Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Dental Journal
versión On-line ISSN 0375-1562
versión impresa ISSN 0011-8516
S. Afr. dent. j. vol.77 no.2 Johannesburg mar. 2022
http://dx.doi.org/10.17159/2519-0105/2022/v77no2a5
RESEARCH
Oral antibiotic prescription patterns for dental conditions at two public sector hospitals in Pietermaritzburg, KwaZulu-Natal
P RamnarainI; S SinghII
IBDT, BDS, M.Sc (Dental Therapy). Discipline of Dentistry, School of Health Sciences, Unversity of KwaZulu-Natal, Durban, South Africa. ORCID: 0000-0003-0428-201X
IIB. Oral Health, PG Dip (Health Research Ethics), M.Sc (Dentium), PhD. Discipline of Dentistry, School of Health Sciences, University of KwaZulu-Natal, Durban, South Africa.ORCID: 0000- 0003-4842-602X
ABSTRACT
INTRODUCTION: Antibiotic resistance is a growing public health concern. Yet, there is a paucity of published data in KwaZulu-Natal on antibiotic prescription trends and patterns related to dental use.
STUDY OBJECTIVES: The objectives of this study were to identify the range of dental conditions for which oral antibiotics are prescribed at two public health settings (Institution A and B) in the Pietermaritzburg Complex, KwaZulu-Natal and to explore practitioner understanding of the indications for antibiotic prescription for dental conditions.
METHODS: The study used a two-phased approach and collected a combination of qualitative and quantitative data. Phase 1 comprised a retrospective clinical chart review (n=720), while phase 2 comprised a focus-group discussion with purposively selected health care practitioners at each institution.
RESULTS: The results of the retrospective clinical chart review indicated that dental abscesses were the most common dental infections requiring oral antibiotic therapy (n= 479; 66%), followed by acute alveolar osteitis (dry socket) (n=110; 15%), dental impactions (n=78; 11%) and dental extractions (n=62; 9%). At Institution A, antibiotic therapy was prescribed for conditions such as trismus (n=13; 6%), soft palate swelling of unspecified origin (n=9; 4%), fibrous epulis (n=6; 3%) and acute herpes simplex (n=2; 1%). Interestingly, antibiotics were not prescribed at Institution B for the same dental conditions. Antibiotic therapy was also prescribed for eruption pain (n=4; 1%) and for cases when patients did not bring their inhaler for asthma treatment (pump) (n=3; 1%). The findings from the focus-group discussions suggested that there is a need to improve practitioner understanding of the indications for antibiotic prescriptions for dental conditions.
CONCLUSION: This study showed some differences in antibiotic therapy prescription patterns at the two public health institutions, especially for dental conditions that did not require such management. This suggests a need for consensus-building among health professionals and the provision of more dedicated guidance for antibiotic prescription in the management of dental conditions.
INTRODUCTION
Antimicrobial resistance is a global threat, it is estimated that 700 000 people die annually as a result of antimicrobial resistance.1 By 2050, this figure is set to escalate to 10 million.2 The reported indiscriminate or inappropriate use of antibiotics for dental conditions requires a review, specifically in light of the proliferation of resistant bacterial strains that could lead to antibiotic resistance.3 There is an unclear picture of antimicrobial consumption rates as well as discrepancies in antibiotic prescriptions across different countries.4 Despite adequate knowledge of appropriate antibiotic use, health care practitioners in Australia still over-prescribe, while dentists in Switzerland are cautious and unsure about prescribing antibiotics.5
From a South African perspective, Mthethwa et al. reported that oral health care practitioners lack adequate knowledge of the available treatment guidelines and best practices related to prescribing antibiotic prophylaxis.6 A more recent study reported that antibiotic prescribing patterns by dentists following tooth extraction did not appear to follow a consistent or coherent set of guidelines for antibiotic use.3 Despite the availability of several clinical practice guidelines on the use of systemic antibiotics to treat pulpal and peri-apical infections 7, there is very little published evidence on antibiotic- prescribing practices of dentists in South Africa.8
The South African Antibiotic Stewardship Programme was developed in 2012 in response to the general identified gap in antibiotic prescription trends and patterns in health care. Its purpose is to implement antibiotic stewardship programmes in hospitals and primary health care facilities.9 The aim of this programme is to 'strengthen the antimicrobial surveillance, ensure uninterrupted access to quality essential medicines, to enhance infection prevention and control and to stimulate further research innovations'.4 Antimicrobial prescribing practices in the public sector in South Africa are also guided by the Standard Treatment Guidelines and the Essential Medicines List 2020.10 These documents are available electronically (http://www.kznhealth.gov.za/pharmacy/PHC-STG-2020.pdf) and is a valuable resource to guide practitioners on antibiotic prescriptions.4,11,12 A properly developed antibiotic surveillance programme coupled with clearly defined protocols for the judicious prescription of antibiotics can collectively contribute to delays in the emergence of resistant bacteria.1 Adherence to the Standard Treatment Guidelines and the South African Antibiotic Stewardship Programme can also contribute to the reduction of inappropriate antibiotic prescribing that could in turn result in improved prescribing practices in dentistry. Yet, it is unclear to what extent health practitioners use these guidelines for the prescription of antibiotics for dental clinical conditions.
