Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.75 n.7 Johannesburg Aug. 2020
http://dx.doi.org/10.17159/2519-0105/2020/v75no7a3
RESEARCH
The effect of A-dec ICXTM on microbiological water quality in self-contained dental units' water systems
SP KgabiI; SR MthethwaII
IBSc, BSc (Hons) MSc (Dent)., Sefako Makgatho Health Sciences University, Pretoria, South Africa. ORCID Number: 0000-0003-0416-1808
IIBDS, MPH, PhD., Sefako Makgatho Health Sciences University, Pretoria, South Africa. ORCID Number: 0000-0003-0420-808X
INTRODUCTION AND BACKGROUND
The contamination of dental unit waterlines (DUWLs) as a result of biofilms that adhere to the inner surfaces of the lines continues to generate concern. The biofilm serves as a reservoir that can increase the number of free-floating microorganisms in the water used for dental treatment.
Recent studies found that it presents a confirmed but limited risk to immunocompetent individuals, but may pose a significant hazard for immunocompromised patients and dental professionals.2-5 DUWLs are prone to biofilm formation because of their small diameter and water stagnation. Untreated or unfiltered dental unit water is likely to contain high numbers of microorganisms and is unlikely to meet standards for water used as a cool-ant/irrigant for nonsurgical dental procedures.6
Common approaches to improve water quality include self-contained water systems combined with periodic or continuous chemical treatment protocols, daily draining, air purging regimens, anti-retraction valves, point of use micro-filters, as well as flushing waterlines for several minutes in the morning and after every patient.7,8
Centralized systems designed for single chair or entire practice waterlines that purify or treat incoming water to remove or inactivate microorganisms are becoming more popular.9
In most dental settings, treatment water comes from the municipal water supply directly into the dental unit.
Self-contained water systems, by contrast, isolate the dental unit from the municipal water supply. A bottle system affixed to the dental unit, in self-contained water systems, allow the clinician to better control the quality of water used in the dental treatment.10 They also provide a way to introduce biofilm or microorganism-attacking chemicals into waterlines.
Without use of a chemical agent, however, self-contained systems do not reliably improve water quality.11 Improperly maintained, a contaminated bottle system can worsen the microbiological quality of dental unit water.10,11
The disinfectant properties of the effervescent tablets of A-dec ICXTM have been assessed.12-15 Their effectiveness in DUWL treatment protocol has been demonstrated in studies performed in simulated patient care settings as well as at dental treatment clinics. McDowell and colleagues (2004) found that A-dec ICXTM prevented biofilm formation in dental unit water-lines, reduced bacterial counts in incoming water and produced water quality exceeding stated recommendations of the American Dental Association (ADA) in a simulated clinical use study over a 16-week period.12 Meiller and colleagues produced results which were consistent with those of McDowell over a 4-week period.14 Independent studies at military hospitals in the USA and Malaysia by Bowen and colleagues (2015) and Siang Ma and colleagues (2015) respectively found that A-dec ICXTM reduced the bacterial load over a 5-week and 24-week periods respectively.13,15
At the oral health centre of Sefako Makgatho Health Sciences University (SMU), a dental school and a comprehensive care referral hospital in the outskirts of Pretoria, water flowing in dental units is mainly obtained from the municipal water supply. In early 2017, less than 10% (17/228) of the dental units had a self-contained water system that was separate from the municipal water.
No waterline treatment devices or chemical treatment protocols were being implemented. This study investigates the consistency of the reported association between the disinfection properties of the effervescent tablets of A-dec ICXTM and reduced bacterial counts in dental unit water at the oral health centre of SMU.
OBJECTIVES OF THE STUDY
To measure and compare mean bacterial counts in water samples collected from dental chairs which received pure distilled water only and those which received A-dec ICXTM tablet dissolved in distilled water.
MATERIALS AND METHODS
Design
This was a pre-test/post-test control group experimental design.
Target population
The study population consisted of seventeen dental units fitted with independent water system and used routinely to treat patients for 8 years with distilled water in clinics at the dental school of the Sefako Makgatho Health Sciences University in early 2017.
Sample size
Fourteen dental units were eligible to participate in the study. Three units that were not being used regularly for patient care were excluded from the study.
Allocation method
A sequence of random numbers was generated by a statistician using the computer software program SPSS (IBM, 2018).
