Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.77 n.2 Johannesburg Mar. 2022
http://dx.doi.org/10.17159/2519-0105/2022/v77no2a2
RESEARCH
Comparison of capsule-mixed versus hand-mixed glass ionomer cements Part II: Porosity
S ArnoldI; G D BuchananII; N WarrenIII; N PotgieterIV
IBChD, PGDip (Endo), MSc (Dent). Department of Odontology, School of Dentistry, Faculty of Health Sciences, University of Pretoria, 31 Bophelo Road, Prinshof Campus, Riviera, Pretoria, 0002, South Africa. ORCID 0000-0002-7518-9560
IIBChD, PGDip (Endo), MSc (Dent). Department of Odontology, School of Dentistry, Faculty of Health Sciences, University of Pretoria, 31 Bophelo Road, Prinshof Campus, Riviera, Pretoria, 0002, South Africa. ORCID 0000-0003-2957-166X
IIIBChD, PGDip (Endo), MSc (Dent). Department of Odontology, School of Dentistry, Faculty of Health Sciences, University of Pretoria, 31 Bophelo Road, Prinshof Campus, Riviera, Pretoria, 0002, South Africa. ORCID 0000-0003-1006-9565
IVBChD, PGDip (Endo), PGDip (Paedo), MSc (Dent)2 Paediatric Dentistry, University of the Western Cape, Robert Sobukwe Road, Bellville, Cape Town, 7535. ORCID 0000-0003-4016-3322
ABSTRACT
INTRODUCTION: Glass ionomer restorative cements (GIC) are routinely used in dental practice. During mixing, air incorporation may lead to higher porosity with subsequent weakening of the cement. The degree of porosity will determine whether capsule-mixed or hand-mixed GIC are mechanically stronger for clinical use
AIM: To compare the porosity of four commercially available dental glass ionomer cements, supplied in both hand-mix and capsule-mix formulations, by evaluating number of voids (%), total volume of voids (mm3) and volume percentage of voids (%
METHODS: Eighty samples were manufactured from hand-mixed GIC: Riva Self Cure; Fuji IX GP ; Ketac Universal, Ketac Molar Easymix, and equivalent capsule-mixed GIC: Riva Self Cure; Fuji IX GP ; Ketac Universal Aplicap and Ketac Molar Aplicap. Micro-CT scanning was used to evaluate porosity. The number of voids (mm3), total volume of voids (mm3) and the volume percentage of voids (%) were calculated
RESULTS: Riva Self Cure Capsules showed significantly less volume of voids (P = 0.005) and volume percentage of voids (P = 0.005) than Riva Self Cure hand-mixed. Fuji IX GP hand-mixed showed a higher number of voids (P < 0.001), but lower volume and volume percentage of voids (P < 0.001) when compared to Fuji IX GP capsules. The number of voids (P < 0.001), volume of voids (P = 0.004) and volume percentage of voids (P = 0.004) were significantly lower for both Ketac Universal and Ketac Molar capsules versus their hand-mixed equivalents
CONCLUSION: Three capsulated forms of glass ionomer cements (Riva Self Cure, Ketac Universal and Ketac Molar) demonstrated decreased porosity, and may therfore be advantageous for clinical application
Key words: Glass ionomer cement, Capsule-mix, Handmix, Micro-CT, Porosity
ABBREVIATIONS FOR ARTICLE
• GIC - Glass Ionomer cement
• FIXC - GC Fuji IX GP capsule-mix
• FIXH - GC Fuji IX GP hand-mix
• RSCC - Riva Self Cure capsule-mix
• RSCH - Riva Self Cure hand-mix
• KUC - Ketac Unversal Aplicap capsule-mix
• KUH - Ketac Universal hand-mix
• KMC - Ketac Molar Aplicap capsule-mix
• KMH - Ketac Molar Easymix hand-mix
• mm3 - cubic millimetre/s
• °C - degrees Celsius
• % - percentage
• rpm - revolutions per minute
• MIDRAD - Micro-focus X-ray Tomography Facility
• NECSA - South African Nuclear Energy Corporation
• SD - Standard deviation
• IQR - interquartile range
INTRODUCTION
