5506
ABSTRACT
INTRODUCTION: Sialendoscopy is a relatively new technique that is safe, minimally invasive and effective as a diagnostic as well as a therapeutic tool for the management of deep seated, proximal, salivary ductal obstruction. However, more than 20 years since its inception it is still not in mainstream use worldwide.
OBJECTIVES: Our aim of this study was to ascertain the awareness of sialendoscopy amongst the medical fraternity in South Africa. More specifically, to determine whether it was frequently used amongst practitioners and the type of cases managed using sialendoscopy
METHODS: An exploratory survey design involving 100 practitioners was used to collect data, using an online survey involving 10 closed-ended multiple choice questions.
RESULTS: The results of the study revealed that while practitioners saw patients who could benefit from sialendoscopy, most practitioners did not feel comfortable performing the procedure independently, and as such, most patients were referred on to other professionals for management.
CONCLUSION: The majority of attending practitioners believed that they would benefit from further practical and theoretical training in the field of sialendoscopy, illustrating the need for continued professional development in this area.
Key words: Sialendoscopy; sialolithiasis; salivary glands; gland-preserving treatment
INTRODUCTION
Sialendoscopy is a relatively new technique, first described by Katz et al. in 1991.1 Before the advent of sialendoscopy, distal salivary gland obstructions were removed via intraoral excision. However, proximal obstructions were impossible to reach, and as such, treatment methods ranged from the use of antibiotics and anti-inflammatories to the use of sialadenectomy.2
The technique of sialendoscopy has evolved over the years and is now used across the world.2 The technique entails using semi-rigid endoscopes to cannulate and view the interior of the salivary ducts. These endoscopes can be used as both diagnostic and interventional tools due to the presence of a hollow working channel that allows the passage of wire baskets, drills and fibre-optic lasers to fragment and remove calculi.3
Salivary duct obstruction is, however, not confined to the presence of salivary calculi alone. Salivary ducts can also be obstructed by polyps, mucous plugs and strictures.4,5
The role of adenectomy in the treatment algorithm for salivary gland ductal obstruction may have become significantly smaller since the advent of sialendoscopy, however, it still has a place.
The management of these patients differs across the clinical units and there is still no consensus as to what factors are used by attending clinicians to determine which patients qualify for gland preservation therapy.
Capaccio et al, state that although available clinical evidence supports minimally invasive gland preservation because it significantly reduces the use of invasive sialadenectomy6, there is a lack of consensus within the literature regarding sialendoscopy practice and patient parameters such as age, gender and antibiotic treatment.
AIM OF THE STUDY
The aim of this study was to ascertain the current clinical practices amongst attending medical practitioners with respect to sialendoscopy. This was done by means of a structured closed-ended survey conducted amongst practitioners managing these patients. Data on the clinical practice of sialendoscopy and the management of sialolithiasis is important to inform evidence based practice both locally and internationally; and can be used to implement a specific sialendoscopy protocol which can be disseminated widely.
METHODS
The study utilized an exploratory survey design with the use of a purposive convenience sampling approach to select participants for this study. A purposive sampling method allows for participants to be chosen based on set criteria stipulated by the research topic. As such, the sample size included 100 treating clinicians which included medical trainees, otorhinolaryngologists, maxillofacial surgeons, general surgeons, dentists and general practitioners.
Data collection was conducted using an online survey via Survey Monkey, which included 10 closed-ended multiple choice questions, as displayed in Figure 1. The online link to the survey was distributed digitally to individuals who met the inclusion criteria for the study, to the discretion of the researchers. Data was analysed using descriptive statistics, whereby, the answers from the respondents were coded and classified according to the percentage of their occurrence.
As part of the research conducted by the researchers for the study entitled "The evolution of sialendoscopy in clinical practice", ethics clearance was received from the relevant university human research ethics committee and clearance was granted unconditionally. This clearance certificate was extended by the Ethics Committee for the current study. All information was kept confidential and anonymous and was coded by the researchers. In the current study there was a threat to validity based on there being a risk of bias, between the survey result and population value. This is as there was a sampling bias and a small sample size, which meant that the results obtained may not have been representative of the wider population of practitioners, and as such, the results of this study cannot necessarily be generalized to a wider population.