The allocation sequence was concealed in a desktop computer until treatments were assigned by the supervisor. The random allocation rule was implemented i.e. a subset of the total sample size was randomly assigned by the research supervisor to group A (units which received distilled water only) and the remainder were assigned to group B (units which received A-dec ICXTM dissolved in distilled water).16
Blinding
Throughout the study period, the supervisor refilled two sterile twenty-five litres bottles labelled A and B with two levels of the treatment. The bottle labelled A contained pure distilled water. The distilled water in the bottle labelled B was prepared into a solution by dissolving one A-dec ICX™ tablet in 0.7 litre of pure distilled water.
The researcher (first author) monitored the water level in the dental units between clinic sessions and reported to the supervisor (second author) who replenished the supply of the allocated treatments daily. The researcher was blinded to group assignment of the units. All the dental units were observed throughout the study period to make sure there was no breakdown reported. The practice of flushing waterlines was not monitored.
Treatments
Seven dental units continued receiving pure distilled water while the remainder received A-dec ICXTM tablet dissolved in distilled water.
The primary outcome measured at the end of the Ave week follow up was the mean bacterial cfu/ml in water samples. The effect of interest was the difference in mean bacterial colony-forming units per millilitre (cfu/ ml) between water samples collected from dental units which received two levels of the treatment. Repeat measurements of bacterial cfu/ml in water samples were performed for 20% of the samples.
Hypothesis
A-dec ICXTM reduces bacterial counts in dental unit waterlines.
Data collection
Water samples were collected from the dental chairs at baseline, the end of week 1 and at the end of week five. All samples reached the laboratory within 3 hours of collection and were processed appropriately upon arrival.
Water samples
100 ml water samples for aerobic cultures were collected from the distal outlets of the three-way air and water syringes into sterile bottles containing 0.1g of sodium thiosulfate to remove any residual disinfectant, after a 2 minute purge at the beginning of the workday before the dental unit was used.
Three, ten-fold serial dilutions (1:10, 1:100, and 1:1000) were prepared by adding 1 ml of each sample to 9 ml of sterile tap water in new sterile universal bottles.
Aliquots of 0.01 ml of each dilution was distributed evenly over the surface of sterile R2A agar plates using a sterile bent-glass rod (spread plate technique) and subsequently incubated at 28 °C for 96 hours.
Ethical considerations
The study protocol was approved by the Ethics Committee of Sefako Makgatho University (SMUREC/D/298 /2016: PG). Permission to conduct the study was granted by the CEO of Medunsa Oral Health Centre.
STATISTICAL ANALYSIS/ HYPOTHESIS TESTING
Collected data were subjected to univariate analysis in} Statistical Package for the Social Sciences (SPSS) software. Measures of central tendency and dispersion were calculated.
ANCOVA was performed to evaluate whether the means of the dependent variable i.e. post-test (follow-up) mean bacterial cfu/ml measurement were equal across levels of a categorical independent variable i.e. the treatment group (pure distilled water = control, A-dec ICXTM tablet dissolved in pure distilled water = treatment), while statistically controlling for the effects of the covariate i.e. pretest (baseline) mean bacterial cfu/ml. The level of significance was originally set at 0.05. Bonferroni correction was performed to counteract the problem of multiple comparisons.
A Bonferroni corrected/adjusted p value of 0.0083 was obtained by dividing the original α-value (0.05) by the number of analyses (6) on the dependent variable.17
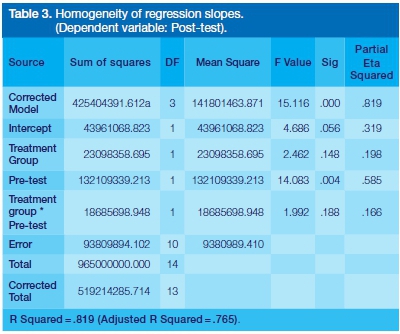
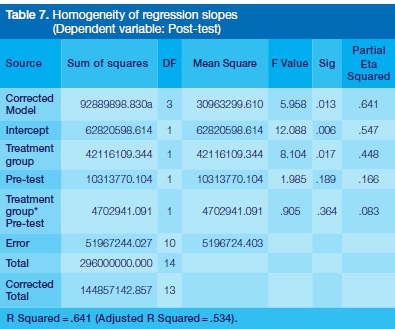
Regression diagnostics was performed to evaluate the appropriateness of ANCOVA model. Two assumptions were checked to make sure that the covariate meets the requirements to run the ANCOVA.
These were: (1) independence of the covariate and treatment effect and (2) homogeneity of regression slopes. Interim analysis was performed at the end of week one.
RESULTS
Bacterial counts recorded from water samples collected from fourteen dental units were analysed. Figure 1 below is a flow diagram of the progress through the phases of the study (that is, enrolment, treatment allocation, follow-up, and data analysis).
