Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.77 no.2 Johannesburg Mar. 2022
http://dx.doi.org/10.17159/2519-0105/2022/v77no2a3
RESEARCH
The Knowledge and Participation of Community Health Care Workers in Oral Health Promotion
LM MakgetlaI; MP MoleteII
IBachelor of Dental Therapy; Diploma in Public Management; Diploma in Public Health; Masters in Public Health (UNISA). Gauteng Provincial Health; Oral Health Directorate
IIBDS; MSc; MDent; PhD (Public Health) (Wits). Wits Faculty of Health Sciences; School of Oral Health Sciences; Department of Community Dentistry. ORCID 0000-0001-9227-3927
ABSTRACT
INTRODUCTION: The human resource constraints in oral health has affected the delivery and sustainability of community oral health programs hence, in the West Rand District of Gauteng, Community Health Workers (CHW) are trained and integrated in Oral Health
AIM: The study therefore sought to assess the level of oral health knowledge and referral practices of CHW working in the West Rand.
METHODOLOGY: The study utilized a cross-sectional descriptive study design and was undertaken in three West Rand district regions. A self-administered questionnaire was used to collect the data and data was analyzed using descriptive and the chi-squared bivariate statistics.
RESULTS: Out of the 450 CHW working in the West Rand, n=148 of them participated in the study, their average age was 39; (SD:8.8) and had 9 years (SD:3.3) of work experience. As much as over 60% of participants reported to have been familiar with common oral conditions, they largely recognized tooth decay (48%) and information concerning the prevention of common diseases such as tooth decay and gum disease was inadequate. In terms of referral practices, they were poor as only (37%) referred when they recognized something unusual and (11%) never referred at all.
CONCLUSION: The oral health knowledge of the West Rand (CHW) was found to be inadequate, and this affected their ability to competently assess and refer common oral conditions.
Key words: Community Health Workers; Programs; Oral Health Promotion; Oral Disease Prevention
INTRODUCTION
Oral health contributes significantly to a health-related quality of life (HRQoL).1 The most common oral disease is tooth loss, which may lead to low self-esteem, psychosocial effects and malnutrition as a result of difficulty in chewing.2 In addition, the effects of the pain caused by oral disease on individuals and families result in loss of workdays for parents and school absenteeism for children. This subsequently leads to a negative impact on socioeconomic development.2 Furthermore, the burden of oral diseases globally has a disproportionately high bearing on the disadvantaged as well as socially marginalized communities because treatment costs are prohibitive while oral health systems are inadequately resourced to provide service.3,4
The human resource constraints in oral health and current staff shortages affect the delivery and sustainability of community oral health programs.5,6,7 In other general health programs, the increased demand of health services has been addressed by task shifting from professional health workers to lay health care workers such as Community Health Workers (CHW).8 CHW were officiallyintegrated into the South African public health system in 2011 as part of efforts to re-engineer and reform primary health care in the country.9 Thus, they have been shown to be effective in engaging closely with communities.10 This approach is in line with the restructuring of health systems that is being advocated by the World Health Organization; with the idea of creating an environment where non-oral health personnel can educate, refer, and attend to basic dental needs in order to increase accessibility.11
Therefore, integration of Community Health Workers in community oral health promotion needs to be considered as CHW are generally trained to render health promotion services in the community, they are involved in health education, community engagement and linking communities to health services.8,12 Their services have also shown to have brought about an improvement in health outcomes of HIV positive mothers and their infants. In addition, they improve community access to primary health care facilities for chronic diseases.8,9
In the West Rand District of Gauteng, CHW are trained in oral health as they are inducted in the district. However, there exists no documentation outlining the nature and dimensions of CHWs knowledge and participation in oral health promotion. It is therefore important to make this assessment in order to document their level of oral health knowledge and to identify what their role in oral health has been to date. The information will assist in addressing any knowledge gaps and also providing direction that is needed for improving the integration of community health workers in the district and ultimately oral health experiences of communities.
The aim of the study therefore sought to assess the type of oral health knowledge and referral practices of CHW working in the West Rand district of Gauteng.
METHODOLOGY
The study utilized a cross-sectional descriptive study design and was undertaken in three West Rand district regions that included; Mogale City, Rand West and Merafong City. The District has an estimated population of 838 594 residents.13
The population of interest was on 450 CHW who are deployed in various communities. Out of the 450 CHW, Participants were conveniently sampled according to an inclusion and exclusion criteria. The inclusion criteria comprised of CHWs who were from the chosen three health sub-districts and had some prior training in oral health promotion. An exclusion criterion entailed CHWs who were not trained in OHP and were not formally employed by the government.
