Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.77 no.3 Johannesburg Abr. 2022
http://dx.doi.org/10.17159/2519-0105/2022/v77no3a2
RESEARCH
Prevalence of Sharps Injuries at a Tertiary Teaching Oral Health Centre, Gauteng, South Africa
Y Malele-KolisaI; OK SibanyoniII; JB MthandazoIII; T NaidooIV; T MhlabaV; H IsmailVI; N LecogeVII
IDepartment of Community Dentistry, School of Oral Health Sciences, University of the Witwatersrand. ORCID: 0000003-3368-9193
IIBSc (Microbiology, BDS), Dentist and former Trainee at the Wits School of Oral Health Sciences. ORCID: 0000-0002-9903-9612, Medicare24, Boksburg, Johannesburg
IIIBTech, BDS. Dentist and former Trainee at the Wits School of Oral Health Sciences. ORCID: 0000-0002-32106868, Vancouver, Canada
IVBDS. Dentist and former Trainee at the Wits School of Oral Health Sciences. ORCID: 0000-0003-1212-6594,Uthukela District, Estcourt
VBDS. Dentist and former Trainee at the Wits School of Oral Health Sciences. ORCID: 0000-0002-2840-765X, Sefako-Makgatho Health Science University, Pretoria
VIBDS, Department of Community Dentistry, School of Oral Health Sciences, University of the Witwatersrand. ORCID: 0000-0002-3698-1221, The Dentist Dental Studio, Estcourt, Inkosi Langalibalele Municipality, Uthukela District, KZN
VIIBDS Dentist and former Trainee at the Wits School of Oral Health Sciences. ORCID: 0000-0002-4680-8166, Tlakgameng Community Health Centre, City
ABSTRACT
INTRODUCTION: Needle-stick and sharps injuries are an occupational hazard in dental training institutions. The study aimed to quantify and describe the nature of Needle-stick and sharp injuries (NSI) at a Tertiary Teaching Oral Health Centre (TTOHC) in South Africa
METHODS: An analytic, cross-sectional study was conducted among students engaged in clinical service and oral health staff supervising them at the Oral Health Centre, Gauteng, South Africa. An adapted 18-item self-administered questionnaire was provided to all students and staff. Standard ethical guidelines were followed according to institutional ethics committee approval (M171131
RESULTS: A response rate of 88% (n=73) was obtained from students, with the majority of participants being female(67%), dentistry students (88 %), aged between 18-25 years, in their fourth year of study (45%) while only 3.7% were final year oral hygiene students. The staff participants were dentists (80.6%) while most staff participants (88.3%) were employed for 3 years or less. The NSI prevalence at the TTOHC was 41.3% (n=45). The number of staff reporting the injury for both staff and students was recorded to be 80% (n = 36 of 45 injuries), with 77.3% of injured individuals receiving post-exposure prophylaxis (PEP) against possible HIV-infection, however, more than a third (39%) reported not to have completed the PEP. The department in which the most NSIs occurred was Maxillofacial and Oral Surgery. Sharp injuries were mostly due to needle sticks. Most NSIs occurred among senior students with more clinical experiences and particularly during the early and late periods in a year
CONCLUSION: The prevalence of needle and sharp injuries was high and of concern. The sharps injury reporting rate was good, however, less than half of injured individuals completed the PEP treatment. The findings highlighted which students were most at risk to encounter NSI, including the period during their training when it was most likely to occur, thus enabling directed re-emphasis and training in Infection Control and Prevention
Key words: Needle-stick, sharps injuries, dentistry, training institution
INTRODUCTION
Needle-stick and sharps injuries (NSI) are described as "puncture wounds, cuts, or scratches inflicted by medical instruments that may be contaminated with a patient's blood or other body fluids"1. NSI are a major occupational hazard in the oral healthcare professions, especially in the busy academic tertiary institutions, due to the high workload and inexperience among students 2.
Globally the pattern of NSI is experienced differently in various health facilities. Lee et al., reported 40.87% NSI prevalence amongst clinicians (dentists and students) at a Taiwan University while (Lee et al, 2012) Leggart (2009) revealed a higher prevalence of 72% among United States of America (USA) dental students3. A relatively low prevalence 23% of NSIs was reported at a College of Dentistry in the United Arab Emirates (UAE)4. In developing countries, a Kenyan University reported 29% prevalence among dental students, slightly higher than the UAE prevalence5. In South Africa, however, Siddiqi et al reported a very high prevalence among undergraduate students (62.1%), followed by postgraduate students (17; 14.7%) in a Dental Teaching University in Cape Town6.
