Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.76 no.8 Johannesburg Set. 2021
http://dx.doi.org/10.17159/2519-0105/2021/v76no8a4
RESEARCH
Predictable sedation: Safe administration of oral Midazolam and nitrous oxide gas for paediatric patients in the general dental practice
N PotgieterI; G StreitII
IBChD, PDD, PGDIP (Dent), MSc(Dent), Department of Paediatric Dentistry, Faculty of Dentistry, University of the Western Cape. ORCID: 0000-0003-4061-3322
IIBChD, MSc(Dent), PGDipAesth, PGDipPracManagement, PDD Interceptive Ortho, PGDipPaedo. Department of Odontology, School of Dentistry, Faculty of Health Sciences, University of Pretoria. ORCID: 0000-0003-2251-7169
ABSTRACT
INTRODUCTION: Behaviour management for anxious paediatric dental patients is challenging. Solutions include education and sedation. Various drugs have been used to effectively sedate paediatric patients during treatment.
Aims and objectives: The aim of this study was to review literature on the sedation of paediatric patients. The study specifically looked at those reviews covering the combination of two sedation methods in case of more challenging paediatric patients.
DESIGN: The study undertook a literature review focused on studies using nitrous oxide, Midazolam, or a combination of the two substances.
METHODS: An electronic search was done on EBSCOhost to source articles published from 1979 to 2019.
RESULTS: A deeper form of sedation can be achieved for paediatric patients when using a combination of nitrous oxide, oxygen and a hypnotic agent such as Midazolam.
CONCLUSION: Dealing with the anxiety levels of paediatric patients is a challenge for dental health providers. Two of the main strategies used to deal with anxious children are behaviour management and sedation. A critical review of journal articles on the use of nitrous oxide and oxygen in combination with Midazolam was therefore undertaken. The findings suggest that, in order to achieve a deeper form of sedation, the combination of nitrous oxide, oxygen and Midazolam works well to reduce discomfort, anxiety and/or pain in paediatric patients
Keywords: Benzodiazepine, dental, Midazolam, nitrous oxide, paediatric, paedodontics, sedation.
AIM
The aim of this study was to review the literature on the sedation of paediatric patients, i.e. patients up to the age of 21 years. The literature review specifically focused on studies using nitrous oxide, Midazolam, or a combination of the two substances. An electronic search was done on EBSCOhost to source articles published over the last 40 years, i.e. articles from 1979 to 2019.
INTRODUCTION
Paediatric dentistry
Children frequently find dentistry challenging, as it induces anxiety. There are various reasons for this:1 Often, children's coping skills are not sufficiently developed to deal with such situations. As a result, they behave fearfully.2 Their anxiety and resultant behaviour can be linked to negative outcomes such as amplified oral ailments, evading dental treatment, and defiance.3 Behaviour management for young paediatric dental patients may therefore be challenging for both the child and the dentist.4
Note that in this paper, the term paediatrics is used to describe children and young people under the age of 21 years.5 According to The South African Children's Act No. 38 of 2005, a paediatric patient limit is 12 years of age.42
Behavioural management
Possibly the most challenging age group for the paediatric dentist to work with is children between 15 months and six years of age.6 Dealing with the anxiety levels of paediatric patients is one of the most demanding circumstances in the dental practice, making the undertaking of helping uncooperative children in need of dental care extremely challenging, if not impossible at times. Two of the main strategies used to deal with anxious children are behaviour management and sedation. Usually, when behaviour techniques are no longer sufficient to manage the child, the help of pharmacological substances is sought.
The dental team can educate children, as well as manage and alleviate their anxiety with suitable mechanisms aimed at eliciting appropriate and cooperative behaviour while in the dental chair. Excellent behaviour management facilitates safe, efficient and better quality treatment by the oral health team.