A self-administered questionnaire was used to collect the data. The questionnaire was adapted from a pre-existing questionnaire by Praveen et al (2014).14 The questionnaire was assessed by the postgraduate committee at University of South Africa (UNISA) for face validity. Upon approval of the questionnaire by the university, the questionnaire was piloted on Ave trained CHWs, after the pilot, all the inconsistencies were addressed and the questionnaire was refined before its use on the study participants.
Ethical clearance was provided by the (UNISA) department of health studies REC 012714-039 (NHERC). Additionally, permission was sought from the district directors and clinic managers. Prior to administering the questionnaire, the researcher outlined the study to the participants, received their consent to participate in the study and assured them that their participation would be anonymous. In addition informed them that they were under no obligation to participate.
Data analysis
Data was captured on Microsoft excel spreadsheet, and imported to the STATA Statistical Software, version 14 for analysis. Descriptive summary statistics was utilized to determine socio-demographic characteristics and type of knowledge using means, standard deviation, frequencies and proportions. Relationships between dependent variables such as knowledge and referral patterns with education, training, and years of experience were assessed using the Pearson and Fischer's exact chi-squared tests.
RESULTS
Sociodemographic information
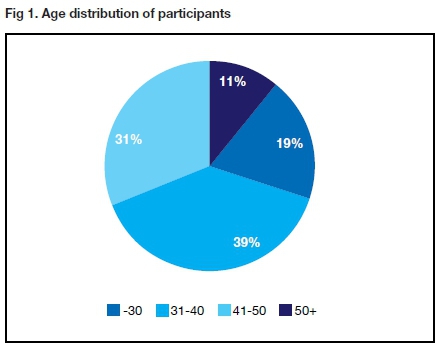
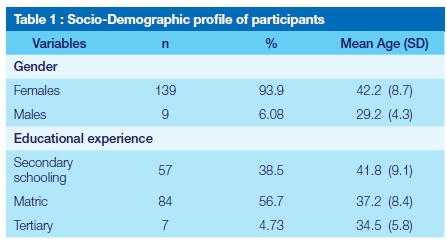
Out of the 450 CHW, (n=148) completed the questionnaire and participated in the study. Majority of the participants were between the ages of 31-40. The mean age was 38.8 (SD:8.89). The mean years of work experience was 9.1 (SD:3.3), (Figure 1). They were largely females (94%) and just over half of them had matriculated (57%). The male participants were of a younger age, and the older participants had limited education. (See table 1).
Knowledge; Common Oral Conditions
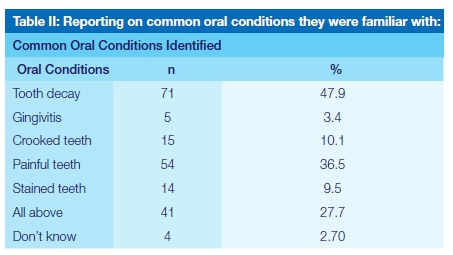
Of the 148, (N=93/ 62.8%) claimed they were familiar with recognizing common oral diseases. However when asked which specific common conditions they were familiar with (see table 2), 48% identified tooth decay, this was followed up by painful teeth, 36.5% and only 28% recognized all the listed common conditions.
Knowledge; Prevention
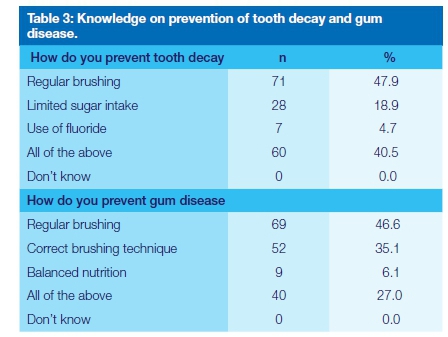
In terms of prevention of tooth decay, majority of them 48% said tooth decay was prevented only by brushing, only 40,5 % correctly answered that tooth decay was prevented collectively by brushing, limited sugar intake and fluoride (see table 3). The knowledge concerning prevention of gingivitis (gum disease), only 27% answered correctly by choosing all of the above, which included regular correct brushing and balanced nutrition. A large majority 47% answered that gum disease was only prevented by regular brushing (see table 3).
Referral practices
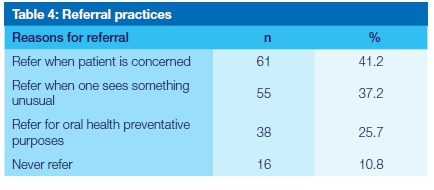
Majority of the participants (41.2%) referred patients to oral health facilities when the patients were concerned about their oral cavity. Less than half referred when they recognized something unusual in the mouth and 11% never referred patients to oral health facilities.
