Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.75 n.5 Johannesburg Jun. 2020
http://dx.doi.org/10.17159/2519-0105/2020/v75no5a8
ETHICS
Fraudulent records - Grave forensic consequences
LM SykesI; L RobinsonII; H BernitzIII
IBSc, BDS, MDent, Dip Research Ethics (IRENSA); Dip ESMEA (Univ Dundee), DipOdont (Forensic Odontology), Department of Prosthodontics, School of Dentistry, Faculty of Health Sciences, University of Pretoria, Pretoria, South Africa. ORCID Number: 0000-0002-2002-6238
IIBChD, PDD (Maxillofacial Radiology), PDD (Forensic Odontology), Department of Oral Pathology and Oral Biology, School of Dentistry, Faculty of Health Sciences, University of Pretoria, Pretoria, South Africa. ORCID Number: 0000-0002-0549-7824
IIIBChD, Dip (Odont), MSc, PhD, Department of Oral Pathology and Oral Biology, School of Dentistry, Faculty of Health Sciences, University of Pretoria, Pretoria, South Africa. ORCID Number: 0000-0003-1361-1225
INTRODUCTION
Natural disasters, fatal accidents, and violent criminal offences are part of everyday life. All of these may result in fatalities that shatter the lives of the victim's families and friends. Their trauma is compounded by the fact that all unnatural deaths have to be investigated, and the bodies of the deceased positively identified before they can be released to the families for burial.
Bodies of victims of violent crimes, fires, drowning, motor vehicle or aviation accidents, work place fatalities or situations where some time has elapsed since death may be so disfigured that "identification by a family member is neither possible or desirable".1
Often the nature or degree of the injury may be so extensive that fingerprinting is also not a viable option. DNA analysis may be considered, however it takes time and is a costly procedure. There are also concerns with maintaining strict control over the chain of evidence during all additional procedures and tests. Thus, in these situations the forensic odontologist may be called in as part of the investigative team.
LITERATURE REVIEW
Dental forensics
Victim identification using forensic odontology may take one of two forms. The more common is where the forensic odontologist performs a comparative examination of ante-mortem records with a post-mortem examination.
The other is when there are no ante-mortem records available. Here dental profiling may help investigators narrow down the search to persons of a specific age, gender, and racial group. The most common reasons for dental identification are the following:
1. In criminal cases - the investigation cannot begin until the victim has been positively identified.
2. Marriage - where a remaining spouse cannot remarry until their partner has been confirmed to be deceased.
3. Monetary - where the payment of pension, life insurance or other benefits will only happen after confirmation of death.
4. Burial - the body may not be released to the family for burial until it has been positively identified (except in cases of a pauper's burial).
5. Social - to preserve the dignity of a deceased person their identity should be known.
6. Closure - for families whose loved ones have been missing for an extended time - a positive identification will provide them with final confirmation and closure.1,2
A delay in identification will thus have an impact on most, if not all of the above activities, and may cause untold anguish and distress to the remaining family members and loved ones.
Comparative dental identification involves comparison of ante-mortem dental records (including patient files, written notes, radiographs, photographs and study models), with findings obtained from a thorough postmortem clinical assessment (including visual appraisal, dental charting and radiographs). Persons with numerous and complex dental restorations, or distinctly characteristic tooth morphology will be much easier to identify than individuals with little or no restorative work or unique features. The process involves a "methodical and systematic comparison of each tooth and the surrounding structures in turn".1
A detailed description of this process is beyond the scope of this paper. In brief, the examination includes noting teeth present and missing, their type and position, morphology and pathology of the teeth crowns, roots, pulp chambers, and periapical regions, and all dental restorations. In addition, the examination may involve the assessment of gingival/periodontal morphology and pathology, as well as surrounding osseous features including the alveolar process and lamina dura, maxillary sinuses, anterior nasal spine, mandibular canal, coronoid and condylar processes, and any other pathological entities.1
After the comparison, one of four conclusions may be reached:
1. Positive identification - where records match with sufficient details and no unexplainable discrepancies.
2. Possible identification - where there are many consistent features, but the nature or quality of the records are not good enough to justify a statement of absolute certainly.
3. Insufficient evidence available to draw any conclusions.
4. Exclusion - if there are clear inconsistencies in ante-mortem and post-mortem data.3
(Note: Larger/more complex or additional restorations in the post-mortem findings may be explained by disease progression, and can still result in a positive identification. However, smaller or fewer restorations are unexplainable and would warrant exclusion).