Given this unclear picture of oral antibiotic prescription patterns for dental conditions, this study aimed to determine antibiotic prescription trends and patterns for dental use in the public health care sector in Pietermaritzburg, in order to have a better understanding of the current management of dental conditions.
METHODOLOGY
This was an exploratory study, using a combination of qualitative and quantitative data. The research sites comprised two purposively selected hospitals (Institution A and Institution B) in the Pietermaritzburg Complex, given that these two institutions offer both basic oral health services such as management of dental caries and periodontal disease as well as more advanced services related to trauma and various types of pathology. Two phases were used in this study. The first phase comprised a retrospective clinical chart review for the period March 2012 to July 2018 (n=720). The second phase comprised two focus-group discussions (FDGs) with purposively selected health practitioners (one FGD at each institution). The study selection criteria included all health care professionals who prescribed and dispensed antibiotics for dental use. The study excluded dental and medical managers, and practitioners not involved in the clinical management and prescription of antibiotics for dental use. Ethical clearance was obtained from the Biomedical Research Ethics Committee, University of KwaZulu-Natal (Reference number. BE026/190) while permission to conduct the study was obtained from the KwaZulu-Natal Department of Health (Reference number. NHRD Ref: KZ_201902_018).
For the retrospective clinical record review, managers for each admissions department in the respective research site selected and retrieved the clinical records based on the criteria set by the researcher. The rationale for this approach was to minimize potential researcher bias in the selection of clinical records for review. The inclusion criteria included patients aged 6 to 80 years; evidence of documented antibiotic prescription for dental conditions; antibiotic prophylaxis for systemic conditions such as infective endocarditis in a patient who suffered from rheumatic heart fever; or oral antibiotic cover prior to dental surgery and/or after dental treatment. A data capturing sheet was used to document the patients' age, gender, dental history, main complaint, symptoms, differential diagnosis, laboratory reports, prescribed treatment, number of prescribed medications, drug dosage, frequency and route of administration. An antibiotic therapy worksheet12,13 was used to gather information related to the appropriateness of the antibiotic regimen, therapeutic duplication and adverse reactions, and comparisons were made with the Standard Treatment Guidelines and the Essential Medicines List (2020). This worksheet has been validated in previous studies.12,13
Phase 2 comprised FGDs with health care practitioners (dental and medical practitioners) and pharmacists, involved in prescribing and dispensing antibiotics for dental purposes. Purposive sampling was used to set up the two FGDs comprising six volunteers per group at each research site. The inclusion criteria entailed practitioner eligibility to prescribe or dispense antibiotics for dental use; and registration with the Health Professionals Council of South Africa or the Pharmacy Council of South Africa (in the case of pharmacists). A semi-structured focus group schedule was used to collect data.
