Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.77 no.2 Johannesburg Mar. 2022
http://dx.doi.org/10.17159/2519-0105/2022/v77no2a6
CASE REPORT
Mandibular myiasis: A case report
I AbdoolaI; MMR BouckaertII; M IbrahimIII
ILenmed Royal Hospital and Heart Centre. Previously of Department of Maxillofacial and Oral Surgery, Medunsa Oral Health Centre, Sefako Makgatho Health Sciences University (SMU), Pretoria, South Africa. ORCID: 0000-0001-9361-5407
IIMDent, FFD, FCMFOS, Professor, senior consultant: Maxillofacial and Oral Surgery, Medunsa Oral Health Centre, Sefako Makgatho Health Sciences University (SMU), Pretoria, South Africa. ORCID number: 0000-0001-9337-3671
IIIBChD, PDD (Sedation and Pain Control). Lenmed Royal Hospital and Heart Centre. ORCID number: 0000-00032548-4630
ABSTRACT
Myiasis is a condition characterised by the infestation of live vertebrates with dipterous larvae. Myiasis is derived from the Greek word mya, meaning fly. Dipterans, (order Diptera), are two-winged insects known as true flies. Myiasis tends to occur in cutaneous, necrotic lesions of patients who have weak immune systems, who inhabit unhygienic environments. Maggot Debridement Therapy is an uncommon treatment of debriding necrotic tissue, with some utility. A case of mandibular myiasis involving a malignant mandibu-lar lesion that was colonised by maggots is discussed.
Key words: Myiasis, maggot, oral, facial, infection, wound
INTRODUCTION
Myiasis is a condition characterised by the infestation of live vertebrates with dipterous larvae1. Myiasis is derived from the Greek word mya, meaning fly. Dipterans (order Diptera) are two-winged insects known as true flies2. The Old Testament was the first written account of human myiasis3. It is more common in the tropical and sub-tropical regions of Africa, Central America and South America.
CASE REPORT
A 71-year-old male patient presented with a two-month history of ulceration on the dorsum of the tongue. Three weeks prior to presentation, infection developed, the patient lost the ability of speech and the lesion became infested by maggots. On examination, the patient was cachexic and an obvious lesion on the genium was noted with associated hyperpigmented skin and maggot infestation.
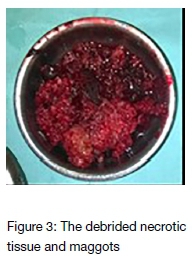
Dysmorphic, necrotic tissue was noted on the anterior aspect of the mandible extending posteriorly along the floor of the mouth. Poor hygiene and mobile teeth were salient. The lesion was debrided, a biopsy was taken, dressings were placed and the patient was prepared for admission to the hospital. Prior to being transported to the ward, the patient developed cardiac arrest. Resuscitation was attempted unsuccessfully and the patient demised. The histology confirmed a squamous cell carcinoma.


DISCUSSION
Human myiasis may be classified according to anatomical location. Cutaneous myiasis may be further classified into wound, furuncular and migratory myiasis4. Wound myiasis is the most common type encountered. The infestation of larvae in a necrotic lesion is considered to be wound, traumatic or opportunistic myiasis. Myiasis may be caused by a variety of fly species, with a particular species being either obligate, facultative or accidental parasites. Although different species may cause wound myiasis, generally only one species is found in a particular lesion1. Cutaneous lesions usually heal well, often with minimal or no scarring1. In a South African study by Kuria et al, 25 cases of wound myiasis were diagnosed over a four-year period in the Eastern Cape. The commonly encountered species leading to human myiasis are Lucilia Sericata and Lucilia Cuprina, with the latter being the most prevalent noted4. Flies may deposit larvae on clothing, soil, wounds, or on mosquitos; these act as fomites and vectors in larval transmission. Incubation periods of obligate parasites vary according to species, lasting up to 12 weeks in Dermatobia Hominis (Human Botfly) (Figure 4).
Diagnosis
Wound myiasis is usually easily diagnosed on inspection. A high clinical suspicion is warranted, especially with the history of travel to endemic areas within 12 weeks. Pain, malodorous suppuration and the sensation of movement beneath the skin may be clues to the presence of larvae. Ultrasound is a useful diagnostic tool. Identification of larvae is sufficient and biopsy may not be necessary if the underlying cause of necrosis is known1.