Many studies have investigated the minimum number of concordant features needed to make a positive identification. However, there is no universally accepted number required, because each case has its own individuality and as such, the final decision needs to lie with the experience, expertise, and judgement of the forensic odontologist.4
Dental fraud
The healthcare industry is unique in that it is both "service and product based". Vast amounts of money is spent, with many different role-players all vying for their share of the market in order to secure personal gains. Inevitably, "some will try to take advantage of the system and manipulate it to their benefit".5
Postma et al. (2011) conducted a study of misconduct complaints against oral health care professionals lodged with the HPCSA from 2004-2009. The results revealed that fraud accounted for 29% and 46% of the cases against dentists and dental therapists respectively.6 The range of fraudulent complaints related to over-servicing, overcharging, claiming for services rendered to non-members, changing service dates, discrepancies between clinical records and billing records, submitting claims while being suspended from practice, incorrect tariff codes, claiming for procedures not performed, and split billing.6
In a later study of HPCSA misconduct records, Nortjé and Hoffmann (2014) also found that the predominant transgression was charging for services not performed and submitting these claims to medical aids, as well as for performing sub-optimal treatment.7
These studies only investigated HPCSA records and did not give any indication of the magnitude/scale of the fraud. Putter and Naidoo (2018) conducted an investigation that looked specifically at dental fraud, using data obtained from HPCSA, Discovery, and the Board of Health Care Funders (BHF) records. Discovery revealed that between 2007 and 2015, dental fraud reached a total of over ZAR 18.1 million. Statistics from the BHF were even more alarming as they estimated that in the same nine-year period the amount exceeded ZAR 40 million. In a separate survey conducted by KPMG from 2007-2009, they reported fraudulent cases in excess of ZAR 221 million, where more than 70% consisted of charging for services not rendered or code manipulation.5
Not only does fraud waste money that could be allocated to proper treatment in deserving patients, but also may have other far-reaching consequences, particularly in legal and forensic fields. The following two cases illustrate the severity and potential adverse repercussions of recording procedures not done, or charging for larger/more complex restorations than were actually carried out.
Dental forensics meets Dental fraud - "Discovering the truth after death"
In the entrance of the Pretoria medico-legal mortuary one is met with a sign which reads "This is where the dead teach the living". It often happens that in the very same mortuary the "The dead reveal secrets about the living". Unfortunately it is here, during the dental examination of deceased victims, that unethical dentistry is often discovered. This includes both poor technical procedures as well as blatent unethical practices.
Case 1
Following an aircraft accident the forensic odontology unit at the University of Pretoria were asked to identify the remains of two severely burned bodies. On arrival they were met by the pilot's wife. She was requested to locate the dental records of her deceased husband for a possible dental identification.
Fortunately, she had with her an appointment card from their regular dentist as her husband was busy undergoing dental treatment and had several follow-up sessions scheduled. The card indicated that he still required three more one-hour sessions. On dental examination of the first victim (the assumed pilot), including radiographic assessment, no carious lesions or any other dental pathology could be found. Thus, there was no evidence to justify three further dental appointments.
In light of this information, the forensic odontologist also viewed the three recently completed composite restorations (Teeth 14, 15 and 16) with suspicion (Figure 1). A sound amalgam restoration was noted on tooth 17.
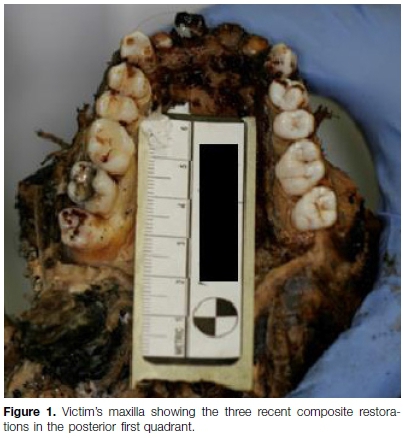
The treating dentist was phoned to discuss the case, but no further action was taken as there was no concrete evidence to substantiate the fact that he intended to carry out more restorative work on "virgin/healthy" teeth (For full details of this case: Forensic dentistry case book 4: Non-maleficence in dental practice, "primum non nocere" by H Bernitz in SADJ August 20158).
Case 2
In a recent mission to identify the victims of a mass disaster, one of the bodies, which had been severly carbonised, was examined for a possible dental identification. During the examination two restorations were noted, these being occlusal amalgams on teeth 18 and 48 (Figure 2). However, when the ante-mortem records arrived, they indicated that an occlusal composite restoration had also been placed on tooth 36, which was not visible during the post-mortem examination.