Children understand and react to painful stimuli in their own individual ways.7 Additionally, children under the age of four years are susceptible to the experience of painful stimuli, and are usually not able to verbalise their fears. Their reactions can be influenced by listening to older children's inaccurate descriptions of negative experiences, as they too do not always understand their experiences or do not communicate these appropriately. A child's behaviour can also be negatively affected by an anxious or nervous parent.8 Communication is the most important obstacle to overcome. Educating and, in essence, managing the parent before the child's first dental visit is of utmost importance. Establishing communication is the main goal for behaviour guidance; this alleviates fear and lessens anxiety. Building an undoubt-ing connection will therefore promote a positive attitude between parent, child and the dental health provider.8 This connection will set the ground work for a trusted relationship, allowing the child to be treated and handled.
Methods used by dental professionals to manage dental nervousness are principally designed to avoid unlikable and unproductive meetings with the paediatric patient. The aim is to create an atmosphere in which one can develop the child's self-confidence, thus allowing the dental oral professional to carry out procedures while limiting disruptions.
Various behaviour management techniques are employed to help prepare young children for dental procedures. Examples of behaviour management techniques are tell-show-do, positive reinforcement, modelling, behaviour shaping, desensitisation and alternative techniques (flexible control, distraction and memory restructuring).9 Techniques used to improve communication with young children include distraction, non-verbal communication, voice control, tell-show-do, positive reinforcement, parental presence/absence, and protective stabilisation.7,10
To encourage the child to act in a more suitable manner in the dental clinic, the sole use of behavioural management techniques is preferred. However, this is not always possible - especially when working with fearful or anxious children, or with those who have a disability that inhibits them from cooperating with the dental team. Sedation is often needed in paediatric dentistry when the patient presents with behavioural impairment, angst and apprehension to any dental procedures, which prohibits the dental team to commence with treatment.11 Sedation in paediatrics therefore becomes advisable when behavioural strategies alone have failed or are contra-indicated.512
The sedation of children for the delivery of dental care has been successfully executed using different drug regimens. Currently, these are the most popular sedation methods used by paediatric dentists:13,14,12,15
• Nitrous oxide inhalation sedation with oxygen alone
• Midazolam (benzodiazepine) alone, or
• A combination of both drugs.
In addition, in-office sedation is cost-effective and safer than conscious sedation and general anaesthesia. Other options include Dexmedetomidine hydrochloride (Orion Pharma, Turku, Finland) a2-adrenergic agonist, CHLORAL HYDRATE (Pocral®, Hanlim Pharmaceuticals Inc., Seoul, Korea) inhibitory action on the cerebral hemisphere of central nerve system and General anaesthesia [The alternative of oral sedation for paediatric dental care.43
Nitrous oxide
Nitrous oxide (N2O) gas, commonly referred to as laughing gas, is a method used for sedation. N2O2 presents itself as an odourless and colourless gas. The technique is effective because it results in a pleasurable feeling, which in turn relaxes the patient. The drug is fast acting, and its effects can be rapidly and effortlessly reversed when needed. For this reason, it is considered to be a safe method of sedation.16,17,22
Midazolam
Midazolam is a short-acting benzodiazepine derivative used to produce sleepiness or drowsiness and to relieve anxiety before surgery or certain procedures. When Midazolam is used before surgery, the patient will not remember some of the details about the procedure.6,32,33
SEDATION
Most of the reviewed articles only focused on one type of sedation (i.e. either nitrous oxide gas or Midazolam), and not on the combination of nitrous oxide gas and Midazolam. This study specifically looked at those reviews covering the combination of the two sedation methods in order to inform the general dentist, chair assistant and specialist about the outcomes of combining two sedation methods in case of more challenging paediatric patients.
Sedation, which is the consequence of a down regulation of state, is short of anaesthetic sleep. Ideally, sedation produces sleepiness or drowsiness with euphoria and muscular relaxation, but not full anaesthetic sleep. A short time after administration, the agent should be effectively absorbed. The rapid effect of sedation allows treatment to begin almost immediately. The agent should be able to be promptly reversed, allowing for a speedy recovery.