Restorative dentistry concepts have changed over the years, with a modern focus on minimally invasive cavity preparation and the placement of adhesive restorative materials capable of re-mineralizing demineralized tooth structure.1,2 Public demand for a non-metallic aesthetic restorations has also increased.3 Glass lonomer cements have been developed to fulfil these requirements due to their unique material properties, which include chemical bonding to tooth structure, setting with an acid base reaction and fluoride release.4 The applications of glass ionomer cements include: the restoration of primary teeth; class lll and V restorations on permanent teeth; intermediated restorations; liners/ bases in the 'Sandwich technique'; the 'Art technique'; pit and Assure sealing and luting of indirect prosthesis.5 Modern high viscosity glass ionomer cements like Ketac Universal, are now indicated for restricted stress-bearing Class I and restricted stress-bearing and non-stress-bearing Class II permanent restorations on permanent teeth.6
Glass ionomer cements consist of a mixture of calcium- or strontium-alumino-flouro-sillicate glass powder combined with a water-soluble polyalkenoic acid.7 Two forms of glass ionomer cements are commercially available from dental material manufacturers. The first is a glass powder and separate polyalkenoic acidic liquid that is mixed by hand.8,9 The second are the capsulated formulations, which require mixing in mechanical mixing triturators.9
Capsulation of glass ionomer cements offer several advantages over hand-mixed materials, these include: a pre-proportioned powder: liquid ratio, standardised mixing technique and times,8,10 user friendliness and time efficiency.6,11 The mixed cement can additionally be immediately injected into a cavity preparation directly from the capsule.12 Dowling and Flemming8 have advocated the clinical use of capsule-mixed glass ionomer cement with respect to the superior mechanical properties and as a solution to the problem of operator-induced variability (i.e. the variation between two or more individuals performing the same task, e.g. mixing dental materials) of hand-mixed materials.8
Several studies have however shown that the vibratory action of conventional mechanical mixing triturators may lead to increased porosity of set capsulated glass ionomers cements when compared to their hand-mixed equivalents, leading to weakening of the cement.13,14 Mechanical mixing triturators with a combined rotational and centrifugal action have been advocated by some manufacturers and researchers to reduce porosity and void formation.8,15 This recommendation has been debated, with Fleming et al.15 and Dowling and Fleming8 suggesting that these types of mixing triturators may not necessarily confer additional benefits as compared to conventional machines.
Porosity within glass ionomers acts as a source of stress concentration, negatively affecting the strength and homogeneity of the material.12,16,17 Voids or porosity may be incorporated into a mixture by either air entrapment or inadequate wetting of the powder by the liquid.12 Large voids have been reported to be responsible for material failure at low stress levels.12
The published literature shows conflicting evidence as to whether capsule-mixed or hand-mixed glass ionomers demonstrate increased porosity.18 Mitchell and Douglas14 evaluated the porosity of hand-mixed and capsule-mixed glass ionomer luting cements and found hand-mixed cements to contain more voids and voids of a larger diameter than the capsule-mixed equivalents.14 Kaushik et al. however reported the opposite,16 in their investigation hand-mixed glass ionomers demonstrated fewer voids per surface area as compared to the equivalent capsule-mixed versions.
AIM AND OBJECTIVES
The present study aimed to compare the porosity of four commercially available dental glass ionomer cements, supplied in both hand-mix and capsule-mix formulations. The objectives were to evaluate differences in number of voids (mm3), total volume of voids (mm3) and the percentage of voids (%) using Micro-CT assessment of the set materials following different mixing methods.
MATERIALS AND METHODS
Ethical approval for this in vitro, comparative study was obtained from the Ethics Committee of the Faculty of Health Sciences, University of Pretoria (protocol number: 206/2017).