The focus group schedule comprised open-ended questions that explored participants' perspectives on the National Strategic Framework, Essential Medicines Lists, Standard Treatment Guidelines, The South African Antibiotic Stewardship Programme, antibiotic prescription patterns for dental conditions, adverse events related to antibiotic prescription and trends and perceptions of antibiotic prescription practices from a multi-disciplinary approach. Other questions included perceived barriers, challenges and opportunities to access oral health care, patient compliance, and the value of a multi-disciplinary team approach in combating antibiotic resistance. Written informed consent was obtained from all participants and ethical considerations such as confidentiality and anonymity were upheld. All participants were informed that they had the right to withdraw from the study at any stage without any negative consequences.
The FGDs were audio recorded and the recordings were transcribed verbatim and then cleaned. The information was transcribed onto a Microsoft Word document. A research consultant assisted with the data analysis process. Data coding was done independently by the researcher and the research consultant to identify significant features of the data and to sort out the data, thereby allowing for the emergence of sub-themes and themes from the participants' responses, as part of the thematic analysis.14-16 The data was then compared in order to identify common themes. The qualitative data was analyzed using Nvivo version.11 The credibility of the study was achieved by establishing that the findings of the study were a true reflection of the participant's' original view.17 Transferability was achieved by comparing the study findings with previous and current literature.18 Conformability was achieved through the use of quotations of actual dialogues expressed by study participants.19
The quantitative data was analyzed using IMB SPSS (version 25R). Univariate descriptive statistics such as frequency and mean distribution were conducted for all variables. Bivariate statistics was also used to assess the outcome and thereafter, the outcome was analyzed by the explanatory variable.20
RESULTS
Phase 1
A total number of 220 clinical charts (30.6%) were reviewed at Institution A and 500 clinical charts (69.4%) at Institution B. The study sample across the two institutions comprised 490 females (65.3 %). Almost half of the study sample (n= 357; 49.7 %) were in the age group 40-60 years. Only 86 patients (12%) recorded were in the 6-year-old age group.
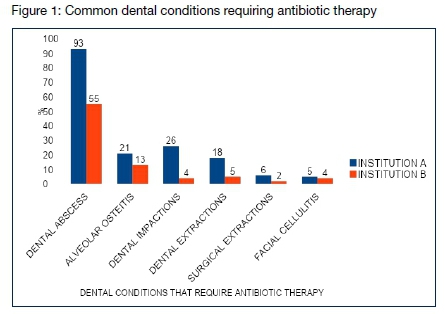
The most common dental infection requiring oral antibiotic therapy at both institutions was dental abscesses (n= 479; 66%), followed by acute alveolar osteitis (dry socket) (n=110; 15%); surgical removal of impacted third molars (n=78; 11%); dental extractions (n=62; 9%), and surgical extractions (n=22; 3%) (Figure 1). Allergies were recorded and alternate antibiotics were prescribed in a small number of clinical files (n=5; 3% in Institution A and n=7; 1% in Institution B). Healthcare practitioners in Institution A prescribed both Clindamycin and Azithromycin for patients allergic to Penicillin (n=5; 0.7%) while those in Institution B prescribed Erythromycin (n=2; 0.3%). According to the Standard Treatment Guidelines 2020 (STG), adult patients should receive Amoxicillin, oral, 500 mg 8 hourly for 5 days and Metronidazole, oral, 400 mg, 8 hourly for 5 days. In cases where patients have severe penicillin allergies, Azithromycin, oral, 500 mg daily can be prescribed for 3 days. The doses for the same antibiotics used in children presenting with dental abscesses, differed according to the guideline. The STG (2020) does not out outline antibiotic prescription for dental caries and dental extractions.
At Institution A, antibiotic therapy was prescribed for conditions such as trismus (n=13; 6%), soft palate swelling (n=9; 4%), fibrous epulis (n=6; 3%), and acute herpes simplex (n=2; 1%) (Table 1). With regards to herpes simplex lesions (such as those on the lips), the STG (2020) indicates that an antiviral agent such as Acyclovir, oral, 400 mg, 8 hourly, for 7 days should be prescribed for adult patients with extensive oral herpes for 7 days. This again reflects that the STG (2020) does not highlight the need for antibiotic prescription for patients with acute herpes simplex lesions. Antibiotic prescription is also not mentioned for conditions such as trismus and fibrous epulis in the STG (2020).
