Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.73 n.5 Johannesburg Jun. 2018
http://dx.doi.org/10.17159/2519-0105/2018/v73no5a7
RESEARCH
Etiological factors for dentine hypersensitivity in a Nigerian population
PI IdonI; TA EsanII; CT BamiseIII
IConsultant Restorative Dentist, Department of Dental Surgery, University of Maiduguri Teaching Hospital, Maiduguri, Borno State, Nigeria
IIBChD, FMCDS. Associate Professor, Department of Restorative Dentistry, Obafemi Awolowo University, Ile Ife, Osun State, Nigeria
IIIBChD, FMCDS. Associate Professor, Department of Restorative Dentistry, Obafemi Awolowo University, Ile Ife, Osun State, Nigeria
ABSTRACT
INTRODUCTION: There are various etiological and predisposing factors for dentine hypersensitivity (DH). Management of the problem requires modification of these factors for successful and long-lasting resolution. There will be value in identifying these factors.
AIM: To identify the predisposing and etiological factors for DH in a population of patients at a teaching hospital.
DESIGN: A cross sectional descriptive study involving adult patients diagnosed with DH.
MATERIALS AND METHODS: Patients that presented with symptoms suggestive of DH over a period of twelve months were screened to confirm the diagnosis. Presence and frequency of predisposing factors as well as clinical findings of tooth wear lesions, gingival recession and fluorosis were documented on a questionnaire.
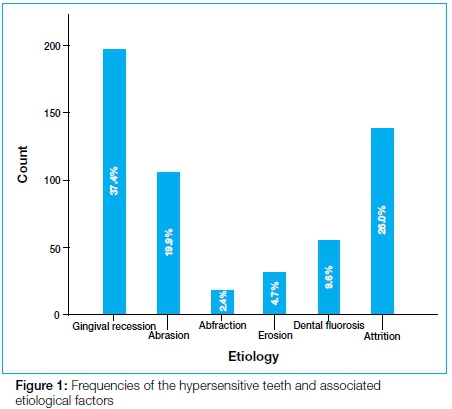
RESULTS: The frequency of hypersensitive teeth (mean 11.5 ±3.8) was significantly (p<0.05) higher for hard compared with soft bristled toothbrush users. The majority of the subjects consumed orange (80.9%) and carbonated drinks (83.3%) frequently, but without significant effect on the mean number of hypersensitive teeth. Gingival recession was observed in 37.4% of the hypersensitive teeth, while abfraction was seen in 2.4%.
CONCLUSION: The use of a hard bristled toothbrush is a risk factor while attrition and gingival recession are the predominant etiological factors for DH in this environment.
INTRODUCTION
Dentine hypersensitivity (DH), is a common dental complaint among young adults. It has been defined as "a chronic condition characterized by a short, sharp pain arising from exposed dentine in response to stimuli, typically thermal, evaporative (air), tactile, osmotic or chemical, and which cannot be ascribed to any other form of dental defect or pathology".1 The first part of the definition points out the cause of the clinical symptoms experienced. As with all conditions or diseases, management strategies which include prevention are usually more successful than treatment alone. Understanding the etiology of a disease condition forms the basis for the preventive measures which may be instituted as part of treatment. The aim in the preventive management of DH is to reduce the risk of exposing the dentine, either as a result of the removal of enamel, or of cementum following gingival recession. Equally, the objective is to prolong the efficacy of prescribed treatment. Ciaramicoli2 demonstrated the importance of prevention in a study that showed that the effects of laser treatment of DH increased when etiological factors were removed.
Enamel loss may result from several factors, while gingival recession is most often attributed to either overzealous tooth brushing in a healthy mouth or periodontal disease and or periodontal treatment.3 Enamel loss with subsequent dentine exposure occurs with tooth wear processes like attrition, abrasion, erosion and abfraction. Attrition is associated with occlusal function resulting in wear of teeth at sites of direct contact between teeth.4 Abrasion as a cause of tooth wear describes tooth tissue loss caused by objects other than another tooth, such as is seen with toothbrush/toothpaste abrasion.5,6,7 Enamel erosion involves dissolution by acids which are not of bacterial origin.5,8 Sources of the acid may be dietary, environmental or intrinsic from regurgitation.8 Abfraction or cervical stress lesions has been hypothesized as an etiological factor in tooth wear, and can lead to hypersensitivity.9'10 These lesions occur most commonly in the cervical region of teeth, where flexure from eccentric loading may lead to breaking away of the extremely thin layer of enamel rods, as well as microfracture of the cementum and dentine.