The materials included for use in this study were: RivaSelf-Cure Hand-mix (RSCH, SDI Ltd., Victoria, Australia); Fuji IX-GP Hand-mix (FIXH, GC, Tokyo, Japan); Ketac-Universal Hand-mix (KUH, 3M, St. Paul, MN); and Ketac-Molar-Easymix Hand-mix (KMH, 3M, St. Paul, MN). Four equivalent capsule-mixed glass ionomers: Riva-Self-Cure Capsules (RSCC, SDI Ltd., Victoria, Australia); GC Fuji-IX GP Capsules (FIXC, GC, Tokyo, Japan); Ketac-Universal Aplicap Capsules (KUC, 3M, St. Paul, MN) and Ketac-Molar Aplicap Capsules (KMC, 3M, St. Paul, MN) were also included for comparison between hand- and capsule-mixed products.
The respective manufacturer's instructions were strictly adhered to at all times during the mixing and preparation of all specimens/ materials evaluated in this study, and are described in detail hereafter. The research was performed in a controlled environment as recommended by the manufacturers. The room temperature was 23 +/- 1°C and relative humidity 50 +/- 5%.15,19 All materials were mixed and dispensed in polytetrafluoroethylene (PTFE) moulds with the following internal dimensions: six millimetres in height and four millimetres in diameter.8,20 The moulds were constructed from PTFE tubing and supported by custom-made Perspex® blocks.12 Cylindrical material specimens were prepared by two dentists with the same level of training, to simulate operator variability.21,22 Ten specimens in capsule-mix and 10 specimens in hand-mix were manufactured for each chosen material.
The FIXC were shaken to loosen the powder before activation.23 All capsules were activated for two seconds to break the membrane separating the powder and liquid components.8,15,23 The capsules were thereafter immediately placed into a mechanical mixing machines. The 3M ESPE capsule materials were mixed in the RotomixTM triturator (3M ESPE, United Kingdom) as by manufacturer's instruction. The triturator was set to an eight second vibratory action and an additional three seconds centrifuging action at 2950 rpm frequency.8,12,15
All other capsules were mixed in an amalgamator (Amalgamator SYG 200, SMACO, Switzerland) for 10 seconds vibratory action.8,15 Immediately after mixing, each capsule was placed in an appropriate applicator to facilitate the extrusion of the glass ionomer restorative material.8,15 The hand-mixed equivalents were mixed on a waxed-paper mixing pad using the scoop and dropper systems provided to measure accurate quantities.22 To simulate clinical practice, the powder and liquid quantities for the hand-mixed materials were intentionally not weighed.
The moulds were placed on a polyester strip in the Perspex® matrix. Mixed cement was dispensed into the moulds within 60 seconds.12,20,21 The capsulated glass ionomers were extruded slowly to provide laminar flow and minimise the incorporation of bubbles with the nozzle positioned to one side of the mould.8,21,24 The hand-mixed materials were applied to the moulds within 60 seconds using a stainless steel spatula and allowed to flow to minimise the incorporation of air bubbles.8,20 A second polyester strip was thereafter placed over the filled moulds.