Risk factors
The most common predisposing factors to developing human myiasis in a South African population4 was found to be lower limb gangrene due to peripheral vascular disease, followed by burns, cancerous ulcers and diabetic ulcers. Multiple predisposing factors exist1,4, including poor hygiene, immunosuppression, old age, alcohol abuse, exposed wounds, suppurative lesions, necrotic tissue, malignant wounds, poor sanitation, poor garbage disposal and low socioeconomic status.
TREATMENT
Mechanical debridement is generally the basis of management1. Removal of necrotic tissue and larvae may be supplemented by irrigation (especially for cavities) or medication (such as Ivermectin for migratory myiasis). Debridement should be followed by meticulous wound care. Wound care and hygiene, especially of debilitated patients, should be optimal to preclude cases secondary to medical neglect.
Maggot debridement therapy (MDT)
MDT or artificially induced myiasis was commonly used in the past. MDT is the deliberate use of larvae to debride necrotic tissue, produce antimicrobial compounds and promote healing if used correctly. Use of MDT was noted in the past millennium by aborigines, Mayans and Burmese. Ambroise Pare noticed the benefit of maggots in the 1500s when a patient lost tissue equivalent to the volume of a hand through an infection involving the skull and recovered. Maggots were used during World War I to debride wounds and were noted to improve recovery.
The perceived distasteful nature of the treatment led to a period of disuse. Justified by contemporary research, a recent surge has been noted in the use of maggot de-bridement therapy in selected patients with long-standing wounds that persist despite attempts of conventional treatment. Contraindications include the presence of large vessels, vital structures or hollow organs near the wound. The larvae of the Green Bottle Housefly (Lucilia Sericata) are the most commonly used species in these cases3. Maggots effectively and selectively debride necrotic tissue and due to their photophobic nature, will debride regions where surgical access may otherwise be challenging1. Larvae used in MDT produce agents similar to antibiotics, alkalinize wounds by secreted ammonia, ingest bacteria and produce substances that promote wound healing3. Larvae must be prepared in a sterile manner for MDT use and removed after a maximum of three days1,5.
Declaration
No sources of funding or financial interests are applicable. This article has not been previously published.
Acknowledgements
Many thanks are due to the Department of Maxillofacial and Oral Surgery, SMU and to Lenmed Royal Hospital and Heart Centre
Conflict of interest
No conflicts of interest
References
1. Francesconi F, Lupi O. Myiasis. Clin Microbiol Rev. 2012; 25 (1): 79-105 [ Links ]
2. Oldroyd H. Dipteran [internet]. Britannica [cited 2020 December 30]. Available from: https://www.britannica.com/animal/dipteran [ Links ]
3. Whitaker IS, Twine C, Whitaker MJ, Welck M, Brown CS, Shandall A. Larval therapy from antiquity to the present day: mechanisms of action, clinical applications and future potential. Postgrad Med J. 2007; 83(980): 409-413. [ Links ]
4. Kuria SK, Kingu HJC, Villet MH, Dhaffala A. Human myiasis in rural South Africa is under-reported. SAMJ. 2015; 105(2): 129-133. [ Links ]
5. Donnelly J. Wound healing--from poultices to maggots. (A short synopsis of wound healing throughout the ages). Ulster Med J. 1998; 67(1): 47-51. [ Links ]
6. Derraik JGB, Heath A, Rademaker M. Human myiasis in New Zealand: imported and indigenously-acquired cases: the species of concern and clinical aspects. NZ Med Jour.2010; 123: 21-38. [ Links ]
 Correspondence:
Correspondence:
I Abdoola
Suite 106, Lenmed Royal Hospital and Heart Centre, 6 Welgevonden
Street, Royldene, Kimberley, 8301
E-mail: maxfax@dr.com
Tel: 053 045 0532/3
The role played and the respective contribution:
1 . I Abdoola: Writing article, data collection, data analysis - 50%
2 . MMR Bouckaert: Corrections - 25%
3 . M Ibrahim: Data analysis, researching relevant related articles - 25%