The risk of NSI are particularly concerning in dentistry due to the use of a wide variety of sharp instruments 2. Routine medical and dental sharp apparatus such as needles, scalpels, burs, scalers, probes, and forceps contribute to most of the injuries 7. NSI carry the risk of infection by saliva and blood-borne infections organisms, particularly in the oral cavity where a multitude of organisms exist. Infection resulting from blood borne pathogens include, but is not limited to Hepatitis B and C virus and HIV8.The risk of HIV infection from occupational NSI range from 0.03% to 0.3%, which increases with the depth of injuries, volume of inoculated blood and hollow needle injuries whereas the risk for hepatitis B infection following exposure from a HBeAg-positive patient is between 6 - 30%. Hepatitis C virus( HCV), with an infection rate of 10%, hepatitis is of greater concern than HIV-infection in the event of NSI9. Apart from the physical effects and infection risk of NSIs, it was found that mental health consequences may be experienced subsequent to the injuries10.
The Tertiary Training Oral Health Centre (TTOHC) enforces a compulsory Hepatitis B virus (HBV) vaccination for all clinical workers and students to minimise post exposure risks. Non-compliance with vaccination or failure to acquire regular booster doses and decreased antibody titres can result in infection, especially with highly infectious strain9. Choi and co-workers suggest that the lack of reporting of injuries constitute noncompliance with institutional guidelines11.
Various factors, such as inexperience during early clinical years, senior students who become complacent, the time of year (July-September), the day of the week (Wednesdays and Fridays), different dentistry disciplines (Restorative Dentistry and Maxillofacial Dept.) have been reported to influence the prevalence rate and increased likelihood of injuries 2,4
The NSI injuries are a particular public health concern, especially among oral health care professionals due to the high frequency of occurrence and because it is preventable. Because of significant differences on the prevalence of needle-stick and sharps injuries reported among dental teaching institutions, it is important that each institution determines what their prevalence is12, hence the aim of the current study was to not only quantify but also describe the nature of NSI at a TTOHC in Johannesburg, South Africa.
METHODS
An analytic, cross-sectional study was carried out to investigate the prevalence, the outcome of NSIs and the factors associated with the injuries. Qualified dentists, dental therapists and oral hygienists who supervised students, as well as all oral hygiene and dentistry students engaged in clinical service were invited to participate in the study at the Oral Health Centre, which is a tertiary teaching hospital in Gauteng, South Africa. Excluded from the study were departmental and unit heads and laboratory staff members as they do not routinely handle contaminated sharp instruments used in patient's mouths.
Data collection
A self-administered questionnaire was made available to staff and students during March 2018. During March 2018, when the survey was conducted, there was a total of 83 students involved in clinical service and 55 staff members who supervised them. The questionnaire was modified and adapted from a percutaneous exposure incidents tool by Siddiqi and co-workers 6. The questionnaire was piloted for feasibility, clarity and the time required to complete it. The 18-item questionnaire sought information on student and staff demographics, occurrence of needle-stick and sharps injury, mode of injury, when and where the injury occurred, action taken after the injury.
Approval to carry out the study was obtained from the relevant authorities and the Human Ethics Research Committee ( M171131.)
Data Analysis
Data from the questionnaires was captured, verified and cleaned using Microsoft Excel 2010. The data was then exported to Stata version 14.1 (StataCorp, USA) and analysed. Descriptive statistics was done. Group differences were assessed by using the Pearson Chi-squared test and the Fischer exact test for cells less than 5. Bivariate analysis was conducted for factors most likely to influence the needle stick injury outcomes.
RESULTS
A response rate of 88%; (n=73) was recorded for students and 65% (n=36)-for staff. Completing the questionnaire took approximately 15 minutes.
Table 1 reveals the majority of the all participants to be female (67%) and aged between 18-25 years (56%). Among student participants, dentistry students in their 4th year of study constituted the majority (30.3%), followed by students in their 5th year of study (14.7%). Oral hygiene students in their final year (3rd) represented 3.7% of the student participants. Among staff members, the majority were dentists/specialists at 80.6% while the majority of staff members (88.3%) had been employed for 3 years or less.