Both the capsulated and hand-mixed materials were gently compressed using a glass slab with a weight of 60 g25 and slight pressure to extrude the excess material and flatten the surface.5,17,19,21,25-29
Coatings were applied for FIX, RSC and KM specimens and omitted for KU specimens according to manufacturers' instructions. All specimens were thereafter placed in distilled water in glass containers maintained at 37+/- 1°C in an incubator (Binder ED23, Tuttlingen, Germany) for a period of one hour.12,20,21 After one hour, 880 grit silicon carbide paper was used under running water to remove surplus cement at the top and bottom of the moulds.12 Each specimen was carefully removed from the moulds and stored in glass containers with 50 ml distilled water at 37°C. for 23 hours. Testing of the specimens commenced 24 hours after manufacturing.20,21,30 Any specimens with visible defects such as bubbles or cracks, were discarded.20,21
Porosity evaluation
The XTH 225kV micro-focus X-ray/CT system (Nikon Metrology, Leuven, Belgium) situated at the micro-focus X-ray radiography/tomography facility (MIXRAD) of the South African Nuclear Energy Corporation (NECSA), Pelindaba, South Africa was used for porosity testing. The system has an intrinsic spatial resolution volume ranging from 0.001-0.006 mm. The manipulator allowed for horizontal optimization to ensure maximum amplification of the samples. To convert 2D projections into 3D volumes, CT-Pro reconstruction software (Nikon XT software, USA) was used. CT-Pro 3D raw volume files were imported into VGStudioMax software (High-End Industrial CT Software, Heidelberg, Germany) allowing for the recovery and reconstruction of the X-rays into pinpoint sharp 3D-virtual images.
The number of voids per volume (n), the total volume of voids (mm3) per volume and the volume percentage of voids (%) per volume of each specimen were determined.14 The measured volume of each specimen was pre-set at 60,054688 mm3. Voids greater than 0.001 mm3 were included in the present study as these are considered to be significantly large.14
Statistical analysis
Statistical analysis was performed using SAS (SAS Institute Inc, Carey, NC, USA), release 9.4, running on Microsoft windows for personal computer. The applied statistical tests, two-sided and P values less than 0.05, were considered significant. Mean values for number of voids per volume (n), total volume of voids (mm3) and volume percentage of voids (%) were compared using the two-sample t-test. Thus any significant differences between the means of the paired test groups could be determined. The non-parametric Wilcoxon Rank-Sum test was used to compare the median values of the paired groups.
RESULTS
The number of voids per volume of the tested materials are reported in Table I.
No significant differences regarding the number of voids between the RSCH- and RSCC- paired groups (mean, P = 0.221; median P = 0.199) or the FIXH- and FIXC- paired groups (mean, P = 0.210; median P = 0.545) were found. The number of voids present in the KUH- and KUC- paired group differed by mean values of 12183.6, which was statistically significant (P < 0.001). The median values of the two groups also varied by 13694 (P = 0.002). Significant differences regarding the number of voids between the KMH- and KMC- paired group mean values (6699.8, P = 0.001) and median values (6666.5, P = 0.007), were also found.
The volume of voids per volume of the tested materials are reported in Table II.
Three of the four hand-mixed materials RSCH (P = 0.005), KUH (P = 0.004) and KMH (P = 0.010) demonstrated a significantly higher mean total volume of voids when compared to the respective capsule-mixed materials (RSCC, KUC and KMC).
The FIXH- and FIXC- paired group also demonstrated significant differences in both the mean and median volume of voids (P < 0.001), however the hand-mixed material (FIXH) displayed a lower total volume of voids as compared to the capsule-mixed material (FIXC). The volume percentage of voids (%) per volume of all materials are reported in Table III. Three of the four hand-mixed materials RSCH (P = 0.005), KUH (P = 0.004) and KMH (P = 0.010) demonstrated a significantly higher volume percentage of voids when compared to the respective capsule-mixed materials (RSCC, KUC and KMC). The FIXH- and FIXC- paired group also demonstrated significant differences in both the mean (P < 0.004) and median volume percentage of voids (P < 0.006), with the hand-mixed material (FIXH) displaying a lower total volume percentage of voids when compared to the capsule-mixed material (FIXC).
