Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.76 n.6 Johannesburg Jul. 2021
http://dx.doi.org/10.17159/2519-0105/2021/v76no6a3
RESEARCH
Oral health knowledge, attitudes, and practices of undergraduate students at a South African University of Technology
FF Mbele-KokelaI; R MoodleyII
IB Dent Ther, Masters Student, Discipline of Dentistry, University of KwaZulu-Natal, Durban, South Africa
IIPhD, Lecturer, Discipline of Dentistry, University of KwaZulu-Natal, Durban, South Africa. ORCID Number: 0000-0002-0171-0595
ABSTRACT
BACKGROUND: Awareness of oral health is essential for developing healthy habits, and a correlation between improved knowledge and better oral health has been shown to exist. Health-related behaviours are more likely to be followed if a person has greater control over their health with a better understanding of diseases and their aetiology.
OBJECTIVES: To determine the knowledge, attitudes, and practices regarding oral health care among undergraduate students in the Life Sciences Department at a University of Technology, Free State.
METHODS: This descriptive study gives insights into the oral hygiene knowledge, attitudes, and practices of undergraduate students in the Faculty of Health and Environmental Sciences, Department of Life Sciences at a University of Technology. Data were collected using an online questionnaire eliciting quantitative and qualitative data.
RESULTS: The results revealed that most of the participants, 80% (n=178) understood that oral health is essential to their overall wellbeing. Overall, in this research, the findings of oral health education were found not to be covered. However, we found that variations in the source of dental information were correlated with university students' oral health behaviour.
CONCLUSION: The study, therefore, concludes that oral health care knowledge, attitudes and practices are affected by education and show that advocacy for the promotion of oral health is significant for the students.
INTRODUCTION
Oral health is a primary predictor of health, nutrition, and overall quality of life.1 Furthermore, one should be free from oral cancer and infection, periodontal diseases, tooth decay, tooth loss, and any facial disorders that impair a person's ability to bite and chew.2 However, in South Africa, oral disease is still a health problem and a considerable burden, which often leads to pain and more significant loss of the tooth.
This disease affects appearance, quality of life, consumption of nutrients, and thus growth and development.3 The 2020 mid-year population estimates from Statistics South Africa (Stats SA) were estimated at 59.62 million. Around 51,1% (about 30.5 million) of the population is female.
The ages of the participants in this study ranged from 18 to 24 years, with the majority being females, in line with South Africa's gender demographics. Stats SA also provides data that suggests that participation in post-school institutions has increased over the past two decades, primarily due to the rise in government support for the sector. However, the nation is still struggling to meet the increasing educational needs of young people and demand skills from the market.
According to the Higher Education and Skills in South Africa 2017 report, in 2016, the life science and physical sciences intake in Universities was 3.3% of females and 2.8% males while a majority of 51% of those that did not attend university stated that they did not have money to pay the fees.
The development and preservation of good general and oral health is a priority and a key factor in enabling adults to achieve overall wellbeing and enhanced quality of life. Therefore, it is essential to determine how people rate their oral health status, their perceived dental needs, and the actual use of available dental services.4 Ghaffari et al. (2018) suggested research that supports that better oral care practices are presented through proper oral health awareness.5 In addition to this, a positive attitude toward oral health practices facilitates improved oral health habits.5
The literature suggests that integrated dental services should be part of every educational institution where oral health education and oral health screening are provided. Students can access dental services through funding, i.e. simple dental payment systems, including scaling and polishing, restorations, Assure sealants, and relief of sepsis, making things easy and accessible for all students.6,7
Of concern among students is alcohol consumption, smoking, and sugary intake, which peaks between 18 and 25. University students in this age group are at particular risk because of increased alcohol consumption than non-enrolled individuals.8 Ramphoma (2016) noted that even though oral health has an impact on general health, in South Africa, it is still one of the most overlooked aspects of health.9
This is the first study evaluating oral health that was conducted at a University of Technology. Even though research suggests that structures such as school health-based and community-based programmes are in place to promote behaviour practices in oral health, it is crucial to remember how the knowledge, attitudes and practices (KAP) are applied, as investigated in this study.