In addition to these factors, dental fluorosis has been implicated in the etiology of the condition.11,12 Tonguc et al.11 reported a positive association between dental fluorosis and DH. High concentrations of fluoride are known to reduce the mineralization of the teeth, with resultant fluorosis and sensitivity to external stimuli.13 This is supported by Vieria's14 study which showed that a higher dentine fluoride level results in wider dentinal tubules.
Any situation which predisposes to enamel loss or gingival recession will contribute toward the development of DH. The type of toothbrush, frequency of toothbrushing and the diet are some of the factors that have been implicated in the occurrence of gingival recession, tooth wear lesions and DH.4'6'15 The majority of studies have identified erosion and abrasion as the main types of tooth wear lesions associated with DH. These studies may however reflect findings peculiar to the population studied. There is limited direct clinical evidence in the literature of the association of these etiological and predisposing factors to DH in the local environment. Identifying the etiological and predisposing factors among patients with DH seen in the study population will clarify understanding of the condition and will contribute to successful control and prevention of the hypersensitivity.
MATERIALS AND METHODS
The study included all adult patients with complaints of sensitive teeth and diagnosed to have DH at the Oral Diagnosis and Restorative clinics of the Hospital over a one year period. Approval for the study was obtained from the Research and Ethics Committee of the Hospital. All the patients received a detailed explanation about the study and their written consent was obtained before they were included in the study. The diagnosis of DH was based on the history and a clinical examination relying on both tactile and thermal/evaporative stimuli by scratching the tooth surface with a dental explorer followed by a blast of air from the air-water syringe of the dental unit. Patients having teeth with suspected pulpitis, extensive caries, cracked enamel, defective or extensive restorations, and teeth with restorations extending into the test area were not included. Patients who had undergone periodontal surgery, orthodontic appliance treatment and tooth-whitening procedures within the previous three months were also excluded.
A questionnaire was used to collect data from all the subjects included in the study. The information included name, age, sex, occupation, nature of the pain, initiating stimulus, mode of cleaning the teeth and frequency, and intake of acidic drinks. All teeth diagnosed as hypersensitive were examined for the presence of wear facets, the type of non-carious cervical lesions and gingival recession.
Gingival recession was diagnosed when there was apical migration of the gingival attachment with any amount of root exposure. Wear facets on the cusps of the posterior teeth or on the incisal edges of the anterior teeth with flattening of the cusp tips or the incisal edges were recorded as attrition. The abrasive lesions were diagnosed as the presence of a horizontal groove running mesiodistally across the surface of the natural crown at the cemento-enamel junction (CEJ). Abfraction lesions were diagnosed as sharp, angular wedge-shaped lesions, located supragingivally or subgingivally around the CEJ with or without marked wear facets on the occlusal surface of the involved posterior teeth. Fluorosis was diagnosed in the presence of loss of translucency, and or discoloration with or without enamel pitting using the Dean's index (DI). The data were analyzed using Statistical Package for Social Sciences (SPSS) for Macintosh (version 21 SPSS Inc., Chicago, IL, USA). Level of statistical significance was set at p<0.05.
RESULTS
A total of 68 adult subjects were diagnosed with DH comprising 36 (52.9%) males and 32 (47.1%) females with ages ranging from 20 to 53 years and a mean age of 33.8±9.2 years. The 68 study subjects had 508 teeth diagnosed as hypersensitive.
Analysis of the predisposing factors.
The majority of the subjects used toothbrush with paste (77.9%) and had a lower mean number of hypersensitive teeth compared with those who used both toothbrush and chewing stick. None of the subjects used chewing stick alone. The use of a hard bristled toothbrush was significantly associated with a higher mean number of hypersensitive teeth (p= 0.001) (Table 1).
Post hoc tests showed a significantly higher mean number of hypersensitive teeth for subjects using a hard toothbrush when compared with those who use medium or soft toothbrush (df =3, F= 5.894, p= 0.005).