Antibiotics were prescribed for necrotizing gingivitis (n=20; 3%). The STG (2020) indicates that chlorhexidine 0.2%, 15 mL as a mouthwash, should be prescribed twice daily for patients with uncomplicated gingivitis while Metronidazole, oral, 400 mg, 8 hourly, for 5 days should be prescribed for patients with necrotizing periodontitis for 5 days together with chlorhexidine 0.2%, 15 mL as a mouthwash. The STG (2020) does not mention antibiotic prescriptions for dental conditions such as gingivitis, facial cellulitis, aphthous ulcers, and fibrous epulis. However, Cefalexin, oral 500mg 6 hourly for 5 days or Flucloxacillin, oral, 500mg 6 hourly for 5 days are indicated in the case of adults presenting with cellulitis.
Antibiotic therapy was prescribed for 16 patients treated for assault (7%) at Institution A while only 9 such cases were recorded at Institution B (2%). However, it is possible that more patients requiring management for assault could have presented at Institution A, hence this can explain the skew in the prescription trends between the two institutions. Moreover, there is no indication in the STG (2020) that antibiotics should be prescribed for patients presenting with trauma. Antibiotics were prescribed for patients for whom dental treatment was complicated due to systemic conditions or the treatment was deferred (n=18; 3%). and/or when the patient was referred to other health facilities for further clinical management (n=11; 2%). The systemic condition necessitated the postponement of dental treatment but antibiotics appeared to be prescribed because the patient needed dental extractions, in most cases. Less than half of the cases with uncontrolled blood pressure (n=48; 7%) were prescribed antibiotic therapy across both institutions. Patients undergoing treatment under general anaesthesia for dental extractions involving multiple teeth, were prescribed antibiotics at both Institution A (n=13; 2%) and Institution B (n=2; 0. 4%). Institution A was much more likely (n=20; 9%) than Institution B (n=4; 1%) to prescribe antibiotics for un-cooperative patients.
Although antibiotics were prescribed for mostly the same dental conditions at both institutions, certain prescriptions made at Institution B did not appear to be prescribed at Institution A. Antibiotic therapy was prescribed for eruption pain (n=4; 1%) and in cases where patients required a dental extraction but did not have their inhaler for their asthma treatment (pump) (n=3; 1%) at Institution B (Table 1).
However, there is no indication if antibiotics were prescribed because the treatment had to be postponed, in the case of a patient who did not bring his/her asthma treatment (pump) to the dental clinic, or due to the dental condition.
Phase 2
The following themes emerged from data analysis: inconsistency in antibiotic use for dental treatment needs; adherence to the standard treatment guidelines, and strategies to combat antibiotic resistance.
Theme 1: Inconsistency in antibiotic cover for dental-related treatment
Study participants indicated that medical practitioners are not primarily involved in the prescription of antibiotics for common dental conditions and instead refer patients to the dental department.
"Antibiotics were prescribed for dental abscesses, patients with multiple carious teeth presenting for general anesthesia, prophylaxis for rheumatic heart fever [Prophylaxis for infective endocarditis in a patient who suffered from rheumatic heart fever] and cases of open wound fractures and trauma" (Institution A). On the other hand, antibiotic coverage was prescribed for dental abscess, open wound fractures, cellulitis, dry socket, pericoronitis, and periodontitis, and antibiotic prophylaxis after tooth extraction, necrotizing ulcerative gingivitis, rheumatic heart fever and infective endocarditis at Institution B.
Theme 2: Antibiotic prescription and the adherence to the Standard Treatment Guidelines
All participants (medical and dental practitioners) confirmed that antibiotics were prescribed according to the STG, as reflected in the following quotation. "Yes, the standard treatment guidelines are followed when prescribing antibiotics." (Institution A) "The medical and dental practitioners seem to be prescribing the correct regimen according to the Standard treatment guidelines." (Pharmacists from Institution A). However, this finding is not congruent with the results of the clinical record analysis reported earlier.