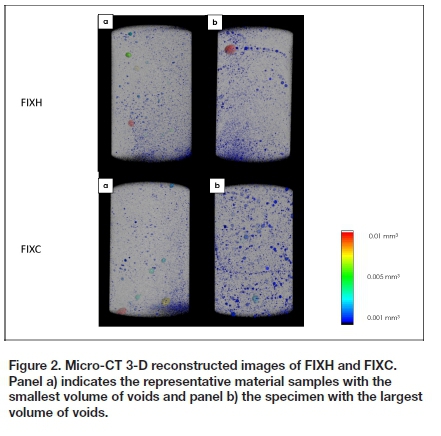
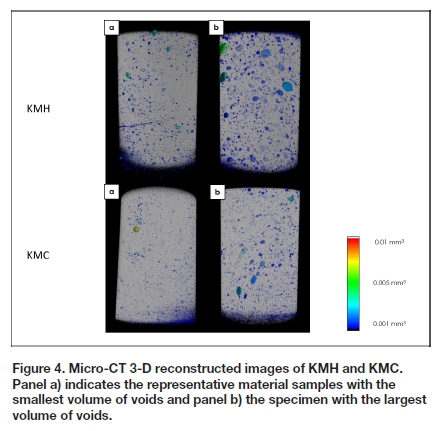
Micro-CT reconstructed 3D images providing a comparative visual indication of the number, size, volume and distribution of voids can be seen in Figures 1, 2, 3 and 4. The images selected for each material were made according to representative material samples displaying the smallest and largest volume of voids.


DISCUSSION
Testing and comparison of the mechanical properties of glass ionomers may have important clinical considerations as the mechanical properties of these materials, such as porosity and the presence of voids, may provide an indication of their long-term durability and wear resistance.31 Micro-CT scanning allows for the non-invasive charting and evaluation of the microstructure of dental materials in three dimensions by producing high resolution images and rapid data acquisition.13,32 Previous studies on glass ionomer cements by Nomoto et al.13 and Chen et al.33demonstrated Micro-CT scanning to be highly effective to evaluate material properties. To the authors' knowledge, this is the first study evaluating porosity in set Riva Self Cure and Ketac Universal samples utilizing Micro-CT technology.
Small air inclusions, dispersed throughout the entire mass of the cement, were observed in all the scanned glass ionomers cements specimens examined in this study.
Larger air inclusions were also observed and these may be of clinical significance as they may contribute to material failure at lower stress forces and have a negative effect on the performance of the set material.13
Hand-mixing of higher viscosity glass ionomer cements should ideally produce an even diffusion of unreacted glass fillers throughout the plastic mass. However, if inadequate spatulation force is used during mixing, clumps of unreacted glass filler powder may form instead of an even diffusion of powder particles. Fleming and Zala previously identified such powder clumps in hand-mixed glass ionomer materials,18 and reported that cracks or fractures of the set material will most likely commence from these sites.18
Fleming et al.20suggested that porosity may be introduced during hand-mixing of glass ionomer cements when a greater volume of powder is added to the liquid than that recommended by manufacturers. Greater powder volume necessitates increased pressure during spatulation to sufficiently mix the material, potentially leading to greater porosity of the end product.20 It has been demonstrated that the use of a lower than recommended powder-to-liquid volume will result in reduced porosity, however this modification negatively affects the strength of the cement due to the lower concentration of reinforced glass filler particles in the set product.20 Dowling and Fleming8 suggested the powder content of glass ionomers routinely used in clinical practice may be as low as 50% of manufacturer's recommendations,8 which could have substantial clinical implications.
No significant differences were found between the number of voids between the RSCH and RSCC specimens tested. However, the volume of voids and volume percentage differed significantly. This finding suggests that capsulated RSC may be beneficial for clinical use considering the reduction in porosity.
FIXC demonstrated significantly higher values for volume and volume percentage of voids as compared to FIXH. These findings could possibly be explained by operator induced variability which has been demonstrated to affect porosity during the mixing of glass ionomer cements.20 During the present study, utmost care was however taken to accurately measure the powder and liquid volumes and mixing was completed according to manufacturer's recommendations. Kausnik et al.16reported capsule-mixed restorative glass ionomer cements to contain more voids per volume than hand-mixed products. Conventional mixing machines, without additional centrifugation, as used with FIXC materials, may be responsible for the increased porosity found in some capsulated glass ionomer cements (Figure 2).18 The results of the present study support this finding.