The total NSI prevalence at the TTOHC was 41.3% (n=45) with the split of 27.5% (n=30) among students and 13.8% (n=15) staff members. The reporting status refers to the number of staff reporting the injury. The sharps injuries reported following an injury by both staff and students was recorded to be 80% (n= 36 of 45 injuries) (Fig 1). Most of the NSI sustained by students occurred in the Maxillofacial and Oral Surgery department, followed by Oral Rehabilitation. The fourth year dental students sustained the most injuries. The lowest percentage of injuries occurred in the Paediatric Dentistry Department and at Community Outreach sites (Fig 2). Among staff members, Maxillofacial and Oral Surgery site resulted in the highest frequency of injuries.
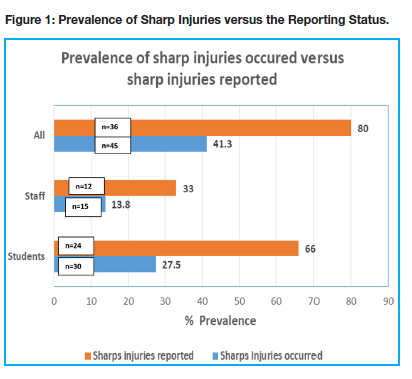
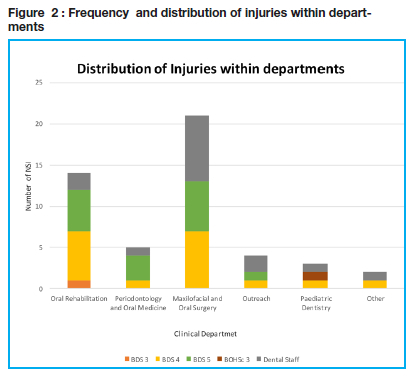
Table 2 illustrates the differences between students and staff members regarding the number of times of experiencing NSI, with a significant majority only experiencing one incident. One participant reported incurring more than Ave injuries within 12 months. The needle stick was the most common injury, with a statistically significant higher prevalence among students than staff members. Students sustained more injuries during the 1st Term (Jan-Mar), followed by 2nd Term (Apr-Jun) and 4th Term (Oct-Nov). From Table 3 it is evident that of those reporting a sharps injury, 77.3% were prescribed PEP against possible HIV-infection, however, 38.5% did not complete the course. Similarly, about 22.7% of those injured did not take PEP at all. Among participants who reported a NSI injury, students were more likely to perceive the PEP to be inadequate (70.4%) as compared to staff members (6.7%) (p<0.001).
The qualitative analysis of the responses to open ended question on the sharp injuries protocol prescribed by the training centre, the common themes were "i) difficulty with obtaining the protocol; ii) long queues to access the post-exposure prophylaxis; iii) difficulty to acquire the full course of medication on site at the dental hospital."
DISCUSSION
This study aimed at determining the prevalence and nature of needle and sharps injuries (NSI) at the Tertiary Training Oral Health Centre in Johannesburg. It does not merely cover the prevalence of NSI but also adds valuable information in terms of the sites where injuries occurred, period of injury and compliance with infection control and prevention measures. The prevalence of the NSIs was high, with 45 injuries reported among the 109 participants. Not surprisingly, the highest contributors to injuries were students as they were still in training and almost one third of students sustained at least one injury (27%). Of the 45 participants that have NSI, 16 participants had more than 1 injury per individual. Considering that there were staff members and students who did not participate in this study, the prevalence may be even higher than that reported. .
The overall NSI prevalence at this TTOHC was similar to a Taiwanese study at a teaching dental school where they reported 41% 2, but in contrast, lower than a study in the United States of American (USA) where it was much higher at 72% 3. The student NSI burden in the current study (28%) was similar to that reported at a Kenyan University at 29% 5. Conversely, another dental school in South Africa in Cape Town recorded a higher prevalence of 62% among dental undergraduates6. From the available literature , the lowest prevalence of NSI were reported in the United Arab Emirates4.
It is important that the findings are taken into cognisance considering the consequences of NSI. With the burden of blood borne disease in South Africa, all efforts should be made to provide training in the prevention of NSI, to support the students and staff subsequent to injuries in order to minimise the negative psychological impact related to the injuries10. While NSI increases the risk of exposure to blood-borne infections such as Hep B and C, it is heartening that 95% of participants are vaccinated against Hepatitis B virus, however, they still remain at risk of Hepatitis C and HV infections.