RESULTS
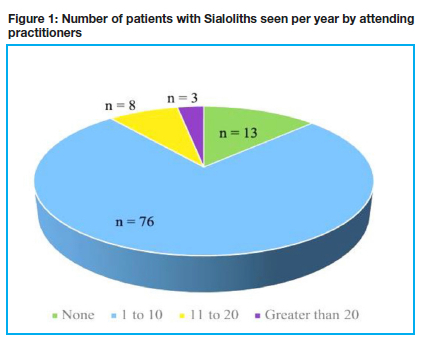
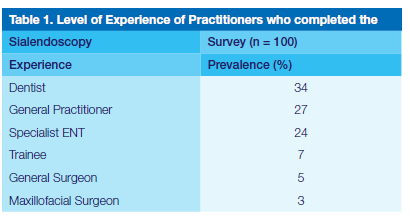
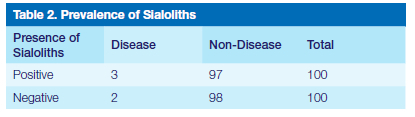
A total of 100 practitioners partook in the study, with 89 people completing the full survey by answering all 10 questions posed. Table 1 describes the level of experience of practitioners who completed the survey. Figure 2 displays the number of patients per year, seen with salivary stones by clinicians in the study. The majority of practitioners (46%; N = 100) reported that in their experience, salivary stones was most prominent amongst young adults between the ages of 16 and 40, followed closely by middle aged people between the ages of 40 and 60, which was noted by 42% (N = 100) of practitioners. Practitioners noted that salivary stones were not common amongst elderly patients greater than 60 years of age and in children under the age of 16.
Most practitioners prescribed Penicillin to treat salivary stones (69%; N = 100) while 17% (N = 100) of practitioners prescribed other antibiotics aside from Penicillin, Macrolides or Quinolones. Most respondents (23%; N = 100) reported using a Sialogram to investigate patients with suspected salivary stones, followed closely by CT scans (16%; N = 100) and ultrasound of the salivary glands (15%; N = 100). Nineteen percent of practitioners used more than one method to investigate the salivary glands, and no practitioners reported using MRI scans.
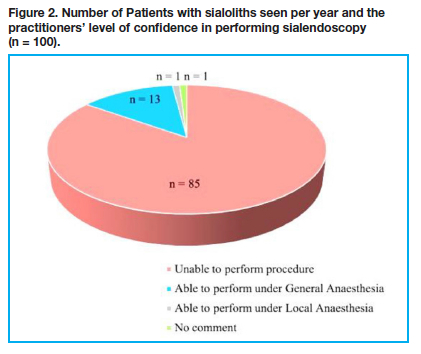
The majority of practitioners (82%; n = 99) reported that they did not have access to sialendoscopy within their clinical settings. As per Figure 3, the majority of practitioners reported that they were unable to perform sialendoscopy and very few practitioners (10%; N = 100) felt confident performing sialendoscopy independently, with 76% (N = 100) of people preferring to refer these cases to fellow colleagues. If assisted by another surgeon, 14% (N = 100) of practitioners noted that they would be able to perform the procedure.
Almost all practitioners felt that they would benefit from training workshops in sialendoscopy (89%; N = 100), with 68% (N = 100) noting that both theoretical and practical training would be useful. Eleven percent (N = 100) of practitioners did not feel that they would benefit from training. While most practitioners (68%; n = 97) were not sure if sialendoscopy changed the number of patients with salivary stones treated with open surgery, 21% (n = 97) believed that it decreased the number of open surgeries and 9% (n = 97) did not think that it made a difference.
DISCUSSION
Sialendoscopy is a relatively new and an increasingly used modality in the management of obstructive diseases of the major salivary glands. Based on international studies salivary glands removed for sialolithiasis have normal glandular architecture, therefore organ preservation should be the goal7, thus reducing the morbidity of the open surgery.