Theme 3: Strategies to combat antibiotic resistance
There was no consensus among research participants on the need for diagnostic laboratory testing to improve antibiotics prescription. However, all participants agreed that there is a need to improve antibiotic prescription in their respective hospitals despite the fact that the respondents indicated earlier that the standard treatment guidelines are followed."Prescribers use empirical treatment which may result in antibiotic resistance." (Institution B).
Some recommendations to improve antibiotics prescription trends and reduce possible resistance are listed in Table 2.
DISCUSSION
The need for systemic antibiotic use in dentistry is limited given that most dental infections such as pulpitis and periapical periodontitis, require only operative procedures such as extractions, restorations or root canal therapy and that it is only by exception that antibiotics are required for dental conditions.6 Yet, the results of this study indicate that some inconsistencies in antibiotic prescriptions for dental conditions did exist in the two identified sites. According to our study, a dental abscess (66%) was the most common dental infection requiring antibiotic therapy. Long postulates that dental abscesses larger than 5 cm, cellulitis or conditions with mixed abscess-cellulitis require antibiotics coverage.21 Incision and drainage (especially when there is substantial inflammation and pain) with or without adjunctive antibiotic therapy are recommended for localized infections such as a periapical abscess, periodontal abscess and a localized dentoalveolar abscess. Likewise, sepsis can progress to cellulitis, and possibly to Ludwig's angina which could be life-threatening. Therefore, the prescription of antibiotics is justified in the management of dental abscesses.22-24
The clinical records revealed that antibiotics were prescribed for the treatment of alveolitis (dry socket) (15%), as it is done in England, Kuwait and Turkey where almost half the dentists surveyed would prescribe antibiotics for a dry socket.23 However, a single dose of Metronidazole was not found to be effective in preventing the onset of dry socket. Similarly, most dentoalveolar surgical procedures in healthy individuals did not require antibiotic prophylaxis.23
This study further indicated that antibiotic prophylaxis was prescribed for impacted third molar surgery (11%). Prophylactic antibiotic therapy in third molar surgery in healthy patients is highly controversial.25 There is no clear evidence that pre-operative antibiotic prophylaxis for routine third molar surgery is necessary for patients with no underlying medical complications.23 A Cochrane review indicated that prophylactic antibiotics reduces the risk of infection, dry socket and pain following third molar extraction.6 Yet, at the same time, the STG (2020) has limited information on the management of dental conditions, with no mention of antibiotic prophylaxis to be given prior to the surgical removal of impacted third molars.
Likewise, the STG (2020) does not provide guidance for all dental conditions that are managed within clinical settings in South Africa. The implications are that this guideline does not provide adequate guidance for dental clinical management. This inadvertently creates loopholes for health and dental practitioners to use their own discretion in deciding when to prescribe antibiotics. This finding is consistent with Lalloo et al. who also observed that practitioners might be using subjective measures or even personal preferences when deciding whether to prescribe antibiotics or not.3 This highlights the need for an urgent review of the STG (2020) so that this document is able to provide more comprehensive guidance to practitioners in the country.
Antibiotics were prescribed for dental conditions such pericoronitis (2%), trismus (2%), acute herpes simplex (0.3%); aphthous ulcers (1%), fibrous epulis (1%), and eruption pain or for procedures such as (0.5%) restorations (fllings) (1%), biopsy (0.4 %) when the STG (2020) has not indicated antibiotics for these conditions and procedures. Antibiotics were also prescribed for uncooperative patients requiring dental extractions especially in Institution A (9%), or because the patient requested so (0.2%). Although these percentages are low, the implications are the wholly inappropriate use of antibiotics for dental clinical management, in respect of certain dental conditions.
The results of the qualitative data analysis further indicated that medical practitioners were more likely to refer patients to the dental department for the prescription of antibiotics for common dental conditions. At the same time all participants suggested that the prescription of antibiotics for dental use was based on the STG, yet the results of the retrospective clinical records review illustrate that antibiotics were prescribed for conditions that are not covered in the guideline. This finding is thus not consistent with the results of the clinical record analysis thereby suggesting some inconsistencies in the pattern and trends in antibiotic prescriptions for dental conditions at the two health institutions.