BACKGROUND
Oral health is now an essential component of general health, and oral health awareness is growing worldwide.8 The Global Oral Health Program of the World Health Organization has done much in the past Ave years to raise awareness.8 Furthermore, 3.5 billion people worldwide suffer from oral diseases, with the most prevalent non-communicable diseases of untreated dental caries, with an established oral and general health relationship.
For example, diabetes mellitus is associated with the development and progression of periodontitis. In addition to the previous statement, there is a causal correlation between high intakes of sugar and non-communicable disorders such as cardiovascular disease and diabetes.8,10
Literature suggests that adults' periodontal health impacts their smiling patterns and their quality of life-related to smiles. Furthermore, poor periodontal health also prevents positive emotions from being expressed by adults, which can, in turn, affect their self-conception and social interactions.11 Evidence supports that problems with oral health can, in several ways, affect the quality of life. Poor oral health can stop students from expressing positive emotions that can affect their social interactions and how they feel about themselves.11
According to Sheiham (2005), some of the risk factors causing oral health disorders worldwide are poor oral hygiene, diet and smoking.12 Additionally, poverty remains the primary determinant of oral health disorders in Africa, predisposing people to a lack of information and poor lifestyle choices.13 In South Africa, there is a high dental caries rate despite public and private services being available. While access is a problem, the knowledge of preventative measures is also very low.14,15
The outcomes of a study done about oral health-related knowledge, attitudes and practices of adult patients in Mangaung Metropolitan Municipality could be used to enlighten the planning of integrated oral health promotion plans, in Mangaung and the Free State Province of South Africa.15 A similar study done in KwaZulu-Natal among undergraduates about knowledge and attitudes in oral self-care practices showed that although oral diseases cannot be avoided, they can be prevented through simple tooth brushing measures twice a day with a fluoride toothpaste but that alone is also not enough.16
With an increased awareness of health and self-care in schools, this study aimed to establish the students' general knowledge, attitudes, and practices concerning oral health care.
OBJECTIVES OF THE STUDY
The objectives were to determine the students' knowledge regarding oral health care, explore the students' attitudes towards dental care, and establish the students' practices regarding oral health and hygiene using an online questionnaire.
METHODS
The study was conducted among undergraduate students at a University of Technology. This University of Technology is in Bloemfontein in the Free State province of South Africa. Ethical approval was obtained from the Humanities and Social Sciences Research Ethics Committee from UKZN (HSSREC/00001570/2020) and thereafter from the Life Sciences Department.
All principles and policies of the UKZN HSSREC were adhered to throughout the study. An online information sheet was uploaded on QuestionPro for all participants in the study to access easily. Informed consent was obtained from the participants online. Participants could withdraw from the study at any stage.
All 260 participants in the Department of Life Sciences were invited to participate during October 2020. A pilot study was conducted on ten students to determine if the students will understand the questionnaire. Thereafter minor changes were made to the research tool.
This was a cross-sectional descriptive study design that used both quantitative and qualitative methods. Data were collected from an online survey questionnaire during October 2020 using QuestionPro. An email contact list was acquired through the programme coordinators, and the link to the study was sent to participants via email. Students were also sent the link via their WhatsApp groups. The questionnaire consisted of five sections: demographics, habits, knowledge, attitudes, and practices. A curriculum checklist was used to review the modules offered in the first year for both two programmes.
Both quantitative and qualitative methods were used for this. Quantitative data in response to each question was entered into an Excel spreadsheet and analysed with SPSS version 26.0. The results present the descriptive statistics in graphs, cross-tabulations, and other figures for the collected quantitative data. Inferential techniques included the use of correlations and chi-square test values, which were interpreted using the p-values. The traditional approach to reporting a result requires a statement of statistical significance. A p-value was generated from a test statistic. A significant result is indicated with "p<0.05".17
The qualitative analysis included an analysis of the targeted curriculum review and thematic analysis of long answer questions. The results from the groups were added to an excel spreadsheet and compared. A curriculum checklist was used. The method used to analyse qualitative data was content analysis by following the steps defined by Braun and Clarke (2006), using a thematic process.18
RESULTS
Demographic data
Overall, the ratio of males to females was approximately 1:2.3 28.4% (n=62): 70.2% (n=153) with 1.4% (n=3) classifying themselves as other (p<0.001). Within the age category of 22 to 24 years, 28.2% (n=60) were male.