The Fischer's exact chi squared showed no significant associations between the identification of common oral conditions and education (p=0.81), years of experience (p=0.58) and training (p=0.72). In addition, no relationship was found between appropriate referral practices to education (p=0.73), years of experience (p=0.10) and training (p=0.62).
DISCUSSION
The average age of participants was 39 years old and they had approximately 9 years of experience. As much as over 60% of participants reported to have been familiar with common oral conditions, their knowledge was elementary. They largely recognized tooth decay (48%) and information they had on prevention of common diseases such as tooth decay and gum disease was inadequate. In terms of referral practices, they were poor as only (37%) referred when they recognized something unusual and 11% never referred at all. No significant associations were found between knowledge and education, training and years of experience. In addition, no link was found between referral patterns and education, training and years of experience.
The majority of CHWs involved in oral health services in the West Rand Health District were 31 to 40 years, had a high school background and had many years of experience (9years). However, this did not translate in our results to having adequate oral health knowledge. This is similar to results reported from a study in Iran where it was observed that the longer the time passed after training of CHW, the lesser the ability of the workers to remember information on oral health.15,16 In addition, CHWs might have received a once-off training upon commencement of their contract and no follow-up or re-training was done.15 Participants' knowledge was especially limited. Despite them being trained and 62.8% claiming familiarity with common oral lesions, only 28% recognized all the common oral conditions. In addition, less than 30% answered correctly on information regarding the prevention of dental caries and gingivitis. The level of understanding of oral health conditions was clearly reflected to be poor and it is suggested that this is in most part attributed to the training intervention.17,18 Culturally and linguistically relevant educational approaches have shown greater success than traditional didactic approaches that are commonly offered to CHW.19
It is a concern that only 37% of the respondents refer when they recognize something unusual and that they largely (47%) refer when someone is concerned about the condition of their oral cavity. This implies that they are not able to recognize unusual oral conditions and thus would be inadequately competent in undertaking appropriate referrals. It could be that their training does not emphasize how to differentiate between normal and abnormal oral conditions.20 In addition, there was uncertainty and lack of preparedness on the functions they were expected to perform.21 Intensive training that involves practical sessions and continuous follow up has been shown to be successful in Kenya for increasing CHW's knowledge, identification and referrals of oral HIV lesions of community members.22
Literature has shown that CHWs potentially have a vital role to play in the promotion of good oral health and prevention of oral health diseases as they form a key link between communities and the health system.21 However, the study reflected our participants to be ill prepared to contribute to oral health and that their role and participation is generally poorly defined.23 It is therefore recommended that CHWs should be exposed to regular training as a way of Continuous Professional Development (CPD). In addition, periodic monitoring and evaluation of the training and participation should be undertaken in order to address emerging gaps proactively.
Limitations of the study.
Little has been documented on the structure or various forms of training that the CHWs were exposed to, thus the study could not measure their training from a standard baseline. Hence the questionnaire was developed around basic oral health knowledge that was expected from non-oral health care workers; and the study was able to outline existing knowledge gaps that impacted on the oral health involvement of CHWs in the West Rand.
CONCLUSION
Considering that CHW participating in the study were trained in oral health and over 60% of them claimed to be familiar with common oral lesions, their oral health knowledge was not found to be adequate. This affected their ability to be able to competently assess and refer common oral conditions. The current training approach that they are exposed to needs to be reviewed and redesigned in order to equip them with the necessary skills required to effectively participate in oral health promotion and disease prevention.
Acknowledgement
We would like to thank Prof. ON Makhubele of the University of South Africa (UNISA) for her guidance in the research process.