It was not surprising that students contributed most to the prevalence of needle-stick and sharps injuries. In this study, students had sustained more injuries than academic staff, which resulted in a student to staff ratio of 2.14:1. The high prevalence of needle-stick and sharps injuries (n=15; 13%) among the academic staff members could be attributed to a variety of factors which may be unique to staff members at the TTOHC. These include being a full-time educator which entails a particularly high workload of clinical supervision in addition to teaching and research responsibilities, including being personally involved in post-graduate studies. The majority of staff members reported to have been in employment for three years or less, indicating inexperience and possible uncertainty regarding their work environment. This was a factor that Lee et al (2014) strongly associated to increased fatigue resulting in a higher incidence of needle-stick and sharps injuries2. The higher NSIs among staff members confirms that dentistry as a profession has a particularly high risk of needle-stick and sharps injuries.2 It is anticipated that with increased clinical experience less needle-stick and sharps injuries would occur, as found by Lee et al , in which the annual incidence of NSI per person-year were 21.28% for interns, 7.50% for residents, 6.77% for nursing staff, 3.33% for clerks, and 0.85% for attending doctors2.
In this study the highest rate of needle-stick injuries were experienced among the dentistry students, followed by oral hygiene students, which in all likelihood can be because dental students perform more invasive procedures as compared to oral hygiene staff and students. Our findings are consistent with the Taiwanese study in which the prevalence of NSI among dentists and students was 40.9% at the National Taiwan University Hospital2.
Year of study and degree of study
The trend of needle-stick and sharps injury events among students also deviated from what was expected, as the students with more clinical experiences (Dentistry 4th year and Dentistry 5th year as well as Oral Hygiene 3rd year) sustained more injuries than the new clinical students. This could be attributed to increased level of pressure on more senior students, who have a significantly higher academic and clinical load, including increased assessment pressure.Dental students and qualified dentists and dental specialists had a higher prevalence of needle-stick and sharps injuries when compared to oral hygiene students and academic staff. It is possible that the results may be skewed by the higher number of dental staff and students, compared to oral hygiene staff and students (4.14:1). Dentists and dental students perform more invasive and surgical procedures and routinely have to use a dental syringe, which was the most common device causing NSI in this study and other studies2,6.
Time of the year
What is evident from our study is that NSI occurred most frequently during the first 3 months of the academic year and students sustained less injuries as the year progressed2. Dentistry students in their 3rd Year of study only sustained injuries in the January-March period when they first entered the clinics. Students in their 4th year of study had the most injuries 33.3 % (N=5) in the October-November period when the anxiety of the final examinations and quota demands could have played a role. This may lead to working while fatigued or rushed due to mentioned constraints. The Dentistry 5th year class, however, had more injuries in the April-June period. The findings are comparable to the findings of Lee et al where most injuries took place between July to September and mid-week from Wednesday to Fridays. July to September was their period where new dental trainees begin their clinical practice2. Among the 2nd and 3rd year oral hygiene students, only one person experienced a needle-stick injury but did not remember which time of year. Among dental staff, 50% were injured in the July-September 3-month period during which staff members are usually still marking and moderating assessments.