The age distributions are not similar as there are more respondents (90%; n=189) younger than 24 years (p< 0.01). This study reported that many respondents lived at home 44.5% (n=97) and private residences 39.9% (n=87), while a smaller number lived on campus 15.6% (n=34) (p<0.001).
Habits
Participants were asked about their habits of drinking alcohol and smoking. Nearly 72% (n=160) had never smoked while 26.6% (n=58) smoked. In this category, it was noted that more males smoke than females.
An overwhelming 99.1% (n=218) of participants (n=220) have had an alcoholic drink. Over 60% (n=132) drink over seven alcoholic drinks per week. Habits were also structured around the participant's sugar intake, and in our study, over 80%; (n=187) of the participants agreed that they love sugar.
Figure 1 provides data on habits about toothbrushing which show significantly different patterns (p<0.001) where more than 63% (n=138) confirmed to brushing their teeth twice a day while only 31% (n=68) brushed once a day.
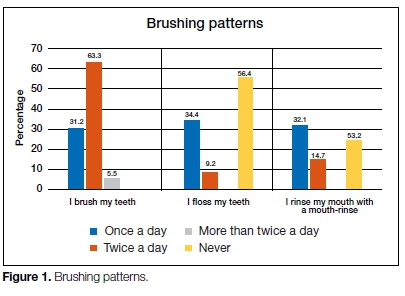
In this study, 56.4% (n=123) of the participants confirmed that they had never flossed before, while 53.2% (n=11 6) stated they had never used a mouth-rinse before. Nearly, 68.8% (n=150) of the participants provided information that suggested that they brush their teeth twice a day, in the morning and before going to bed, whilst a smaller number, 5% (n=12) brushed three times a day.
The significance of the differences in habits was noted in the participants. The higher levels of disagreement imply that respondents consider their breath, teeth, and gums healthy or acceptable. A small number 13.8% (n=30) indicated that they had bad breath, and 31.7% (n=69) indicated missing teeth. A further 24.7% (n=54) indicated that they had bleeding gums.
Knowledge
Participants provided significantly higher levels of agreement regarding their knowledge of oral health. Over 51% (n=112) agreed that smoking could affect their gums, while 64,2% (n=159) believed that dental caries is caused by a combination of sugar, bacteria, and poor oral hygiene. However, a significant 86,7% (n=189) supported the statement that supports brushing twice a day to keep their teeth clean and healthy.
Attitudes
The participant's responses towards their oral health care attitudes indicated that out of the participants (n=220), over 94% (n=206) agreed that taking care of their oral hygiene was important, and about 67% (n=146) visited the dentist twice a year. Only a few with a response of 8,4% (n=18) indicated that taking care of their oral hygiene was not important in the present time of Covid-19 with everyone wearing a mask. Few of the participants, 29,4% (n=64), believed that one could get heart diseases from bad oral health.
Practices
About 65% (n=141) of participants believed they should brush their teeth for two minutes, while 29,3% (n=63) suggested there is no need to visit a dentist if they have no problems orally. Oral hygiene techniques such as brushing twice daily (36.9%) and flossing (7.5%) were recorded and identified by many dental assisting students. Interestingly, most participants, 64,9% (n=141) agreed that they had been taught about oral health in school, but their habits prove otherwise, as discussed above.
All open-ended questions are reported in the tables below. Participants were asked to reflect on their oral health care while exploring their knowledge, attitudes, and practices. The responses were summarised from QuestionPro and supported with quotes, and these were analysed thema-tically. In our study, out of n=220 participants, 34% (n=75) were from Dental Assisting (DA) and 65.9% (n=145) from Environmental Health (EH).