References
1. Zucoloto ML, Maroco J, Campos JA. Impact of oral health on health-related quality of life: a cross-sectional study. BMC Oral Health. 2016 Dec;16(1):1-6. [ Links ]
2. Sheiham A, Alexander D, Cohen L, Marinho V, Moysés S, Petersen PE, Spencer J, Watt RG, Weyant R. Global oral health inequalities: task group-implementation and delivery of oral health strategies. Advances in Dental Research. 2011 May;23(2):259-67. [ Links ]
3. Van Wyk PJ, van Wyk C. Oral health in South Africa. International Dental Journal. 2004 Dec 1;54:373-7. [ Links ]
4. Peres MA, Macpherson LM, Weyant RJ, Daly B, Venturelli R, Mathur MR, Listl S, Celeste RK, Guarnizo-Herreho CC, Kearns C, Benzian H. Oral diseases: a global public health challenge. The Lancet. 2019 Jul 20;394(10194):249-60. [ Links ]
5. Govender U, Bhayat A, Rudolph M. Services rendered and barriers faced by public sector oral hygienists in two provinces of South Africa. South African Dental Journal. 2013 May 1;68(4):156-60. [ Links ]
6. Reddy M, Singh S. Viability in delivering oral health promotion activities within the Health Promoting Schools Initiative in KwaZulu-Natal. South African Journal of Child Health. 2015 Nov 3;9(3):93-7. [ Links ]
7. Molete M, Stewart A, Bosire E, Igumbor J. The policy implementation gap of school oral health programmes in Tshwane, South Africa: a qualitative case study. BMC health services research. 2020 Dec;20(1):1-1. [ Links ]
8. Schmitz K, Basera TJ, Egbujie B, Mistri P, Naidoo N, Mapanga W, Goudge J, Mbule M, Burtt F, Scheepers E, Igumbor J. Impact of lay health worker programmes on the health outcomes of mother-child pairs of HIV exposed children in Africa: A scoping review. PloS one. 2019 Jan 31;14(1):e0211439. [ Links ]
9. Nxumalo N, Goudge J, Thomas L. Outreach services to improve access to health care in South Africa: lessons from three community health worker programmes. Global health action. 2013 Dec 1;6(1):19283. [ Links ]
10. Horwood C, Butler L, Barker P, Phakathi S, Haskins L, Grant M, Mntambo N, Rollins N. A continuous quality improvement intervention to improve the effectiveness of community health workers providing care to mothers and children: a cluster randomised controlled trial in South Africa. Human resources for health. 2017 Dec;15(1):1-1. [ Links ]
11. Pitts NB, Mayne C. Making Cavities History: A Global Policy Consensus for Achieving a Dental Cavity-Free Future. JDR Clinical & Translational Research. 2021 May 24:23800844211020298. [ Links ]
12. Thema KL, Singh S. Oral health service delivery in Limpopo Province. South African Dental Journal. 2017 Aug;72(7):310-4. [ Links ]
13. Municipalities of South Africa; West Rand District Municipality. In https://municipalities.co.za/overview/115/west-rand-district-municipality; Accessed on (20/11/2020). [ Links ]
14. Praveen G, Anjum MS, Reddy PP, Monica M, Rao KY, Begum MZ. Effectiveness of school dental screening on stimulating dental attendance rates in Vikarabad town: A randomized controlled trial. Journal of Indian Association of Public Health Dentistry. 2014 Apr 1;12(2):70. [ Links ]
15. Eskandari A, Abolfazli N, Lafzi A, Golmohammadi S. Oral health knowledge and attitudes of community health workers in East Azerbaijan, Iran. Journal of Dentistry. 2016 Dec;17(4):297. [ Links ]
16. Kwan SY, Petersen PE, Pine CM, Borutta A. Health-promoting schools: an opportunity for oral health promotion. Bulletin of the World Health organization. 2005;83:677-85. [ Links ]
17. Villalta J, Askaryar H, Verzemnieks I, Kinsler J, Kropenske V, Ramos-Gomez F. Developing an effective community oral health workers-"Promotoras" model for early head start. Frontiers in public health. 2019 Jul 3;7:175. [ Links ]
18. Hoeft KS, Rios SM, Guzman EP, Barker JC. Using community participation to assess acceptability of "Contra Caries", a theory-based, promotora-led oral health education program for rural Latino parents: a mixed methods study. BMC oral health. 2015 Dec;15(1):1-1. [ Links ]
19. Horton LA, Parada H, Slymen DJ, Arredondo E, Ibarra L, Ayala GX. Targeting children's dietary behaviors in a family intervention:'Entre familia: reflejos de salud'. salud pública de méxico. 2013;55:397-405. [ Links ]
20. Ramos-Gomez FJ. A model for community-based pediatric oral heath: implementation of an infant oral care program. International journal of dentistry. 2014 Oct;2014. [ Links ]
21. Venancio ED, Paula EM, Reis CB. Oral health care: the knowledge and work of the community health agent. Revista de Odontologia da UNESP. 2014 Mar;43:124-30. [ Links ]
22. Koyio LN, Sanden WJ, Dimba E, Mulder J, Creugers NH, Merkx MA, van der Ven A, Frencken JE. Oral health training programs for community and professional health care workers in Nairobi East District increases identification of HIV-infected patients. PloS one. 2014 Mar 14;9(3):e90927. [ Links ]
23. Khan MA, Okeah BO, Mbivnjo EL, Kisangala E, Pritchard AW. The Role of Community Health Workers in Oral Health Promotion and the Impact of their services in Sub-Saharan Africa: A Systematic Review. medRxiv. 2021 Jan 1. [ Links ]
 Correspondence:
Correspondence:
Mpho Molete
Email: mpho.molete@wits.ac.za
Tel: 011 7172241
Author contributions:
1 . Lesego M Makgetla: 60%
2 . Mpho P Molete: 40%