Anxiety tends to lessen the pain threshold. Hence, it is imperative to have an agent that has a sedative effect as well as an anxiolytic effect. Amnesia is a welcome side-effect for sedation and for sedative drugs.5 The General Dental Council (GDC) describes sedation as: 'A technique, of depressing the central nervous system by a drug, allowing for execution of planned treatment to be done whilst maintaining lingual communion throughout the duration of sedation. The sedation level should allow for the reflex behaviours to be maintained to protect the airway specifically the pharynx from aspiration, allow the patient to remain conscious and be able to comprehend and react to spoken instructions.9,21 Many different drugs have been employed to effectively sedate paediatric patients during dental care treatment.9
One of the more favourable sedation techniques used by paediatric dentists is the combined use of the inhalation of nitrous oxide (N2O) and oxygen (O2), as a sedation alone or, in combination with Midazolam.22 Moderate sedation can be successfully administered in the clinical management of a paediatric dental patient, with both intranasal and oral sedation using Midazolam in combination with nitrous oxide gas.23,15
SEDATION IN THE PAEDODONTICS PRACTICE
Team effort and discussions are required to decide whether or not to sedate a paediatric patient. Decisions about which sedation technique to use, the mode of delivery and the type of agent depend on the suitability of the sedation techniques for that child and caregiver. General anaesthesia (GA) in paediatric patients is always risky for the following reasons:17
• Children have a somewhat larger epiglottis and tongue
• The head-to-body ratio of children
• Children have a different (higher) metabolic rate compared to adults
• Children's adenoid mass
• Children's anterior and higher vocal cords
• Children have a smaller, less developed and retrog-nathic mandible
• Children have a smaller lung capacity
• Children have less oxygen reserves, so they can de-saturate more quickly than adults do.
An effective drug should assist with anxiety management (anxiolysis) using minimal sedation and allowing patients to respond naturally and routinely to verbal commands.
Cardiovascular and upper respiratory functions should remain unaffected. However, cognitive function and physical coordination may be impaired.24
PATIENT SELECTION
When selecting a specific form of sedation, the pre-operative evaluation should comprise a meticulous medical history (including all chronic and acute medication) and dental history, prior hospitalisations and operations. In addition, according to the American Society of Anesthesiologists (ASA), physical status classification ought to be determined as part of the patient's assessment.25 Table II below summarises the ASA classification.
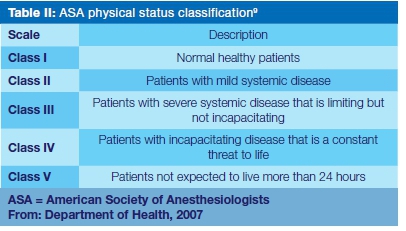
Paediatric patients who fall under ASA Class I or Class II (see Table III) are deemed fit to receive sedation in a general paediatric practice. Those in Classes III to V should be treated in a hospital environment.9 Should the child have a history of recent respiratory illnesses or common infections, then the airway, weight and vital signs should be assessed before general anaesthesia is administered.
The employment of basic monitoring devices such as a pulse oximeter and blood pressure cuff is somewhat mandatory for lighter sedation techniques and highly recom-mended.17
PATIENT MONITORING
Regulatory bodies and professional associations with advanced technology have provided the framework for the safe and effective practice of patient sedation. Clinicians' sedation techniques in earlier times were largely unregulated, usually only relying on direct clinical findings such as physical rate of respiration and signs of cyanosis to assess the sedated patient.26 Safety increased when regular monitoring became normal practice. Observation includes the use of a pulse oximeter for the electronic monitoring of blood oxygen saturation levels, pulse and blood pressure.27 An oxygen saturation level of 90 O2 or below should be seen as alarming for a 4- to 6-year-old patient undergoing a dental procedure (a level of 95 O2 and above is acceptable).