It must be noted that the participants could give multiple responses. The participants were asked, "what is plaque?" Out of (n=220), more than 41% (n=91) stated it was a layer of bacteria in the teeth. A few participants, 14%; (n=38) stated it was dirt on the teeth, while a 6.3% (n=14) believed that it was a calcified deposit on teeth. However, the rest 37.9% (n=77) of the participants stated they did not know what plaque was. Themes and frequencies are shown in Table 3 below.
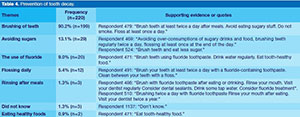
Participants reflection on the prevention of tooth decay
Participants were asked: "How can you prevent tooth decay?" 90.2% (n=199) responded, "by brushing twice a day". While there were multiple responses, only a few did not know how 1.3% (n=3). Themes and frequencies are shown in Table 4 below.
Participants reflection on the sequelae of poor oral hygiene
Participants were asked: "What happens if you do not clean your mouth?" The responses indicated that they were aware that tooth decay is caused by bacteria and plaque build-up from not brushing regularly. Below are themes and frequencies (Table 5).
Reason for visiting a dentist
Respondents were asked if they had ever been to a dentist, dental therapist, or an oral hygienist. Overall, 58% (n = 129) stated yes and 31.3% (n=69) had not been to either one. Out of the 58% (n=129) that stated they have been to one and the majority, 36% (n=78) indicated that it was mainly for extraction (Table 6). A slightly lower number, 15% (n=34), stated that they did not have money to go to a dentist/therapist or a hygienist. Themes are reflected in Table 7.
Table 8 reports that about 32% (n=72) of the participants did not understand how the state of one's oral health can affect their general health. They indicated that they did not know the relationship between the two. In comparison, only 44.5% (n=98) had an idea. Table 9 reports on the methods of cleaning teeth, its themes, statements, and frequencies. The respondents were asked what methods they used to clean their teeth. The majority 99% (n=218) stated they brushed with toothpaste and a toothbrush.
DISCUSSION
In this study population, we found that variations in the source of dental information were correlated with oral health behaviour; both positive and negative associations were observed between the sources and oral health behaviour.
The ages of the participants in this study ranged from 18 to 24 years, with the majority being females, in line with South Africa's gender demographics. Overall, the ratio of males to females is approximately 1:2.3; 28.4% (n=62): 70.2% (n=153). Participants reported to be living at home were 45% (n=97) which might influence their oral hygiene methods. This statement is supported by a study conducted in Mangaung, Free State, South Africa where oral health care knowledge, attitudes, and practices among adult patients was researched..15
Modikoe et al. (2019) suggest that living at home could influence oral hygiene methods in a good or bad way to fight dental caries.15 However, the correlation between students staying at home and toothbrushing in our study revealed no degree of association or significance - between the number of household individuals and toothbrushing habits of the participants. Our research noted that significantly more males 26.6% (n=58) smoked than females. Interesting enough, over 51% (n=114) in our study, agreed that smoking could influence their gums.6,19 Formicola (2017) and Park et al. (2011) found that tobacco use may influence students' oral hygiene methods.6,19 An analysis of smoking and bleeding gums was done, and no significant difference was found in our study.
Almost all the participants, 99.1% (n=218) have had an alcoholic drink, and of the 99%, over 60% (n=132) drink over seven alcoholic drinks per week. These findings might influence the participants' oral hygiene as seen in a study conducted by Afshin et al. (2019).8 It was observed that the overall trend of alcohol use increased among students. Furthermore, the systematic analysis for the Global Burden of Disease Study done in 2017 suggested that alcohol intake influenced students in all educational institutions regarding their lifestyle.8
This study's habits were also structured around the participant's sugar intake as reported in a study conducted by Modikoe et al., (2019), whose findings indicated a low intake of vegetables and more sugary products in adults. In our study, over 80%; (n=187) of the participants agreed that they love sugar and only 14%; (n=32) do not like sugar.15 Over 22%; (n=50) stated that they take sugar more than three times a day.
Their intake of sugar is to be noted, as it is significantly high. There was a strong and significant positive correlation between high sugar levels, bad breath and missing teeth using the Pearson Chi-Squared Test (p = 0.01). This finding is also to be noted as 72.2% (n=159) participants believed that a combination of sugar, bacteria causes dental caries and poor oral hygiene, but the results of their drinking and smoking habits prove otherwise.