Antibiotics were prescribed for patients for whom treatment was complicated due to underlying systemic conditions. It is noteworthy that antibiotics were not prescribed for the systemic condition, but rather, were given because either the dental treatment could not be performed or it was deemed that the patient is at risk of infection due to the systemic condition. This finding is consistent with previous reviews which concluded that patients with low immunity may be at higher risk of infection.26 In such cases prophylactic antibiotics could be beneficial to patients, where applicable.26
The results of this study showed that antibiotics were prescribed for the prevention of infective endocarditis in a patient who suffered from rheumatic heart fever (1%). This observation is consistent with the findings reported by Mthethwa et al., in that 2.2% of antibiotic prescriptions were given for this purpose. Bacterial endocarditis remains a risk following dental treatment.27 This is supported by the British Society for Antimicrobial Chemotherapy and the American Heart Association which recommend that only high-risk patients require such cover.28,29 Although antibiotic prophylaxis to prevent infective endocarditis in patients who suffer from rheumatic heart fever, is widely accepted by the dental profession,6 the effectiveness of such antibiotic prophylaxis in humans, however, remains unproven.30,31 The question however, remains as to whether antibiotics were prescribed judiciously in this study. Future research in this area is needed to further explore these identified issues.
Overall, the results of the study suggest that some over-prescription of antibiotics does exist. This needs to be reviewed because an increase in bacterial resistance to antibiotics and the associated costs will have an impact on care care delivery as well as resource allocations.3 Dental practitioners have a responsibility to reduce and improve the way they prescribe antibiotics and should prescribe with the correct indications. Practitioners should not be swayed or influenced by the patient's demands for antibiotics cover.32 Dental practitioners also have a responsibility to educate patients on the spread and consequences of antimicrobial resistance.32 There should be greater community awareness on the appropriate use of antibiotics.32 and the injudicious prescription of antibiotics for the treatment of 'toothache' should be avoided.33 Clinicians thus need to be aware of the ongoing evidence base for antibiotic prescription practices.3 More research is required for the appropriate antibiotic prescription in the field of clinical dentistry.34 Some participants in the FGDs also indicated that pharmacists played an important in the oversight and approval of antibiotic prescriptions recommended by medical and dental practitioners. This reiterates the value of a multidisciplinary team approach for antibiotic stewardship so as to ensure that there is oversight and accountability for antibiotic prescriptions.
Study strengths and Limitations
This study provided much needed data on antibiotic prescription patterns for dental conditions in the public health sector in Pietermaritzburg. While the value of such timely data cannot be overstated, several limitations were noted. The study findings are limited to the two participating health institutions and the reporting period (March 2012- July 2018). Poor record keeping and insufficient diagnostic data could have skewed the study findings. From a data analytical process, inferential statistics were a challenge given the nature of the data collected in the retrospective clinical chart review. A further research question could focus on practitioners' source of knowledge for antibiotic prescriptions (e.g. is it university education, continuing professional development, national guidelines, etc.). This could perhaps identify the gaps that seem to contribute to practitioners' decision-making. Despite these limitations, a clear picture has emerged on antibiotic prescription patterns at the identified health institutions.
CONCLUSION
This study showed that there were some differences in antibiotic prescription trends for dental conditions at the two public health institutions. There is a need for consensus building among health professionals and for better guidance in respect of antibiotic prescription in the management of dental conditions.
Acknowledgements
All study participants for their active participation in the study. The administrative departments at the two research sites for their support.