INHALATION SEDATION
The technique of inhalation sedation analgesia using nitrous oxide gas can be used to control pain. Nitrous oxide gas is a weak anaesthetic agent that is very useful in alleviating anxiety in patients. The use of N2O is safe and effective for children who are anxious but cooperative. It is a reasonably simple technique to use as an adjunct to dental care, assisting patients to accept routine operative dental care. The acceptance of the mask can be made more favourable when lending out the mask to the patient and parents to role-play at home. This makes inhalation sedation a safe and relatively easy technique to use. In addition, inhalation sedation has a quick induction and it is completely reversible, with a short recovery time. Nitrous oxide gas can be titrated to the desired level of sedation. Contra-indications include, but are not limited to, a blocked nose, severe psychosis, cystic fibrosis, chronic upper airway obstructions (due to large adenoids), intercommunication problems, reluctant patients, pregnancy and acute respiratory tract infections.28 Nausea is often induced due to fluctuating concentrations of N202 resulting in alternative mouth and nose breathing. Patients receiving nitrous oxide sedation may continue with their normal daily routines upon discharge from the practice or clinic.29
Nitrous oxide (N2O) inhalation sedation is used by 85% of paedodontics for dental sedation.6 However, it has a proven high-technique sensitivity and as a single-drug sedation it has a low potency. In order to overcome the shortcomings of both drug routes, i.e. Midazolam and N2O, the N2O inhalation technique is frequently used in combination with oral medications.6,30,31
ORAL SEDATION
Oral sedation is one of the most popular routes due to the ease of administration for most children. Benzodiazepines, Midazolam, chloral hydrate, ketamine, hydroxyzine, Promazine and Fentanyl are commonly used drugs in this context.
The popularity and usage of Midazolam has increased over the past decade due to its safety record and short-acting nature. It allows for relatively quick recuperation and for the almost immediate safe discharge of the patient. The oral dosage of 0.3 to 0.7mg/kg, and a maximum dose of 10mg for older children, is used.17
An example of an ideal situation is the following:
• Child: aged 6 to 8 years
• ASA classification: 1 or 2
• Type of procedures: short procedures
• BMI: should be ideal
• Discharge: Caregiver able to look after child after procedure.
Children older than six years may be more difficult to manage due to them being more disinhibited and having more paradoxical reactions while children with a higher BMI may have trouble with airway management. Children should have fasted for a few hours to avoid vomiting after the procedure. A significant limitation of the oral route is that it cannot be titrated accurately as it has a hepatic metabolism route, unlike gas which is easier to titrate.10
COMBINATION OF AGENTS
To achieve a deeper form of sedation, nitrous oxide, oxygen and hypnotic agents (benzodiazepines, anti-histamines, chloral hydrate and opioids) may be com-bined.1'32,33'34'35,36 Midazolam and nitrous oxide in amalgamation with oxygen are the pharmacological agents mainly used for the treatment and management of dental anxiety, mainly in children.19
Nitrous oxide given concurrently with drugs like Mida-zolam increases its effect.37 Various research articles have recorded the efficiency and safety of using nitrous oxide with other sedative drugs in children who were uncooperative. Nitrous oxide potentiates the sedative effects of benzodiazepines in sedation. The N2O mixture enhanced the duration of action of the Midazolam, and this duration was well suited to the dental environment.2 Although successful sedation events were established, an elevated occurrence of overdose was associated due to adverse sedation events when combinations of drugs were administered.36
In children with cerebral palsy, Valium can be used as its side-effects include drowsiness due to its antihistamine properties. The draw-back is its long half-life.38