Oral health knowledge
More than 63% (n=138) participants confirmed brushing their teeth twice a day, and 31% (n=68) brushed once a day. Taniguchi-Tabata et al. (2017) cited that oral health education successfully modified students' oral health behaviour.26 However, this research study's findings further suggested that participants did not use oral hygiene strategies such as dental floss (56.4%; n=123), or have ever used a mouth-rinse (53.2%; n=116). The findings in our study are close to that of a research carried out by Ghaffari et al. (2018), where it was concluded that oral health problems have a considerable effect on the quality of life of individuals.5
Similar patterns were observed in another study conducted by Taniguchi- Tabata et al., (2017) among Japanese university students on dental knowledge. It was indicated that school is important as a source of dental awareness for oral health education.26 In addition, dental awareness from dental clinics may effectively improve oral health behaviour, as Taniguchi-Tabata et al. (2017) stated.26 In our study, majority of the participants 62% (n=140) indicated that they are aware that tooth decay is caused by bacteria and plaque build-up from not brushing regularly; however, the findings of oral health education were found not to be covered.
Oral health attitudes
In our research, an area of concern was when the participants were asked about why they had to visit a dentist, dental therapist, or an oral hygienist. Nearly 58% (n=129) stated yes and 31.3% (n=69) had not been to either one. Out of the 58% (n=129) that stated they have been to one, the majority 36% (n=78) indicated that it was mainly for extraction. The research explored by Silva and Oliveira (2018) suggested that the outcomes for primary care oral health services have shown that areas with lower coverage for dental services are more prone to oral health problems.27
In our study, fifteen percent (n=36) indicated that they did not have money to go to a dentist/therapist or a hygienist. Pain and sepsis could hinder students from going about their daily life, as defined, and supported through research by (Glick et al., 2016) through the FDI World Dental Federation's definition of oral health.2
Research further notes the mouth as multifaceted that involves the voice, smile, smell, taste, touch, and chew. Additionally, it is used to swallow and communicate a spectrum of emotions through confident and painless facial expressions of the craniofacial complex.2 Furthermore, poor oral health care could compromise the functioning of the oral cavity needed for mastication.20
University students are aware of their oral health and appearance, pain and cavities could affect their confidence levels and progress. If students have bypassed school and are now at the university level with oral hygiene issues, oral health education needs to be reviewed at school level.
Peltzer and Pengpid (2014) conducted a study in developing countries, including SA. The results suggested that oral hygiene education in our country was associated with weak oral health habits.21 These findings suggest that oral hygiene may not have been adequately incorporated into the secondary education system.21 Notably, there was strength in toothbrushing rates from the participants in our study.
Dental care is expensive even in high-income environments, averaging five percent of overall health spending and 20% of out-of-pocket health expenditure.9,22 Sarpkaya et al. (2018) suggested that the Universal Health Coverage should support activities that would help frame policy dialogue and resolve weak primary oral health programs. Furthermore, to resolve high out-of-pocket oral health care costs in SA, a simple dental payment system would assist the students, as cited in a study considering students' cost of dental education by Formicola (2017). This study's outcomes suggest that oral health care campaigns would benefit the students, and free oral health screening and discounted dental services could be offered to students.
Oral health practices
This study's findings suggest that the majority, 86,7% (n=191), brushes twice a day to keep their teeth clean and healthy. This is supported by Al-Hussaini et al.'s (2003) research on dental health knowledge among students at Kuwait University that suggests what university students know about oral health care.23
The literature further supports the results of our study. Azodo et al. (2010) researched students in Nigeria and concluded that most students were aware that oral health is an aspect of general health and affected everyday life.4
However, 32% (n=72) did not know the correlation between oral and general health. Thus, the study advocated maintaining proper oral health which relies on implementing habits, such as dental check-ups, frequency of toothbrushing, food and sugar intake, dental floss, and other interproximal cleaning techniques. In the prevention of dental caries and periodontal disease, these practices play an important role as adequate oral hygiene habits and the frequent use of dental services have shown efficacy in reducing the prevalence of these diseases as well as in preventing them.24
Our study noted a marked difference between Dental Assisting (DA) and Environmental Health (EH) students in the reported oral health knowledge and practices. Oral hygiene techniques such as brushing twice day were recorded (36.9%), and flossing (7.5%) were identified from (DA) students. The dental assisting group knew there was a correlation between oral health and general health. Nearly 29,4% (n=64) DA believed that one could get heart diseases from bad oral health while a small number from DA and the Environmental Health (EH) had no idea 70% (n = 156).