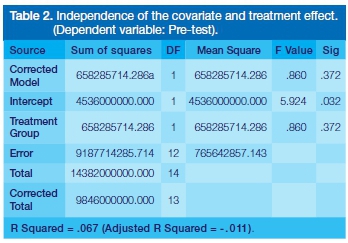
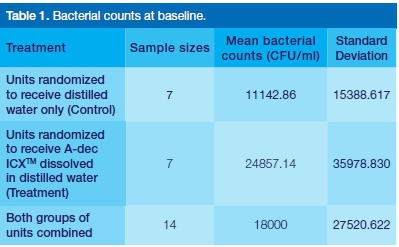
The huge discrepancy in mean bacterial counts (24857.14 vs. 11142.86) indicate that the bacterial counts at baseline were not evenly distributed in the treatment groups. The mean bacterial count of the units was 18000cfu/ml.
There was insufficient evidence (p (0.860) >0.0083) to reject the null hypothesis that the covariate (pre-test) was not different across the levels of the independent variable (treatment group) in the analysis.
The interaction effect between the covariate (pre-test) and independent variable (treatment group) in a model that includes the interaction between the covariate and independent variable was not significant (p (0.188) > 0.0083). This means that the regression slopes for the independent variable (treatment group) and covariate (pre-test) are similar.
There was insufficient evidence (p(0.391)> 0.0083) to reject the null hypothesis that the post-test mean bacterial cfu/ml were equal across levels of the treatment group when controlling for the covariate (pre-test).
At the end of week 1, the difference in mean bacterial cfu/ml between the control group and the treatment group was not statistically significant (p (0.391) > 0.0083 in Table 6 above) when controlling for the covariate (pre-test).


ANALYSIS AT THE END OF WEEK 5
There was insufficient evidence (p(0.860)>0.0083) to reject the null hypothesis that the covariate (pre-test) was not different across the levels of the independent variable (treatment group) in the analysis.
The interaction effect between the covariate (pre-test) and independent variable (group) in a model that includes the interaction between the covariate and independent variable was not significant (p (0.364)>0.0083). This means that the regression slopes for the independent variable (treatment group) and covariate (pre-test) are similar.
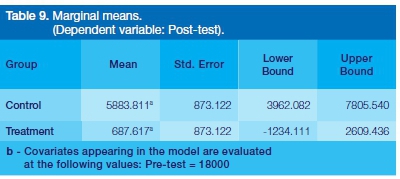
There was a statistically significant difference (p (0.002) < 0.0083.) in the post-test mean bacterial cfu/ml across levels of the treatment group when controlling for the covariate (pre-test).
At the end of week 5, a statistically significant (p (0.002) <0.0083 in Table 8 above.) drop in mean bacterial cfu/ ml from 5883.811 in the control group to 687.617 in the treatment group was estimated when controlling for the covariate (pre-test).


The 95% confidence interval of the difference in mean bacterial counts between the groups ranged from 2470.336 to 7243.964 cfu/ml. This confidence interval did not include zero, confirming the finding that the difference was statistically significant (p(002)< 0.0083).
DISCUSSION
This study was designed to determine the effect of A-dec ICXTM on bacterial counts in dental unit water. The results indicate that the baseline mean bacterial count was 18000 cfu/ml (SD 27520.622 cfu/ml) (Table 1). This bacterial count far exceeded the Centers for Disease Control and Prevention (CDC) and European Union's standard for water quality used in non-surgical dental procedures.
The results were however consistent with those of other studies which assessed bacterial counts in dental units which used distilled water alone. Marais and Brozel (1999) reported bacterial counts ranging from 3x104-2x105 cfu/ml from chairs at the University of Pretoria's Department of Oral Medicine and Periodontology, that had been in use for twelve years.18
Schmidtke found bacterial counts approximating 240000 cfu/ml in twelve chairs in the orthodontic clinic at the Department of Orthodontics, University of Alabama at Birmingham School of Dentistry, Birmingham, Alabama.19 The findings of the current and cited previous studies was not unexpected. Kettering and Stephens (2002) demonstrated that distilled water alone cannot reduce microbial contamination of dental treatment water to the 200cfu/ml ADA stated goal.20 The Organization for Safety, Asepsis and Prevention (OSAP) recommends using distilled water combined with periods of continuous application of chemicals.10,11
The results of this study showed a huge discrepancy in mean bacterial counts at baseline between the treatment groups (Table 1 ). This was not unexpected. The small sample size accounted for the large chance difference observed following randomization.21
The results of the regression diagnostics showed that the data satisfied the underlying assumptions inherent in the ANCOVA model (Tables 2, 3, 6 and 7). They confirmed that the ANCOVA model was the appropriate analysis for this study - consequently, the validity of the conclusions drawn could be relied upon.