Conflict of interest
None
References
1. Farley, E., Stewart, A., Davies, M.A., Govind, M., Van den Bergh, D. and Boyles, T.H. (2018). Antibiotic use and resistance: Knowledge, attitudes and perceptions among primary care prescribers in South Africa. SAMJ: South African Medical Journal, 108(9), pp.763-771. [ Links ]
2. O'Neill, J. (2019). Tackling drug-resistant infections globally: final report and recommendations: the review on antimicrobial resistance; 2016 [Available from: https://amr-review.org.Publications.html. [ Links ]
3. Lalloo, R., Solanki, G., Ramphoma, K. and Myburgh, N.G. (2016). AntibioticBprescribing patterns of South African dental practitioners following tooth extractions. Journal of Investigative and Clinical Dentistry, 8(4), p.e12247 [ Links ]
4. Schellack, N., Benjamin, D., Brink, A., Duse, A., Faure, K., Goff, D., Mendelson, M., Meyer, J., Miot, J., Perovic, O. and Pople, T. (2017). A situational analysis of current antimicrobial governance, regulation, and utilization in South Africa. International journal of infectious diseases, 64, pp.100-106. [ Links ]
5. Mainjot, A., D'hoore, W., Vanheusden, A. and Van Nieuwenhuysen, J.P.(2009). Antibiotic prescribing in dental practice in Belgium. International endodontic journal, 42(12), pp.1112-1117. [ Links ]
6. Mthethwa, S.R. and Matjila, S.A. (2018). Antibiotic prescribing practices of dentists at Medunsa Oral Health Centre. South African Dental Journal, 73(8), pp.520-526. [ Links ]
7. Matthews, D.C., Sutherland, S. and Basrani, B. (2003). Emergency management of acute apical abscesses in the permanent dentition: a systematic review of the literature. Journal of the Canadian Dental Association, 69(10), pp.660. In Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. Centre for Reviews and Dissemination (UK). [ Links ]
8. Lalloo, R., Solanki, G., Ramphoma, K. and Myburgh, N.G. (2016). Antibiotic prescribing patterns of South African dental practitioners following tooth extractions. Journal of Investigative and Clinical Dentistry, 8(4), p.e12247 [ Links ]
9. National Department of Health of South Africa (2017). Guidelines on the Implementation of the Antimicrobial Strategy in South Africa: One Health Approach and Governance. Ministerial Advisory Committee on Antimicrobial Resistance, National Department of Health Affordable Medicines Directorate, Department of health, RSA, June 2017. [ Links ]
10. Standard Treatment Guidelines and the Essential Medicines List (2020). Available at: http://www.kznhealth.gov.za/pharmacy/PHC-STG-2020.pdf [ Links ]
11. Perumal-Pillay, V.A. and Suleman, F. (2017). Selection of essential medicines for South Africa-an analysis of in-depth interviews with national essential medicines list committee members. BMC health services research, 17(1), p.17. [ Links ]
12. Huang, W.H. and Owen, C.P. (2012). Antibiotic prophylaxis for dental procedures: is it necessary? Clinical review. South African Dental Journal, 67(7), pp.413-419. [ Links ]
13. Ntsekhe, M., Hoohlo-Khotle, N., Tlali, M. and Tjipura, D. (2011). Antibiotic prescribing patterns at six hospitals in Lesotho. Submitted to the US Agency for International Development by the Strengthening Pharmaceutical Systems (SPS) Program. http://apps.who.int/medicinedocs/documents/s21028en/s21028en.pdf) Accessed on 16 June2020. [ Links ]
14. Thomas, J. and Harden, A. (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC medical research methodology, 8(1), pp.45. [ Links ]
15. Bazeley, P. (2009). Analysing qualitative data: More than 'identifying themes'. Malaysian Journal of Qualitative Research, 2(2), pp.6-22. [ Links ]
16. Dookie, S., Singh, S. and Myburgh, N.G. (2017). Analysis of district oral health services in KwaZulu-Natal. African Population Studies, 31(2), pp.3683-3693 [ Links ]
17. Braun, V. and Clarke, V. (2006). Using thematic analysis in psychology. Qualitative research in psychology, 3(2), pp.77-101. [ Links ]