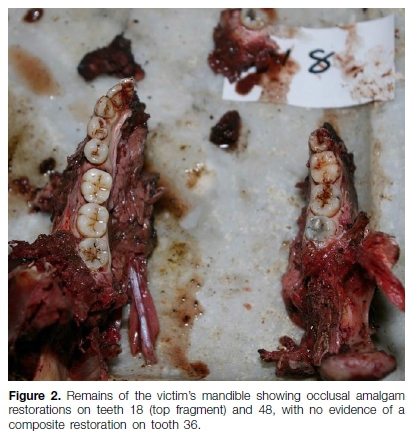
Under microscopic examination, a thin film of sealant was seen, which certainly did not account for the class I composite restoration that the ante-mortem records indicated and for which the patient had been charged.
These findings presented the forensic odontology unit with an unexplainable discrepancy. Faced with this scenario, the unit had to decide what conclusion to draw on the victim's identity. The first option, and the only truly accurate and defensible argument, was that the postmortem dental examination did not match the ante-mortem dental records, and thus positive identification was excluded. The second option was to presume that the dentist had placed the miniscule sealant and fraudulently charged for a larger restoration, and then con-Arm a positive identification. However, with no concrete proof of this fraud,the forensic odontology unit were forced to report exclusion of identity. This meant that the body could not be released to the family for burial until further tests/DNA analysis had been carried out. The victim was subsequently confirmed to be their family member, however the incident forced the family to endure a costly and stressful delay in closure due to the fraudulent activities of their "trusted" dentist.
DISCUSSION AND CONCLUSIONS
Fraud may be defined as "wrongful deception, misrepresentation or concealment with the clear intention to deceive, resulting in personal or financial gain, or as intentional theft".9 However, the extent and repercussions can extend far beyond that of personal gratification, and may have a negative impact on many other innocent persons.
This has been illustrated in the above case scenarios where not only have the victims fallen prey to unscrupulous dentists, but their families have also been forced to endure the extended uncertainly regarding confirmation of their loved ones deaths. The difficulty of dealing with suspected fraud lies in proving intent, and there will always be those who get away with this heinous practice.
The onus lies with the remaining majority of honest practitioners to continue in their pursuits of developing a "strong anti-fraud culture, and improving the character of the nation and reputation of the profession".5
References
1. Pretty IA., Sweet D. A look at forensic dentistry - Part I: The role of teeth in the determination of human identity. Br Dent J. 2001; 190(7): 359-66. [ Links ]
2. Gosavi S, Gosavi S. Forensic odontology: A prosthodontic view. J Forensic Dent Sci. 2012; 4(1): 38-41. [ Links ]
3. Singal K. Dentistry as a tool for identification. J Forensic Science and Criminology. 2015; 2(5): 1043. [ Links ]
4. Acharya AB. Are a minimum number of concordant matches needed to establish identity in forensic odontology? J of Forensic odonto-stomatology. 2003; 21(1): 6-13 [ Links ]
5. Putter S, Naidoo S. Dental fraud in South Africa 2007-2015. SADJ. 2018; 73(9): 546-53. [ Links ]
6. Postma TC, van Wyk PJ, Heymans JH, White JG, Prinsloo PM. An analysis of complaints againt oral health professionals charged with misconduct at the HPCSA: 2004-2009. SADJ. 2011; 66(9):420-5. [ Links ]
7. Nortjé N, Hoffmann, WA. Professional consequence for dentists involved in unethical decision-making in South Africa. J Forensic Odontostomatol. 2014; 32; 22-9. [ Links ]
8. Bernitz H. Forensic dentistry case book 4: Non-maleficence in dental practice, "primum non nocere". SADJ. 2015; 70(7): 312. [ Links ]
9. The Concise Oxford Dictionary. 10th ed. Oxford. Oxford University Press. 1999; 562. [ Links ]
 Correspondence:
Correspondence:
Leanne M Sykes
Department of Prosthodontics, School of Dentistry, Faculty of Health Sciences
University of Pretoria, South Africa
Email: leanne.sykes@up.ac.za
Author contributions:
1 . Leanne M Sykes: Primary author - 40%
2 . Liam Robinson: Secondary author - 30%
3 . Herman Bernitz: Tertiary author - 30%