In the 2018 article by Bourke and Phadraig, it was found that nitrous oxide and Midazolam as sedative agents were uniformly safe and effective for the use in healthy young children in a hospital setting.1 Both trials on nitrous oxide and Midazolam observed no incidence of patients suffering respiratory depression, with a low prevalence of excitatory behaviour. Any desaturation recorded remained inside acceptable clinical limits in all trials. This emphasised the safety of both these techniques. While testing Midazolam and nitrous oxide separately, they found that the Midazolam and nitrous oxide had fairly identical results relating to behaviour management and sedation. However, in a single experiment they found nitrous oxide to be more effective than oral Midazolam in relieving anxiety, and with fewer adverse effects.39,40 Sole pharmaceutical treatment with a single dose of Midazolam took longer than with nitrous oxide to gain effectiveness.1 Poor behaviour of paediatric dental patients has shown no effect on oxygen saturation. However, it has predictably shown an increase in the pulse rate of children under sedation with Midazolam and nitrous oxide.41 There were no significant differences in the general behaviour of patients when using either the nitrous oxide or the Midazolam technique. However, the combination of nitrous oxide and Midazolam helped with stressful situations such as injections of local anaesthesia, sleep drowsiness, crying and movements.15 As a result, nitrous oxide or oxygen at 40% with Midazolam may allow the patient to tolerate unpleasant procedures by reducing discomfort, anxiety and/or pain.41
In a Drug Bank study, 0.5 mg/kg Midazolam, 1 mg/kg Promethazine and 50% N2O/50% oxygen were administrated, which was in line with previous investigations where the subjects presented with amnesic effects.18 Adding N2O is permitted with all sedation methods, leading to increased sedation and improved oxygen delivery to the patient.18 A concentration of 50% N2O/50% oxygen provides a safe anxiolytic/analgesic effect by activating the opioid and gamma-aminobutyric acid receptors.4 Preceding researchers advocated 0.5 mg/kg Midazolam, as no difference was seen in sedating efficacy of 0.5, 0.75, and 1 mg/kg Midazolam and some side-effects were reported with 1 mg/kg Midazolam.18
CHALLENGING ROLE OF DENTAL ANAESTHESIA
Children's behaviour in the dental office is becoming more difficult to manage, which is aggravated by parents becoming increasingly particular about their child's experience and interfering with treatment. In addition, sedation dental practitioners face considerable challenges to achieve the described levels of child-centred care.27
CONCLUSION
Providing superior dental care to young paediatric patients can be challenging. Preserving the child's trust by providing minimal traumatic treatment is the main objective of paediatric dental sedation and treatment. To specifically create a high standard for safety and to incorporate this into the clinical practice, practitioners should strive to reduce patient risk by vigilantly selecting patients who are medically sound for sedation.
Two of the main strategies used to deal with anxious children are behaviour management and sedation. Usually, when behaviour techniques are no longer sufficient to manage the child, the help of pharmacological substances is sought. A critical review of journal articles on the use of nitrous oxide (N2O) and oxygen (O2), as a sedation alone, or in combination with Midazolam, was therefore undertaken. The findings suggest that, in order to achieve a deeper form of sedation, the combination of nitrous oxide, oxygen and a hypnotic agent such as Midazolam works well, allowing paediatric patients to tolerate unpleasant procedures by reducing discomfort, anxiety and/or pain.
It is anticipated that the need for safe dental sedation will grow in the future, given the parents' preference and the towering incidence of paediatric dental disease.26,27
References