Dental disciplines and Departments contributing to NSIs
At the TTOHC, there are eight departments namely Prosthodontics, Rehabilitation, Periodontics and Oral Medicine, Oral Pathology, General Dental Practice, Orthodontics, Community Dentistry/Outreach and Maxillofacial and Oral Surgery. The Department of Maxillofacial and Oral Surgery was the site of most of the NSI compared to the other departments. A total of 61.9% (N=13) of these injuries were sustained by the Dentistry 4th year and Dentistry 5th year students. This observation followed the trend seen in a study by Cleveland et al. who found that more than one-third of percutaneous injuries are reported by the Oral Surgery unit13. The increased number of NSI in this department could be due to the high volume of patients seen during clinical sessions than other departments, as well as the use of a number of invasive instruments for the procedures performed. The Department of Oral Rehabilitation had the second highest occurrence of NSI reported at 38,6% (N=17). This could be attributed to the duration the procedures in this department require, for example, an endodontic procedure could last an entire two-hour session. A total of 11.4% (N=5) of the injuries were sustained in the Department of Periodontics and Oral Medicine. In the latter department there are numerous sharp instruments used in periodontal procedures. Additionally, patients in the periodontal department mostly present with inflamed gingivae leading to increased bleeding and reduced vision of the work field. The Department of Orthodontics had no needle-stick injuries reported and this is clearly attributed to the lack of sharp instruments involved during orthodontic procedures. Community outreach sites also pose a risk of injury to the students. Depending on the site where services are provided, the students may be expected to work in confined spaces which might lead to mistakes and injuries. Clinical practice in mobile dental truck has been reported to be challenging due to limited space and might lead to cross-infection.14
Instruments involved in NSI
The majority of the sustained injuries (47.6% (n=20) were caused by the needle of the dental syringe. The report is consistent with the findings of Lee et al. and may be credited to the dental syringe being used most frequently during the administration of local anaesthesia across many departments2. Scaler tips were recorded as the instrument responsible for 14.3% (n=6), which is the second most common injury. Extensive scaling procedures are usually carried out to remove staining and calculus deposits to perform a comprehensive diagnosis of tooth structures before further treatment can be administered. Fine scaling is required as part of the treatment of gingival and periodontal diseases. Injury sustained from scaler tips may occur as a result of incorrect finger rest and support during the procedure, scratching oneself against the tip when it is mounted on the controls station or during disassembly of the scalers following completion of procedures. The number of injuries caused by burs/drill bits were found to be 9.5% (N=4) which might also be sustained during mounting on similar powered hand pieces. Other reported injuries included forceps, eye splashes and from the Nabers probe and suturing needle.
Behaviour and protocol after sharps injury
The response pertaining to the PEP protocol against HIV-infection at the time of the study is of concern. In the current study, the responses to the question about PEP varied from no knowledge of what the protocol entails and where to And it, long queues when reporting the incident and obtaining the full course of antiretroviral medication on site, to the availability of nursing staff to assist in the matter.
Of the 45 NSI reports in the survey, 36 subjects reported their injuries, with only 34 commencing PEP treatment and only 23 completing the treatment. Students found the guidelines of what to do after injury and the implementation of these guideline to be inadequate, while most staff members were content that the treatment and execution of the NSI protocol was adequate. The reasons for this could be diverse, varying from inexperience with previous NSI (for many this would be the first exposure), lack of understanding of the NSI protocol amongst students, lack of authoritative privilege as compared to staff or relative inflexibility of schedules as per reports of not receiving adequate time to follow the procedure due to the students workload. The concern is that these difficulties may contribute to further underreporting, in fact, Choi et al also found in their study that the lack of reporting injuries was common due to the time it consumed to comply with the protocol11. Our findings show that 18.8% (N=8) did not report their injuries, choosing to either receive treatment privately, or not to receive treatment at all. Siddiqi et al in 2017 described the benefits of documenting needle-stick and sharps injuries6. The benefits include the effective implementation of educational programs, ensuring proper treatment post-exposure as well as assisting with the development of adequate NSI protocol.
While the PEP treatment may be adequate, a challenge with adherence was evident from responses because 39% did not complete the course. Non-compliance with HIV PEP has been attributed to the side effects associate with the afore mentioned drugs, which include diarrhoea, nausea and vomiting. Failure to complete the recommended 28 day course of ARVs reduces the efficacy of PEP treatment and increases the risk of acquiring HIV infection15 . Counselling and follow-up of injured staff and students is important in order to improve compliance.
CONCLUSION AND RECOMMENDATIONS
The hazard of NSI was found to be high at this TTOHC at 41%. It is not surprising that most injuries were among students. but what was surprising was that the more senior dental students sustained more injuries. The majority of injuries occurred in busy departments such as Maxillofacial and Restorative departments. Dental needles were reported to be the common cause of sharp injuries and most occurred around April-June as well as October-November period. The reporting rate was good however, it is concerning that less than half injured completed the PEP treatment. It is therefore necessary that counselling is conducted among the injured individuals to improve the compliance and the completion rate of PEP. Greater awareness and education are recommended at students' clinical orientation platforms and new staff clinician orientation sessions. In addition, students should be orientated with the protocol for PEP. It is also recommended that the guidelines and protocols to be followed subsequent to injuries should be made clear and posted where clearly visible. as they found it inadequate as opposed to staff. Lastly, the availability of PEP for the full 30 days should be available in-house within the TTOHC to encourage a speedy acquisition process.