The results of the interim analysis study showed that the mean bacterial counts in both group of units decreased, more so for the group of units which received A-dec ICXTM dissolved in distilled water (Table 5). The decrease was however not statistically significant (Tables 4).
This result may be explained by the fact that the mean difference in bacterial counts between the groups at baseline was huge relative to that measured at week one. These findings suggest that A-dec ICX™ tablets improved water quality. They support the OSAP recommendation that distilled water should be combined with periods of continuous application of chemicals.10,11
This experiment found substantial evidence (p(0.002)< 0.0083.) to reject the null hypothesis that the post-test mean bacterial cfu/ml were equal across levels of the treatment group when controlling for the covariate (pretest) i.e. the difference in mean bacterial cfu/ml between units which received A-dec ICXTM dissolved in distilled water and those which received distilled water only was statistically significant (Tables 8 and 9).
This study produced results which corroborate the findings of a great deal of the previous research in different settings.12-15 There are several possible explanations for the failure of treated distilled water to reduce bacterial counts to levels recommended by the ADA and CDC.
These include among others, the contamination of water sample by detachment of biofilm from the inner surface of the dental tubing, the extremely high bacterial count prevalent at baseline and the relatively short study period of Ave weeks.
The current study found that the 95% confidence interval of the difference in mean bacterial counts between the groups ranged from 2470.336 to 7243.964 cfu/ml (Table 10). The upper and lower limits of the confidence interval indicate that the true difference was large and practically significant.
The wide confidence interval however indicates that the estimate of the mean difference was not precise. A wide confidence interval results from a small sample and/ or data with substantial variability, and is a suggestion of low power.22
Limitations of the study
The flushing of the waterlines in the morning, at the end of the day, and between patients was not monitored. This was a source of potential imprecision in the measurement of the effect of interest.
Waterline flushing has been reported to improve water quality.23-25 Cobb and colleagues (2002) found evidence that time-dependent waterline flushing produced a statistically significant reduction in planktonic bacteria.26
The failure to monitor waterline flushing in this study could not have distorted the estimate of the reduction in bacterial counts between water samples collected from dental units which received A-dec ICXTM dissolved in distilled water and those which received distilled water only as the users of the dental units were blinded to group assignment of the units.
CONCLUSION
A-dec ICXTM reduced bacterial counts in dental unit waterlines.
References
1. Lauritano D, Nardone M, Gaudio RM, Candotto V, Carinci F. Risk assessment of colonization of legionella spp. in dental unit waterlines. Oral Implantol. - Rome. 2017; 10(3): 283-8. [ Links ]
2. Mills SE. The dental unit waterline controversy: defusing the myths, defining the solutions. J Am Dent Assoc. 2000; 131(10): 1427-41. [ Links ]
3. Ricci ML, Fontana S, Pinci F, et al. Pneumonia associated with a dental unit waterline. Lancet. 2012; 379(9816): 684. [ Links ]
4. Barbot V, Robert A, Rodier MH, Imbert C. Update on infectious risks associated with dental unit waterlines. FEMS Immunol Med Microbiol. 2012; 65(2): 196-204. [ Links ]
5. Weissfeld, A.S. Infection Control in the Dental Office. Clin Microbiol Newsletter. 2014; 36(11): 79-84. [ Links ]
6. Organization for Safety, Asepsis and Prevention. Dental Unit Water Quality: OSAP White Paper and Recommendations. 2018; Available:https://cdn.ymaws.com/www.osap.org/resou-rce/resmgr/annual_conf_2018/handouts/osap.duwl.whitepa-peredits.mi.pdf Accessed [05 March 2019]. [ Links ]
7. Centers for Disease Control and Prevention. Infection Prevention & Control in Dental Settings. 2019; Available at: http://www.cdc.gov/OralHealth/infectioncontrol/index.html Accessed [05 March 2019]. [ Links ]