1. Bourke M, Mac Giolla Phadraig C. Nitrous oxide versus midazolam for paediatrics. J Ir Dent Assoc. 2018 April/ May; 46(2):88-95. [ Links ]
2. Wood M. Specialist in special care dentistry: The safety and efficacy of intranasal midazolam sedation combined with inhalation sedation with nitrous oxide and oxygen in paediatric dental patients as an alternative to general anaesthesia. Louton, Bedfordshire: Leagrave Dental Sedation Clinic. [ Links ]
3. Myers GR, Maestrello CL, Mourino AP. Effects of submucosal midazolam on behaviour and physiologic response when combined with oral chloral hydrate and nitrous oxide sedation. Pediatr Dent. 2004; 26:37-43. [ Links ]
4. Mozafar S, Bargrizan M, Golpayegani MV, Shayeghi S, Ahmadi R. Comparison of nitrous oxide/midazolam and nitrous oxide/promethazine for pediatric dental sedation: A randomized, cross-over, clinical trial. Dent Res J. 2018 Nov-Dec; 15(6):411-19. [ Links ]
5. American Academy of Pediatrics. Age limits of pediatrics. 1988 May; 81(5):736. Available from: https://pediatrics.aappublications.org/content/81/5/736 [ Links ]
6. Dean JA, Avery DA, McDonald RE. Dentistry for child and adolescent. 10th ed. Indiana: Mosby Publication; 2016:303-20. [ Links ]
7. Council on Clinical Affairs. Guideline on behavior guidance for the pediatric dental patient Pediatric Dentistry Reference Manual. 2014; 36(6):179-191. [ Links ]
8. 8) American Academy of Pediatrics; American Academy of Pediatric Dentistry. Guideline for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures. Pediatr Dent. 2008; 30:143-59. [ Links ]
9. Adamji R, Holroyd I, Ashley P. Conscious sedation for anxious children. Dental Nursing. 2009 Sept; 5(9). Available from: https://doi.org/10.12968/denn.2009.5.9.43719 [ Links ]
10. Roche. Dormicum (Midazolam). Mims. [2015 Apr; cited 2019 Feb 21]. Available from: https://www.roche.com.sg/content/dam/rochexx/roche-com-sg/documents/product-page/Dormicum%20Tab%20Nov%202017%20PI.pdf. [ Links ]
11. Baygin O, Bodur H, Isik B. Effectiveness of premed-ication agents administered prior to nitrous oxide/ oxygen. Eur J Anaesthesiol. Apr 2010; 27(4):341-6. Doi: 10.1097/EJA.0b013e3283313cdd [ Links ]
12. Folayan MO, Faponle A, Lamikanra A. A review of the pharmacological approach to the management of dental anxiety in children. Int J of Pediatric Dentistry. 2002 Sep; 12(5):347-54. [ Links ]
13. Peretz, B, Kharouba J, Somri M. A comparison of two different dosages of oral midazolam in the same pediatric dental patients. Pediatr Dent. 2014 May-Jun; 36(3):228-32. [ Links ]
14. NHS education for Scotland. Conscious Sedation in Dentistry. Dental Clinical Guidance. 2017. Available from: http://www.sdcep.org.uk/wp-content/up-loads/2018/07/SDCEP-Conscious-Sedation-Guidance.pdf. [ Links ]
15. Al-Zahrani AM, Wyne AH, Sheta SA. Comparison of oral midazolam with a combination of oral midazolam and nitrous oxide-oxygen inhalation in the effectiveness of dental sedation for young children. J Indian Soc Pedod Prev Dent. 2009 Jan-Mar; 27(1):9-16. [ Links ]
16. Colgate. What does laughing gas do? [cited 2019 Feb 20]. Available from: https://www.colgate.com/en-us/oral-health/procedures/anesthesia/what-does-laughinggas-do-0117 [ Links ]
17. Alcaino EA, McDonald J, Cooper MG, Malhi S. Pharmacological behaviour management. In: Cameron AC, Widmer RP, editors. Handbook of Pediatric Dentistry. 4th ed. Amsterdam: Elsevier, 2013, p. 25-46. [ Links ]
18. Tavassoli-Hojjati S, Mehran M, Haghgoo R, Tohid-Rahbari M, Ahmadi R. Comparison of oral and buccal midazolam for pediatric dental sedation: A randomized, cross-over, clinical trial for efficiency, acceptance and safety. Iran J Pediatr. 2014; 24:198-206. [ Links ]
19. Drug Bank. Midazolam. [cited 2019 Feb 20]. Available from: https://www.drugbank.ca/drugs/DB00683 [ Links ]
20. Medscape. Midazolam. [cited 2019 Feb 2]. Available from: https://reference.medscape.com/drug/versed-midazolam-342907 [ Links ]
21. Pitts T. Airway protective mechanisms. Lung. 2014 Feb; 192(1):27-31. [ Links ]
22. Litman RS, Berkowitz RJ, Ward DS. Levels of consciousness and ventilatory parameters in young children during sedation with oral midazolam and nitrous oxide. Arch Pediatr Adolesc Med. 1996; 150:671-75. [ Links ]