The study further reveals that higher levels of disagreement from DA students imply that respondents consider their breath, teeth, and gums healthy or more acceptable than the EH group. These findings could potentially be attributed to the structure of the curriculum for both groups. No module covers oral and general health for EH students, whereas for DA students; oral and general health is covered in pharmacology, oral pathology, dental assisting theory and practical. This was verified by a curriculum checklist that was done for both programmes.
Lastly, in this study, we explored whether there is a course that focuses on students' self-care and general health. A study conducted in oral and oral health knowledge and the attitude among nursing students revealed that because oral health was not part of the curriculum, students had no interest or knowledge about oral health.25 This study's findings suggested that both programmes did not feature a module that teaches them about self-care. This was verified through a curriculum checklist. Even though the DA might have a bit of knowledge about oral health in this research, further research and a more thorough review of this learning process must unpack the dynamic realities of understanding health and oral disease systems.16
Despite the impact that oral health has on general health and the quality of life, in most developing countries including South Africa, it is still one of the most neglected aspects of health.9
Clinical relevance
This is the first research study to evaluate oral health awareness and oral health behaviours among students in a University of Technology. The dental clinic in the university will be presented with the results of this study, and this will provide the basis to modify the current teaching module to improve the outcomes and treatment services offered to students.
Noting that there is a shortage of oral health research at the university, this study's results can be a catalyst for more oral health research. Although research recognises that knowledge does not always translate into action, the disparities found in this study may be primarily resolved using community and individual-based oral health education, promotion and prevention strategies and services. These can be integrated into the National Health Insurance planning for university students in South Africa.
Limitations of the study
The study participants were drawn from a single place, and therefore, the results cannot be generalised to other departments. This study, with its limitations, can provide insight into students' oral health care knowledge. Further research about oral health care knowledge still needs to be explored in all the university departments. In our study, the DMFT index could not be performed due to the Covid-19 pandemic.
CONCLUSION
The study aimed at exploring the students' oral health care methods and thereafter make them aware of measures such as the use of fluoridated toothpaste and application of topical fluoride. Curative measures are available, but the achievement of lower dental caries rates in SA could be through community campaigns and oral health programs. Although these are already in place, the coverage needs to be increased and include tertiary institutions. Oral health promotion should be community-based and must also be included in the course designed for University students.
DECLARATIONS
Acknowledgements
The researcher would like to thank the participants who contributed to this study.
Disclaimer
The views expressed in the submitted article are the authors own and not an official position of the institution.
Competing interests
The author(s) declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article.
Ethical consideration and consent to participate
This is contained in the manuscript.
Source of funding/support
The authors received financial support for the research, authorship, and publication of this article from the Department of Higher Education and Training (DHET) via the Research Grant and Scholarship Committee (UCDR R&D) from the University of Technology.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, RM, upon reasonable request.