18. Creswell, J.W. and Creswell, J.D. (2017). Research design: Qualitative, quantitative, and mixed methods approaches. 4th edition, Sage publications. [ Links ]
19. Mandal, P. (2018). Qualitative research: Criteria of evaluation. International journal of academic research and development, 3(2), pp.591-596. [ Links ]
20. Bertani, A., Di Paola, G., Russo, E. and Tuzzolino, F. (2018). How to describe bivariate data. Journal of thoracic disease, 10(2), p.1133-1137. [ Links ]
21. Long, S.S. (2016). Optimizing antimicrobial therapy in children. Journal of Infection, 72, pp.S91-S97. [ Links ]
22. Olsen, I. and van Winkelhoff, A.J. (2014). Acute focal infections of dental origin. Periodontology 2000, 65(1), pp.178-189. [ Links ]
23. Dar-Odeh, N.S., Abu-Hammad, O.A., Al-Omiri, M.K., Khraisat, A.S. and Shehabi, A.A. (2010). Antibiotic prescribing practices by dentists: a review. Therapeutics and clinical risk management, 6, p.301-306. [ Links ]
24. Kuriyama, T., Absi, E.G., Williams, D.W. and Lewis, M.A.O. (2005). An outcome audit of the treatment of acute dentoalveolar infection: impact of penicillin resistance. British dental journal, 198(12), pp.759-763. [ Links ]
25. Lodi, G., Figini, L., Sardella, A., Carrassi, A., Del Fabbro, M. and Furness, S. (2012). Antibiotics to prevent complications following tooth extractions (Review). Cochrane Database Syst Rev. [ Links ]
26. Sidana, S., Mistry, Y., Gandevivala, A. and Motwani, N. (2017). Evaluation of the need for antibiotic prophylaxis during routine intra-alveolar dental extractions in healthy patients: a randomized double-blind controlled trial. Journal of Evidence Based Dental Practice, 17(3), pp.184-189. [ Links ]
27. Pallasch, T.J. (2003). Antibiotic resistance. Dental Clinics, 47(4), pp.623-639. [ Links ]
28. Gould, F.K., Elliott, T.S.J., Foweraker, J., Fulford, M., Perry, J.D., Roberts, G.J., Sandoe, J.A.T. and Watkin, R.W. (2006). Guidelines for the prevention of endocarditis: report of the Working Party of the British Society for Antimicrobial Chemotherapy. Journal of antimicrobial chemotherapy, 57(6), pp.1035-1042. [ Links ]
29. Wilson, W., Taubert, K.A., Gewitz, M., et. al. (2007). Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation, 116(15), pp. 1736-1754. [ Links ]
30. Jankelow, D., Cupido, B., Zuhlke, L., Sliwa, K., Ntsekhe, M., Manga, P., Doubell, A., Lawrenson, J. and Essop, M.R. (2017). Prevention of infective endocarditis associated with dental interventions: South African Heart Association position statement, endorsed by the South African Dental Association. SA Heart Journal, 14(3), pp.170-174. [ Links ]
31. Chambers, J.B., Shanson, D., Hall, R., Pepper, J., Venn, G. and McGurk, M. (2011). Antibiotic prophylaxis of endocarditis: the rest of the world and NICE. Journal of the Royal Society of Medicine, 104(4) pp.138-40. [ Links ]
32. Sanderson S. (2019). A Piece on the need for global guidance on antibiotic stewardship in dentistry.AMR Control, FDI 120, 27 July. [ Links ]
33. Lewis, M.A.O. (2008). Why we must reduce dental prescription of antibiotics: European Union Antibiotic Awareness Day. British dental journal, 205(10), pp.537538. [ Links ]
34. Perić, M., Perković, I., Romić, M., Simeon, P., Matijević, J., Prpić Mehičić, G. and Jukić Krmek, S. (2015). The pattern of antibiotic prescribing by dental practitioners in Zagreb, Croatia. Central European journal of public health, 23(2), pp.107-113. [ Links ]
 Correspondence:
Correspondence:
Shenuka Singh:
Discipline of Dentistry, School of Health Sciences
University of KwaZulu-Natal
Tel: 031-2068591, Fax: 031-260806
E-mail:singhshen@ukzn.ac.za
Author contributions:
1 . P Ramnarain: Study conceptualization, data collection and analysis, report writing
2 . S Singh: Research supervision, study conceptualization, review of study results, manuscript review and revision.
Both authors approved the final submission.