Al-Kadhim et al.34compared hand-mixed and capsule-mixed glass ionomer luting cement and reported the capsule-mixed material to have larger voids and an increased volume of voids as compared to the hand-mixed equivalents. The decreased viscosity of glass ionomer luting cements as compared to restorative glass ionomer cements may be responsible for this finding. This assertion is supported by the findings of Nomoto and McCabe,12 who demonstrated conventional mechanical mixing to introduce a type of foam or frizz in low-viscosity cement.
The 3M materials (KUC and KMC) were mixed according to manufacturer's instructions using a RotomixTM mechanical triturator. The reduced volume of voids and volume percentage of voids of the 3M materials tested in the present study may be attributed to the added centrifugal action of the RotomixTM triturator when mechanically mixing these products. Centrifuging has been shown to move air bubbles to the surface, allowing the air to "break out" before mixing is completed.18 Studies have demonstrated that the added centrifugal action may only be beneficial for some cements and that performance is dependent on the initial viscosity of the cement mass.12,18 Glass ionomer cements mixed in the RotomixTM show decreased working and setting times due to prolonged mixing caused by centrifuging after rotation.18 Issa et al. 35 examined the extrusion force, surface pH (indicating homogeneity), and porosity of capsulated glass ionomer cement when mixed with the RotomixTM, by hand and or with a conventional amalgamator and found the RotomixTM to be beneficial when the examined properties were compared. A future study specifically aimed at using the Rotomix™ for mixing all the capsulated test glass ionomer materials used in the present study, may provide valuable information and more conclusive results.
A solution to reduce porosity in glass ionomer cements, using applied ultrasonic excitation, was suggested by Coldebella et al.25In their study, ultrasonic excitation decrease the size and number of voids in tested materials.25 High-vibration frequency caused the voids to collapse during the mixing process.25 Ultrasonic wave application may therefore improve the setting reaction between the glass particles and the polyacid, and break up powder particle clusters formed.25 Higher compressive strength and surface hardness, and increased bonding to enamel have been documented when ultrasonic vibration was applied to glass ionomer cement during the early setting reaction.25
CONCLUSION
Significant differences in the porosity of glass-ionomer cements were found between the hand-mixed and capsule-mixed equivalents tested in the present study. The results demonstrate that the method of mixing may significantly influence the porosity of dental glass ionomer cements. The results for FIX were inconclusive as to whether the capsule-mix or the hand-mixed materials are superior in terms of porosity. With reference to the RSCC, KUC and KMC materials, capsule-mixing resulted in significantly lower porosity than hand-mixing when the number, total volume and volume percentage of voids were compared. These findings suggest capsule-mixing to be advantageous as compared to hand-mixing regarding the porosity of these materials. A related research study by the authors, 'Comparison of capsule-mixed versus hand-mixed glass ionomer cements, Part 1: compressive strength and surface hardness', supports the conclusion that capsulated glass ionomer cements could be superior to their hand-mixed counterparts.
Acknowledgements
The South African Division of the IADR contributed to this research by awarding funds from the Cornelius Pameijer Fellowship. The University of Pretoria, Faculty of Health Sciences provided funds to purchase the 3M ESPE glass ionomers. GC South Africa donated the GC glass ionomers and Wright-Millners, South Africa donated the SDI glass ionomers. The materials used in this study were provided with no prerequisites or terms and conditions for material assessment. The authors declare that there are no conflicts of interest in this study. The authors do not have any financial interest in the companies whose materials were included in this manuscript.
Conflict of interest
The authors declare that they have no conflict of interest related to any aspect of this research project.