References
1. Bissett S, Preshaw P. Guide to providing mouth care for older people. Nurs Older People. Dec 2011; 23(10): 14-21. doi: 10.7748/nop2011.12.23.10.14.c8837. PMID: 22256725. [ Links ]
2. Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. J Am Dent Assoc. Dec 2016; 147(12): 915-7. doi: 10.1016/j.adaj.2016.10.001. PMID: 27886668. [ Links ]
3. Blaggana A, Grover V, Anjali, Kapoor A, Blaggana V, Tanwar R, Kaur H, Haneet RK. Oral Health Knowledge, Attitudes and Practice Behaviour among Secondary School Children in Chandigarh. J Clin Diagn Res. Oct 2016; 10(10): ZC01-ZC06. doi: 10.7860/JCDR/2016/23640.8633. Epub 2016 Oct 1. PMID: 27891447; PMCID: PMC5121785. [ Links ]
4. Azodo CC, Ehizele AO, Umoh A, Ojehanon PI, Akhionbare O, Okechukwu R, Igbinosa L. Perceived oral health status and treatment needs of dental auxiliaries. Libyan J Med. 2010 Mar 15;5. doi: 10.3402/ljm.v5i0.4859. PMID: 21483589; PMCID: PMC3071173. [ Links ]
5. Ghaffari M, Rakhshanderou S, Ramezankhani A, Noroozi M, Armoon B. Oral Health Education and Promotion Programmes: Meta-Analysis of 17-Year Intervention. Int J Dent Hyg. 2018 Feb;16(1):59-67. doi: 10.1111/idh.12304. Epub 2017 Aug 24. PMID: 28836347. [ Links ]
6. Formicola AJ. Considering Students' Cost of a Dental Education: Return on Investment and Debt to Income Ratio. J Dent Educ. Aug 2017; 81(8): eS28-eS32. doi: 10.21815/ JDE.017.004. PMID: 28765452. [ Links ]
7. Formicola AJ, Bailit HL. Community-based dental education: history, current status, and future. J Dent Educ. Jan 2012; 76(1): 98-106. PMID: 22262554. [ Links ]
8. Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS, Mullany EC, Abate KH, Abbafati C, Abebe Z, Afarideh M. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 11 May 2019; 393(10184): 1958-72. doi: 10.10 16/S0140-6736(19)30041-8. Epub 2019 Apr 4. PMID: 30954305; PMCID: PMC6899507. [ Links ]
9. Ramphoma KJ. Oral Health in South Africa: Exploring the role of dental public health specialists. SADJ. 2016; 71(9): 402-3. Available from http://www.scielo.org.za/scielo.php?script=sci_arttext&pid=S0011-85162016000900005 (Accessed on 02 Feb. 2021). [ Links ]
10. Murray CJ, Abbafati C, Abbas KM, Abbasi M, Abbasi-Kangevari M, Abd-Allah F, Abdollahi M, Abedi P, Abedi A, Abolhassani H, Aboyans V. Five insights from the global burden of disease study 2019. Lancet (London, England). 2020 Oct; 396(10258): 1135-59. doi: 10.1016/s0140-6736(20)31404-5. [ Links ]
11. Patel RR, Richards PS, Inglehart MR. Periodontal health, quality of life, and smiling patterns - an exploration. J Periodontol. Feb 2008; 79(2): 224-31. doi: 10.1902/jop.2008.070344. PMID:18251637. [ Links ]
12. Sheiham A. Oral health, general health and quality of life. Bull World Health Organ. Sep 2005; 83(9): 644. Epub 2005 Sep 30. PMID: 16211151; PMCID: PMC2626333. [ Links ]
13. Thorpe S. Oral health issues in the African region: Current situation and future perspectives. Journal of Dental Education. 2006; 70(11): 8-15. https://doi.org/10.1002/j.0022-0337.2006.70.11_suppl.tb04209.x. [ Links ]
14. Singh S. Dental caries rates in South Africa: implications for oral health planning. South Afr J Epidemiol Infec. 2011; 26(4): 259-261. https://doi.org/10.1080/10158782.2011.11441463. [ Links ]
15. Modikoe MM, Reid M, Nel R. Oral health-related knowledge, attitudes and practices of adult patients in Mangaung Metropolitan Municipality, South Africa. SADJ. 2019; 74( 4 ): 180-6. https://dx.doi.org/10.17159/2519-0105/2019/v74no4a3. [ Links ]
16. Singh S, Pottapinjara S. Dental undergraduate students' knowledge, attitudes and practices in oral health self-care: A survey from a South African university. AJHPE. 2017; 9(2): 83-7. https://doi.org/10.7196/AJHPE.2017.v9i2.800. [ Links ]