23. Venchard GR, Thomson PJ, Boys R. Improved sedation for oral surgery by combining nitrous oxide and intravenous midazolam: A randomized, controlled trial. Int J Oral Maxillofac Surg. 2006; 35:522 27. [ Links ]
24. Rodrigo MR, Cheung LK. Oral midazolam sedation in third molar surgery. Int J Oral Maxillofac Surg. 1987; 16:333-37. [ Links ]
25. Saklad M. Grading of patients for surgical procedures. Anesthesiology. May 1941; 1(3):281-284. [ Links ]
26. Nelson T, Xu Z. Pediatric dental sedation: Challenges and opportunities. Clin Cosmet Investig Dent. 2015 Aug; 7:97-106. [ Links ]
27. Musani IE, Chandan NV. A comparison of the sedative effect of oral versus nasal midazolam combined with nitrous oxide in uncooperative children. Eur Arch Paediatr Dent. 2015; 16:417 24. [ Links ]
28. 28) Houpt MI, Livingston L, Livingsone R. Clinical effects of nitrous oxide conscious sedation in children. Pediatr Dent. 2004; 26:29 36. [ Links ]
29. obias JD. Applications of nitrous oxide for procedural sedation in the pediatric population. Pediatr Emerg Care. 2013; 29(2):245-65. [ Links ]
30. Thompson JM, Neave N, Moss MC, Scholey AB, Wesnes K, Girdler NM. Cognitive properties of sedation agents: comparison of the effects of nitrous oxide and midazolam on memory and mood. Br Dent J. 1999; 187:557-62. [ Links ]
31. Litman RS, Berkowitz RJ, Ward DS. Levels of consciousness and ventilatory parameters in young children during sedation with oral midazolam and nitrous oxide. Arch Pediatr Adolesc Med. 1996; 150:671-75. [ Links ]
32. Ozen B, Malamed SF, Cetiner S, Ozalp N, Ozer L, Altun C. Outcomes of moderate sedation in paediatric dental patients. Continuum of depth of sedation: Definition of general anesthesia and levels of sedation/analgesia. Aust Dent J. 2014; 57:144-50. [ Links ]
33. Seth RW, Theophilos T, Babl FE. Intranasal fentanyl and high-concentration inhaled nitrous oxide for procedural sedation: a prospective observational pilot study of adverse events and depth of sedation. Acad Emerg Med. 2012; 19(1):31-6. [ Links ]
34. Soldani F, Manton S, Stirrups DR, Cumming C, Foley J. A comparison of inhalation sedation agents in the management of children receiving dental treatment: a randomized, controlled, cross-over pilot trial. Int J Paediatr Dent. 2010; 0(1):65-75. [ Links ]
35. Cote CJ, Notterman, HW, Karl DA. Adverse sedation events in pediatrics: analysis of medications used for sedation. Pediatrics. 2000; 160(4):633-44. [ Links ]
36. Klein U. N2O/O2 sedation in pediatric dentistry. In: Brunick A, Clarke MS, editors. Handbook of nitrous oxide and oxygen sedation. 4th ed. Amsterdam: Elsevier, 2015, p. 164-85. [ Links ]
37. Blumer S, Iraqi R, Bercovich R, Peretz B. Oxygen saturation and pulse rate change in children during sedation with oral midazolam and nitrous oxide. J Clinical Pediatric Dentistry. 2018; 42(6):461-64. [ Links ]
38. Levy H. General dentistry for children with cerebral palsy. New York: Springer. 2018. [ Links ]
39. Chala HR. Pharmacological and non-pharmacological treatments for anxiety to the dental treatment. Rev Cubana Estomatol. 2016; 53(4). Available from: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-75072016000400010 [ Links ]
40. Bourke M, Phadraig CMG. Nitrous oxide versus midazolam for paediatrics. JIDA. 2018; 64(2):88-95. [ Links ]
41. Cameron AC, Widmer RP, editors. Handbook of pediatric dentistry. 4th ed. Amsterdam: Elsevier, 2013. p. 25-46. [ Links ]
42. 42) Van Heerden J, Delport R, Kruger M. Children's ability to consent to medical management in South Africa. S. Afr. J. Child Health., 2020;14(1):25-29. [ Links ]
43. Kim J, Kim S, Lee D-W, Ryu D-S. The alternative of oral sedation for pediatric dental care. Dent Anesth Pain Med. 2015 Mar; 15(1):1-4. Available from: https://doi.org/10.17245/jdapm.2015.15.1.1 [ Links ]
 Correspondence:
Correspondence:
Dr G Streit
coastal.dental.clinic@gmail.com
Author contributions:
1 . Nicoline Potgieter: Conception, Editing and Writing 30%
2 . Günther Streit: Conception, Editing and Writing 70%