REFERENCES
1. Cho S, Cheng AC. A review of glass ionomer restorations in the primary dentition. J Can Dent Assoc. 1999; 65:491-5. [ Links ]
2. Seemann R, Flury S, Pfefferkorn F, Lussi A, Noack MJ. Restorative dentistry and restorative materials over the next 20 years: A delphi survey. Dent Mater. 2014; 30(4):442-8. [ Links ]
3. Browning WD. The benefits of glass ionomer self-adhesive materials in restorative dentistry. Compend Contin Educ Dent. (Jamesburg, NJ: 1995). 2006; 27(5):308-14; quiz 15-16. [ Links ]
4. De Moor RJ, Verbeeck RM, De Maeyer EA. Fluoride release profiles of restorative glass ionomer formulations. Dent Mater. 1996; 12(2):88-95. [ Links ]
5. Salinovic I, Stunja M, Schauperl Z, Verzak Z, Malcic AI, Rajic VB. Mechanical properties of high viscosity glass ionomer and glass hybrid restorative materials. Act Stomato Croa. 2019; 53(2):125-31. [ Links ]
6. 3M ESPE Deutschland GmbH [Internet]. Product specification for Ketac Universal Aplicap. 3m ESPE Germany Online Resources I [Internet] http://multimedia.3m.com/mws/media/1090408O/ketac-universal-aplicap-technical-product-profile-pdf.pdf [updated 16 Aug 2016; cited 2019 24 July]. [ Links ]
7. Croll TP, Nicholson J. Glass ionomer cements in pediatric dentistry: Review of the literature. Pediatr Dent. 2002; 24(5):423-9. [ Links ]
8. Dowling AH, Fleming GJ. Are encapsulated anterior glass-ionomer restoratives better than their hand-mixed equivalents? J Dent. 2009; 37(2):133-40. [ Links ]
9. Wilson AD, Nicholson JW. Acid-base cements: Their biomedical and industrial applications: Cambridge University Press; 2005. [ Links ]
10. Dowling AH, Fleming GJ. Is encapsulation of posterior glass-ionomer restoratives the solution to clinically induced variability introduced on mixing? Dent Mater. 2008; 24(7):957-66. [ Links ]
11. 3M ESPE Canada [Internet]. Product specification for Ketac Molar Quick Aplicap. 3m ESPE Canada Multimedia Online Resources I [Internet] https://multimedia.3m.com/mws/media/296110O/3m-ketac-molar-quick-aplicap-glass-ionomer-filling-material.pdf [updated 19 Jan 2012; cited 2019 15 August]. [ Links ]
12. Nomoto R, McCabe JF. Effect of mixing methods on the compressive strength of glass ionomer cements. J Dent. 2001; 29(3):205-10. [ Links ]
13. Nomoto R, Komoriyama M, McCabe JF, Hirano S. Effect of mixing method on the porosity of encapsulated glass ionomer cement. Dent Mater. 2004; 20(10):972-8. [ Links ]
14. Mitchell C, Douglas W. Comparison of the porosity of hand-mixed and capsulated glass-ionomer luting cements. Biomater. 1997; 18(16):1127-31. [ Links ]
15. Fleming GJ, Kenny SM, Barralet JE. The optimisation of the initial viscosity of an encapsulated glass-ionomer restorative following different mechanical mixing regimes. J Dent. 2006; 34(2):155-63. [ Links ]
16. Kaushik M, Sharma R, Reddy P, Pathak P, Udameshi P, Vallakuruchi Jayabal N. Comparative evaluation of voids present in conventional and capsulated glass ionomer cements using two different conditioners: An in vitro study. Int J Biomater. 2014; 2014(Article ID 935240):1-5. [ Links ]
17. Xie D, Brantley W, Culbertson B, Wang G. Mechanical properties and microstructures of glass-ionomer cements. Dent Mater. 2000; 16(2):129-38. [ Links ]
18. Fleming G, Zala D. An assessment of encapsulated versus hand-mixed glass ionomer restoratives. Oper Dent. 2003; 28(2):168-77. [ Links ]