It is noted that 73% of practitioners included in the survey were less to not experienced colleagues (general surgeons, dentists, general practitioners, medical trainees) in the management of sialolithiasis. These are colleagues who are mainly referring, and may not be treating those patients. Most may not be familiar with salivary gland diseases and this was evident concerning tumors, but even more for inflammatory or obstructive diseases. This is also underscored by the low number of salivary stones seen by majority of the participants in this study (76%; N = 100) saw between 1 and 10 cases per year. Not surprising that for instance a general practitioner has no access to sialendoscopy as this is a rare diagnosis in their practice and/or the equipment is very specific. Therefore, general practitioners may not have been an appropriate group to participate in this study and evaluate this.
Sialendoscopy is a specific procedure mostly managed by ENT specialists, or Maxillofacial surgeons, however it is noted that only 27% of these practitioners took part in this study. This may indicate that this study seems not to be representative to judge if this technique is used adequately or not and/or should be implemented more intensely.
Training workshops may be beneficial for practitioners not familiar with salivary gland diseases to better understand the indications of sialendoscopy and to refer these patients to more experienced units/colleagues.
It was noted in the results that 68% of participants were not sure if sialendoscopy changed the number of patients with salivary stones treated with open surgery. This seems to correspond with the 73% of practitioners who supposedly are not experienced with obstructive salivary diseases. These and all other data should be discussed within the discussion part (see below).
Demographics
The incidence of sialolithiasis has according to our knowledge not been described in the South African setting. The vast majority of respondents' saw between 1 to 10 patients a year that presented with salivary stones and most of these patients were young adults. This illustrates that practitioners are exposed to the kind of patient load that would benefit from sialendoscopy.
Ideally sialendoscopy should be performed by experienced units. Diagnostic sialendoscopy may be performed by less experienced colleagues. Interventional sialendoscopy, if successfully performed, needs much more practical experience and should be performed at least not in low volume units (1-10 patients/year). Prerequisites of performing sialendoscopy are firstly sufficient and appropriate equipment and secondly experienced personnel (including experienced assistant personal). Otherwise the results will be not sufficient for the patient, in particular in the long-term course.
Based on the cohort from our study, the prevalence of salivary stones was estimated to be 2.5%. This is comparable to international studies that reported the prevalence to be between 1% and 3% of the population.8 Based on the current body of knowledge, there is a peak incidence between the third and fifth decade. As many as 4% of cases occur in individuals younger than 20 years of age.8 These trends were noted in our study as well.
A study by Gallo et al. (2016), in which 1152 sialendoscopies were performed, showed a male to female preponderance of 52% vs 48%. Sialoliths made up 53.1% of the pathology in this cohort. Stenotic ducts made up 9.4% of the study population. Idiopathic recurrent sialadenitis cases were 27.2% of the total number of cases. Autoimmune cases were 3.4%, while radioiodine exposed cases were 1.6% of cases and 0.5% of cases were post radiotherapy.9 The total Juvenile Recurrent Parotitis cases came to 4.1%.10 The overall success rate was 97.5%. The majority of cases were of the submandibular glands at 55.4% and parotid gland cases accounted for 44.6% of cases.
Deenadayal et al., found in their study of 133 cases that obstruction occurred bilaterally in 26 cases, while 10 cases were normal, and in a total of 149 glands, pathology was found. 78 patients were male and 55 patients were female and 16 were paediatric cases. The age range of the study population was from age 3 to age 76.11
Investigations
Traditionally, the established gold standard in diagnosing salivary duct obstruction was the sialogram. It has since been superseded by ultrasound, CT (computerized tomography) scan and MRI (magnetic resonance imaging) scanning.
In our study the investigation of choice was the sialogram. The advantage of sialography is that it can show the salivary ductal system beyond a calculus, however there is radiation exposure to the patient along with the possibility of perforating the duct or pushing a calculus more proximally into the gland. Although this is not regular sequelae, it may render sialendoscopy thereafter, more difficult. Ultrasound is non-invasive, widely available, cost effective. It represents a first line diagnostic technique. The quality of the results is dependent on the experience of user/operator. It is better for the one performing the sialendoscopy to be the one who performed the initial ultrasound. CT scan of the region is significantly more expensive and as such, no practitioner in the current study reported utilizing it.