8. Szymanska J. Control methods of the microbial water quality in dental unit waterlines. Ann Agric Environ Med. 2003; 10(1): 1-4. [ Links ]
9. USAF Dental Evaluation & Consultation Service. Synopsis of Dental Unit Waterline Treatment Products and Devices. (Project 09-07) (9/09). Available: https://www.crosstex.com/sites/de-fault/files/public/usaf-study.pdf. Accessed [05 March 2019]. [ Links ]
10. Organization for Safety, Asepsis and Prevention. Biofilm and Dental Unit Waterlines. 2003 CDC guidelines expand dental worker responsibilities for treatment water quality. Infection Control in Practice. 2004; 3(2): 1-5. [ Links ]
11. Organization for Safety, Asepsis and Prevention. Dental Unit Waterlines: Questions and Answers. Available: https://www.osap.org/page/Issues_DUWL_1. Accessed [05 March 2019]. [ Links ]
12. McDowell JW, Paulson DS, Mitchell JA. A simulated-use evaluation of a strategy for preventing biofilm formation in dental unit waterlines. J Am Dent Assoc 2004; 135(6): 799-805. [ Links ]
13. Bowen CG, Greenwood W, Guevara P, Washington MA. Effectiveness of a dental unit waterline treatment protocol with A-Dec ICX and Citrisil disinfectants. Military Medicine 2015; 180(10): 1098-1104. [ Links ]
14. Meiller TF, Kelley JI, Zhang M, DePaola LG. Efficacy of A-dec's ICX dental unit waterline treatment solution in the prevention and treatment of microbial contamination in dental units. J Clin Dent. 2004; 15(1): 17-21. [ Links ]
15. Siang MM, Zalini Y, Ahmad R, Zukri A, Farizah AF. A comparison of different disinfectants on the microbiological quality of water from the dental unit waterlines of a military hospital. Sains Malaysiana. 2015; 44(2): 187-92 [ Links ]
16. Schulz KF, Grimes DA. Generation of allocation sequences in randomised trials: chance, not choice. The Lancet. 2002; 359: 515-9. [ Links ]
17. Chen SY, Feng Z, Yi X. A general introduction to adjustment for multiple comparisons. J Thorac Dis. 2017; 9(6): 1725-9. [ Links ]
18. Marais J.T, Brozel, V.S. Electro-chemically activated water in dental unit water lines. Br Dent J. 1999; 187: 154-8. [ Links ]
19. Schmidtke DW. Efficacy of Sterisil in the treatment of dental unit waterlines [Thesis]. University of Alabama at Birmingham. 2011; Available: https://static1.squarespace.com/static/5528a5d7e4b0f89b5fecbc38/t/58ab73cd3a0411800f24 1112/1487631310570/Alabama+Student+Study+Pure tube+and+bottle.pdf. Accessed [05 March 2019]. [ Links ]
20. Kettering JD, Munoz-Viveros CA, Stephens JA, Naylor WP, Zang W. Reducing bacterial counts in dental unit waterlines: distilled water vs antimicrobial agents. J Calif Dent Assoc 2002; 30: 735-41 [ Links ]
21. Petrie A, Sabin C. Clinical trials. Medical statistics at a glance. 2nd ed. Massachusetts: Blackwell Publishing, 2005; 34-6. [ Links ]
22. Petrie A, Sabin C. Errors in hypothesis testing. Medical statistics at a glance. 2nd ed. Massachusetts: Blackwell Publishing, 2005: 44-5. [ Links ]
23. Pankhurst CL, Johnson NW, Woods RG. Microbial contamination of dental unit waterlines: the scientific argument. Int Dent J. 1998; 48: 359-68. [ Links ]
24. Venkatesh VK, Vidyashree NV, Parameswaran VA, et al. 2006. Evaluation of bacterial contamination of dental unit water Lines and the efficacy of a commercially available disinfectant. J Conserv Dent. 2006; 9: 93-8. [ Links ]
25. Watanabe E, Agostinho AM, Matsumoto W, et al. Dental unit water: bacterial decontamination of old and new dental units by flushing water. Int J Dent Hyg. 2008; 6(1): 56-62. [ Links ]
26. Cobb CM, Martel CR, McKnight SA 3rd, Pasley-Mowry C, Ferguson BL, Williams K: How does time-dependent dental unit waterlines flushing affect planktonic bacteria levels? J Dent Educ. 2002; 66: 549-55. [ Links ]
 Correspondence:
Correspondence:
Sibusiso R Mthethwa
Medunsa Campus, PO Box D24
Sefako Makgatho Health Sciences University, 0204
Pretoria, South Africa.
Email: rocky.mthethwa@smu.ac.za
Author contributions:
1 . Shamaka P Kgabi: Conception; revising the article critically for important intellectual content - 50%
2 . Sibusiso R Mthethwa: Project supervision; analysis and interpretation of data; drafting the article - 50%