19. McKinney J, Antonucci J, Rupp N. Wear and microhardness of glass-ionomer cements. J Dent Res. 1987; 66(6):1134-9. [ Links ]
20. Fleming GJ, Farooq AA, Barralet JE. Influence of powder/liquid mixing ratio on the performance of a restorative glass-ionomer dental cement. Biomater. 2003; 24(23):4173-9. [ Links ]
21. Fleming GJ, Dowling AH, Addison O. The crushing truth about glass ionomer restoratives: Exposing the standard of the standard. J Dent. 2012; 40(3):181-8. [ Links ]
22. Billington R, Williams J, Pearson G. Variation in powder/ liquid ratio of a restorative glass-ionomer cement used in dental practice. Br Dent J. 1990; 169(6):164-7. [ Links ]
23. GC America [Internet]. Operatory instructions for GC Fuji IX GP capsules. GC America Online Resources I [Internet] http://www.gcamerica.com/products/operatory/GC_Fuji_IX_GP/325282-GCFujiIXGP-IFU4L.pdf [updated 5 Apr 2019; cited 2019 16 September]. [ Links ]
24. Baig MS, Dowling AH, Fleming GJ. Hertzian indentation testing of glass-ionomer restoratives: A reliable and clinically relevant testing approach. J Dent. . 2013; 41(11):968-73. [ Links ]
25. Coldebella CR, Santos-Pinto L, Zuanon ACC. Effect of ultrasonic excitation on the porosity of glass ionomer cement: A scanning electron microscope evaluation. Microsc Res Tech. 2011; 74(1):54-7. [ Links ]
26. Ban S, Hasegawa J, Anusavice K. Effect of loading conditions on bi-axial flexure strength of dental cements. Dent Mater. 1992; 8(2):100-4. [ Links ]
27. Menne-Happ U, Ilie N. Effect of heat application on the mechanical behaviour of glass ionomer cements. Clin Oral Investig. 2014; 18(2):643-50. [ Links ]
28. Yap A, Cheang P, Chay P. Mechanical properties of two restorative reinforced glass-ionomer cements. J Oral Rehabil. 2002; 29(7):682-8. [ Links ]
29. Zoergiebel J, Ilie N. Evaluation of a conventional glass ionomer cement with new zinc formulation: Effect of coating, aging and storage agents. Clin Oral Investig. 2013; 17(2):619-26. [ Links ]
30. Prentice LH, Tyas MJ, Burrow MF. The effect of mixing time on the handling and compressive strength of an encapsulated glass-ionomer cement. Dent Mater. 2005; 21(8):704-8. [ Links ]
31. Hamid DMA, Mahmoud GM, El-Sharkawy FM, Auf EAA. Effect of surface protection, staining beverages and aging on the color stability and hardness of recently introduced uncoated glass ionomer restorative material. Fut Dent J. 2018; 4(2):288-96. [ Links ]
32. Hoffman JW, De Beer F, editors. Characteristics of the micro-focus x-ray tomography facility (mixrad) at necsa in south africa. 18th World Conference on Nondestructive Testing; 2012. [ Links ]
33. Chen X, Cuijpers V, Fan M, Frencken J. Marginal leakage of two newer glass-ionomer-based sealant materials assessed using micro-ct. journal of dentistry. 2010; 38(9):731-5. [ Links ]
34. Al-Kadhim A, Abdullah H, Mahmood A. Effect of porosity on compressive strength of glass ionomer cements. Malays Dent J. 2012; 34(1):23-9. [ Links ]
35. Issa M, Brunton P, Silikas N, Watts D. Expulsion force, surface ph, and porosity of encapsulated glass-ionomer cements mixed with a rotomix device. Eur J Prosthodont Restor Dent. 2002; 10(3):119-23. [ Links ]
 Correspondence:
Correspondence:
Samantha Arnold
E-mail: samantha.arnold@up.ac.za
Telephone: +27 12 319 2559 / 084 521 2429
Author contributions:
1 . Samantha Arnold - 40%
2 . Glynn D. Buchanan - 25%
3 . Nichola Warren - 20%
4 . Nicoline Potgieter - 15%