Conservative treatment
Therapeutic strategy depends on the size and location of the calculi. Conservative treatment, rather than surgical removal, is accepted as the first choice in managing small calculi located in the distal section of the duct, expecting their spontaneous expulsion. Hydration should be administered to patients with infrared heating and massage of the gland. Natural sialagogues such as a slice of lemon or medications such as pilocarpine are beneficial as they stimulate the production of saliva and subsequent flushing of calculi. Antibiotics should be initiated whenever infection is suspected to be combined.12 Administration of penicillinase-resistant and staphylococcal agents for 7-10 days, is generally accepted. However, many cases fail to respond to such a regimen. The success rate of spontaneous passage of stones with conservative management for a period of 3 months is only 10%.
Surgical treatment
Sialendoscopy is a relatively new procedure for the diagnosis and treatment of salivary duct diseases. As with any new procedure it seems that there is a definite learning curve involved in achieving success with sialendoscopy.
According to Steck et al. (2016), a study was conducted to evaluate learning progression of a single surgeon with the aim to estimate how many procedures were necessary to achieve better results and for the surgeon to perform a safe sialendoscopy and to establish if complication rates were higher in the beginning of the learning. In this study most of the endoscopies (85%) were performed under general anaesthesia however the procedure can be performed under local anaesthesia. In the initial cases performed by the surgeon using the same equipment and after initial hands on training, two of the most common problems encountered included the failure to cannulate ducts and the failure to remove stones. Operative times was slightly higher in the first 50 cases (56 minutes) compared to the subsequent 63 cases (41 minutes). The complication rates were higher in the first 50 cases as opposed to subsequent cases where better outcomes were evident and complications low.13
Luers et al. (2010) concluded that the performance of sialendoscopy improves with time and experience. The study highlighted that in order to improve skills to an adequate level to achieve satisfactory operation times and performance ratings, it required a number of 30 cases, however, true proficiency occurred after the first 50 cases. Within this study, the average operative times were 39 minutes and there was a significant improvement in the average operative time and performance rating after the first 10 cases performed and a further improvement was noted then again after 30 cases.14
The above studies are indicative that the performance of sialendoscopies improves with time and amount of experience and demonstrates the remarkable learning curve of surgeons. Koch et al., in their study published in 2012, found that gland-preserving treatment was possible in 96.8% of the patients in their study, with 92.2% of the patients reporting no relevant symptoms postoperatively.15
Long term results of sialendoscopy are to be judged on its ability to avoid gland resection with its concomitant complications, whether its results are long lasting and whether it has fewer and less severe complications than sialadenectomy.16
CONCLUSION
Analysis of our data shows that most of the respondents were aware of the procedure, and were exposed to the type of patient load who required sialendoscopy. However, the majority of practitioners were not able to perform the procedure independently, and reported that they preferred to refer patients requiring the procedure on to other colleagues as they may be less to not experienced in management of salivary duct diseases. While a portion of practitioners were unsure of its effects, many indicated that sialendoscopy had led to a decrease in the need for open surgery.
Despite the majority of practitioners not having access to sialendoscopy equipment, if practitioners were better equipped to perform the procedure, they were most likely to use it in their clinical settings, based on the number of patients requiring it and the positive views towards the procedure. Diagnostic sialendoscopy may be performed by less experienced colleagues. Interventional sialendoscopy, if successfully performed, needs much more practical experience. In fact, most practitioners felt that they would benefit from further theoretical and practical training. Training workshops may be beneficial for practitioners not familiar with salivary gland diseases to better understand the indications of sialendoscopy and be able to make more informed referrals to experienced units and practitioners.
The results of the study reveal that there is a need for further training in sialendoscopy in the South African setting and that this would enhance clinical practice to the benefit of the South African public.
Compliance With Ethical Standards
i) Research Funding
No research grant was utilized for the study conducted.
ii) Conflict of Interest
The authors hereby declare that they have no conflict of interest.
iii) Ethical Approval
All procedures performed in this study involving human participants were conducted in accordance with the ethical standards of the University of the Witwatersrand Human Research Ethics Committee (Protocol Number M111130) and permission was taken from the committee prior to conducting the research study.
iv) Informed consent
Informed consent was obtained from the individual participants who were included in the study and participants were assured that anonymity would be maintained as no identifying information would be disclosed within the article or to others outside of the researchers who were conducting the study.