17. Cochran, WG. Sampling techniques. 2007. John Wiley & Sons. ISBN 471-16240-X. Available from https://hwbdocuments.env.nm.gov/Los%20Alamos%20National%20Labs/General/14447.pdf (Accessed on 02 February 2021). [ Links ]
18. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative research in psychology. 2006; 3(2): 77-101. http://doi.org/10.1191/1478088706qp063oa. [ Links ]
19. Park SE, Timothé P, Nalliah R, Karimbux NY, Howell TH. A case completion curriculum for clinical dental education: replacing numerical requirements with patient-based comprehensive care. J Dent Educ. Nov 2011; 75(11): 1411-6. PMID: 22058389. [ Links ]
20. Thema LK, Singh S. Integrated primary oral health services in South Africa: the role of the PHC nurse in providing oral health examination and education: open forum. Afr J Prim Health Care Fam Med. 2013; 5(1): 1-4. https://doi.org/10.4102/phcfm.v5i1.413. [ Links ]
21. Peltzer K, Pengpid S. Oral health behaviour and social and health factors in university students from 26 low, middle and high income countries. Int J Environ Res Public Health. 26 Nov 2014; 11(12): 12247-60. doi: 10.3390/ijerph111212247. PMID: 25431876; PMCID: PMC4276612. [ Links ]
22. Sarpkaya R, Çavus B, Yilmaz K. The Involvement of Adults in Formal Education and Lifelong Learning Activities According to OECD Data: An Evaluation in the Light of OECD Education at a Glance 2017. International Journal of Psycho-Educational Sciences. 2018; 7(2): 16-29. Available from https://flles.eric.ed.gov/fulltext/EJ1252963.pdf (Accessed on 02 February 2021). [ Links ]
23. Al-Hussaini R, Al-Kandari M, Hamadi T, Al-Mutawa A, Honkala S, Memon A. Dental health knowledge, attitudes and behaviour among students at the Kuwait University Health Sciences Centre. Med Princ Pract. Oct-Dec 2003; 12(4): 260-5. doi: 10.1159/000072295. PMID: 12966201. [ Links ]
24. Graça SR, Albuquerque TS, Luis HS, Assunção VA, Malmqvist S, Cuculescu M, Slusanschi O, Johannsen G, Galuscan A, Podariu AC, Johannsen A. Oral Health Knowledge, Perceptions, and Habits of Adolescents from Portugal, Romania, and Sweden: A Comparative Study. J Int Soc Prev Community Dent. 30 Sep 2019; 9(5): 470-80. doi: 10.4103/jispcd.JISP-CD_194_19. PMID: 31620380; PMCID: PMC6792312. [ Links ]
25. Smadi L, Nassar OS. Oral & dental health knowledge and attitude among nursing students. WJER. 2016; 3(2): 238-50. https://doi.org/10.22158/wjer.v3n2p238. [ Links ]
26. Taniguchi-Tabata A, Ekuni D, Mizutani S, Yamane-Takeuchi M, Kataoka K, Azuma T, Tomofuji T, Iwasaki Y, Morita M. Associations between dental knowledge, source of dental knowledge and oral health behavior in Japanese university stu-dents: A cross-sectional study. PLoS One. 8 Jun 2017; 12(6): e0179298. doi: 10.1371/journal.pone.0179298. PMID: 28594914; PMCID: PMC5464648. [ Links ]
27. Silva JVD, Oliveira AGRDC. Individual and contextual factors associated to the self-perception of oral health in Brazilian adults. Rev Saude Publica. 2018 Apr 9;52:29. doi: 10.11606/ S1518-8787.2018052000361. PMID: 29641654; PMCID: PMC 5893273. [ Links ]
 Correspondence:
Correspondence:
Rajeshree Moodley
Email: moodleyra@ukzn.ac.za
Author contributions:
1 . Feziwe Flora Mbele-Kokela: Study conception and design, data collection, data analysis, data interpretation and drafting of the manuscript - 50%
2 . Rajeshree Moodley: Supervision of the entire work, study design and manuscript review - 50%
All authors critically revised the article for valuable intellectual content and approved the final version to be published.