ACKNOWLEDGEMENT
The authors would like to thank, V Yengopal, M Molete, M Thekiso, T Ralephenya for inputs during protocol writing. In addition, the authors would like to thank all the participants and the School Of Oral Health Sciences for providing support and an environment to conduct research.
REFERENCES
1. Himmelreich H, Rabenau HF, Rindermann M, Stephan C, Bickel M, Marzi I, et al. The management of needlestick injuries. Deutsches Ärzteblatt International. 2013;110(5):61. [ Links ]
2. Lee J-J, Kok S-H, Cheng S-J, Lin L-D, Lin C-P. Needlestick and sharps injuries among dental healthcare workers at a university hospital. Journal of the Formosan Medical Association. 2014;113(4):227-33. [ Links ]
3. Leggat PA, Smith DR, Speare R. Exposure rate of needlestick and sharps injuries among Australian veterinarians. Journal of occupational medicine and toxicology. 2009;4(1):25. [ Links ]
4. Jaber MA. A survey of needle sticks and other sharp injuries among dental undergraduate students. Int J Infect Control. 2011;7(3):1-10. [ Links ]
5. Mungure E, Gakonyo J, Mamdani Z, Butts F. Awareness and experience in needle stick injuries among dental students at the University of Nairobi, Dental Hospital. East African medical journal. 2010;87(5):211-4. [ Links ]
6. Siddiqi A, K Niazi M, De Silva H, Firth N, Konthasingha P, Zafar S. Percutaneous exposure incidents: a review of practice and awareness of current protocols at a Dental Faculty. Oral Surgery. 2017;10(4):e80-e7. [ Links ]
7. Ingole K, Pawar S, Pathak S. Needle Stick Injuries among Health Care Worker at Tertiary Care Hospital. Int J Curr Microbiol App Sci. 2016;5(12):718-25. [ Links ]
8. Hasak JM, Novak CB, Patterson JMM, Mackinnon SE. Prevalence of needlestick injuries, attitude changes, and prevention practices over 12 years in an urban academic hospital surgery department. Annals of surgery. 2018;267(2):291-6. [ Links ]
9. Coppola N, De Pascalis S, Onorato L, Calò F, Sagnelli C, Sagnelli E. Hepatitis B virus and hepatitis C virus infection in healthcare workers. World journal of hepatology. 2016;8(5):273. [ Links ]
10. Green B, Griffiths E. Psychiatric consequences of needlestick injury. Occupational medicine. 2013;63(3):183-8. [ Links ]
11. Choi LY, Torres R, Syed S, Boyle S, Ata A, Beyer TD, et al. Sharps and needlestick injuries among medical students, surgical residents, faculty, and operating room staff at a single academic institution. Journal of surgical education. 2017;74(1):131-6. [ Links ]
12. Rothe C, Schlaich C, Thompson S. Healthcare-associated infections in sub-Saharan Africa. Journal of Hospital Infection. 2013;85(4):257-67. [ Links ]
13. Cleveland JL, Barker LK, Cuny EJ, Panlilio AL. Preventing percutaneous injuries among dental health care personnel. The Journal of the American Dental Association. 2007;138(2):169-78. [ Links ]
14. Gao SS, Yon MJY, Chen KJ, Duangthip D, Lo ECM, Chu CH. Utilization of a mobile dental vehicle for oral healthcare in rural areas. International journal of environmental research and public health. 2019;16(7):1234. [ Links ]
15. Sultan B, Benn P, Waters L. Current perspectives in HIV post-exposure prophylaxis. HIV/AIDS (Auckland, NZ). 2014;6:147. [ Links ]
 Correspondence:
Correspondence:
Yolanda Malele-Kolisa
Department of Community Dentistry, School of Oral Health Sciences
University of the Witwatersrand
E-mail: Yolanda.Kolisa@wits.ac.za
Author contributions:
1 . Dr Y Malele-Kolisa 30%
2 . Dr OK Sibanyoni 15%
3 . Dr BJ Mthandazo 15%
4 . Dr TNaidoo 10%
5 . Dr H Ismail 10%
6 . Dr NT Mhlaba-van Rooyen 10%
7 . Dr N Lecoge 10%