REFERENCES
1. Katz P et al. Endoscopy of the salivary glands. Ann Radiol (Paris). 1991 [cited 2018 Oct 6];34(1-2):110-3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1897843 [ Links ]
2. Al-Abri R, Marchal F. New Era of Endoscopic Approach for Sialolithiasis: Sialendoscopy Sultan Qaboos University Medical Journal. 2010;10(3):382-387. [ Links ]
3. Marchal F, Dulguerov P, Becker M, Barki G, Disant F, Lehmann W. Specificity of parotid sialendoscopy. Laryngoscope. 2001;111(2):264-271. [ Links ]
4. Erkul E, Gillespie MB. Sialendoscopy for nonBstone disorders: The current evidence. Laryngoscope investigative otolaryngology. 2016 Oct;1(5):140-5. 19. [ Links ]
5. Marchal F, Becker M, Kurt AM et al. Histopathology of submandibular glands removed for sialolithiasis. Annals of Otology, Rhinology & Laryngology. 2001 May;110(5):464-9. [ Links ]
6. Capaccio P, Torretta S, Pignataro L et al. The role of adenectomy for salivary gland obstructions in the era of sialendoscopy and lithotripsy. Otolaryngologic Clinics of North America. 2009 Dec 1;42(6):1161-71. [ Links ]
7. Bowen MA, Tauzin M, Kluka EA. Diagnostic and interventional sialendoscopy: A preliminary experience. The Laryngoscope. 2011 Feb;121(2):299-303. [ Links ]
8. Lustmann J, Regev E, Melamed Y. Sialolithiasis. A survey on 245 patients and a review of the literature. International Journal of Oral Maxillofacial Surgery. 1990;19:135. [ Links ]
9. Gallo A, Capaccio P, Benazzo M et al. Outcomes of interventional sialendoscopy for obstructive salivary gland disorders: An Italian multicentre study. Acta Otorhinolaryngologica Italica. 2016 Dec;36(6):479. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28177330 [ Links ]
10. Papadopoulou-Alataki E, Chatziavramidis A, Vampertzi O. Evaluation and management of juvenile recurrent parotitis in children from northern Greece. Hippokratia. 2015 Oct;19(4):356. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27688702 [ Links ]
11. Deenadayal DS, Bommakanti V. Sialendoscopy et al. A review of 133 cases. International Journal of Otolaryngology and Head & Neck Surgery. 2016 Jan 15;5(01):28. [ Links ]
12. Pachisia, S, Mandal G, Sahu S, Ghosh S. Submandibular sialolithiasis: A series of three case reports with review of literature. Clinics and Practice. An international Journal of Medical Case Reports. 2019 Jan 29; 9(1): 1119. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6444375/ [ Links ]
13. Steck JH, Stabenow E, Volpi EM et al. The learning progression of diagnostic sialendoscopy. Brazilian journal of otorhinolaryngology. 2016 Apr;82(2):170-6. [ Links ]
14. Luers JC, Damm M, Klussmann JP. The learning curve of sialendoscopy with modular sialendoscopes: A single surgeon's experience. Archives of Otolaryngology-Head & Neck Surgery. 2010 Aug 16;136(8):762-5. [ Links ]
15. Koch M, Iro H, Klintworth N et al. Results of minimally invasive gland-preserving treatment in different types of parotid duct stenosis. Archives of Otolaryngology-Head and Neck Surgery. 2012 Sep 1;138(9):804-10. Available from: http://archotol.jamanetwork.com/article.aspx?doi=10.1001/archoto.201 2.1618 [ Links ]
16. Koch M, Künzel J, Iro H et al. Long-term results and subjective outcome after gland-preserving treatment in parotid duct stenosis. The Laryngoscope. 2014 Aug;124(8):1813-8. [ Links ]
 Correspondence:
Correspondence:
Dr SH Maharaj
Department of Otorhinolaryngology
University of the Witwatersrand
Tel: 011 4884 299
E-mail:Shivesh.maharaj@wits.ac.za
Author contributions:
1 . Prof SH Maharaj: 30%
2 . Dr NO Kana: 25%
3 . Ms Z Cassim: 25%
4 . Dr S Mungul: 20%