Intake of acidic drinks/drugs
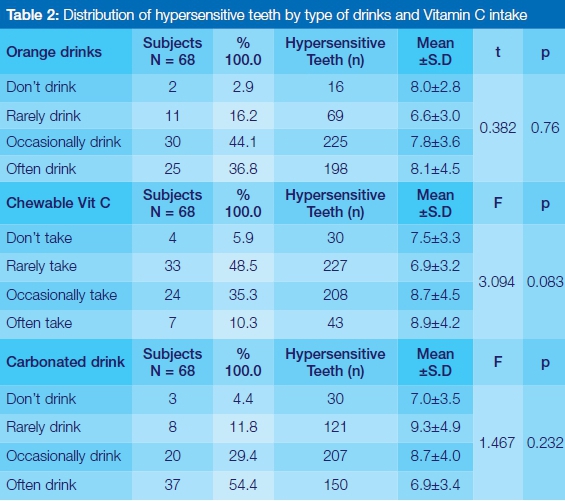
About 83.8% of subjects with DH took carbonated drinks, 80% of subjects consumed orange drinks, while slightly less than half of the subjects consumed chewable vitamin C often or occasionally. However, there was no statistically significant association between the mean number of hypersensitive teeth by frequency of intake of chewable vitamin C, carbonated drinks and orange drinks (p >0.05) (Table 2).
Etiological factors of DH among hypersensitive teeth
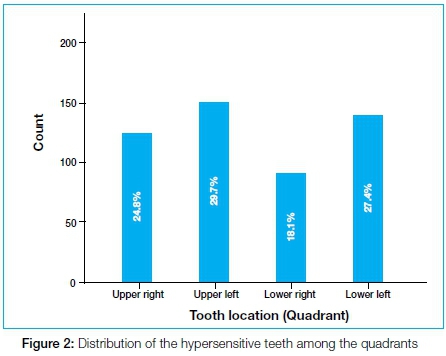
Of the 508 diagnosed hypersensitive teeth, gingival recession was the lesion most commonly associated with DH (190, 37.4%) while abfractive lesion was the least frequent (Figure 1). The hypersensitive teeth occurred more often on the upper and lower left quadrants and accounted for 151 (29.7%), and 139 (27.4%) of the 508 total hypersensitive teeth (Figure 2). Figure 3 illustrates the distribution of the hypersensitive teeth and the associated tooth wear lesions and dental fluorosis among the quadrants.
DISCUSSION
Evidence suggests that the preventive aspects of the management of DH are not usually considered by many clinicians when treating the condition.16,17 Indeed, the treatments available for DH have limited efficacy over time, requiring repeated applications. Addy18 thus proposed that the clinician should identify and modify the etiological and predisposing factors of DH as part of the management of a patient with the condition.
This study set out to identify the predisposing and etiologic factors for DH that should be modified in people suffering from the condition. In the subjects studied, those who used both toothbrush with paste and chewing stick had a higher mean number of hypersensitive teeth than subjects who used only toothbrush and paste although the difference was not significant. The higher mean number of hypersensitive teeth in the former group may be due to the additional use of chewing stick, which has been documented as causing gingival recession and tooth wear.19 Chewing sticks are usually cut or carved out of trees and shrubs. The stick is held at one end with the other end placed into the mouth where it is chewed into a fibrous brush-like fringe. When the brush is formed, the fringe is used to scrub the surfaces of the teeth. The process of chewing to soften it and the actual scrubbing to clean the teeth may result in gingival recession and tooth wear if used inappropriately. Omani patients were reported to have significantly more sites with gingival recession among chewing stick users when compared with toothbrush users.20 However, the effect of chewing stick alone on DH could not be ascertained in the present study because none of the subjects who participated used a chewing stick alone to clean their teeth.
Whilst most of the subjects used medium-bristled toothbrushes, the mean number of hypersensitive teeth was observed to be highest among hard-bristled toothbrush users. Colak21 reported that more than half of the subjects in his study who had DH used hard-bristled toothbrushes. Bamise et al.6,22 also supported these findings in two separate studies, where there were significant correlations between tooth wear, DH and the use of hard bristled toothbrush.
A direct relationship was observed between the mean number of hypersensitive teeth and the frequency of tooth brushing, though this was not statistically significant. This result should be interpreted with caution as there was only one subject who brushed three times a day and had the highest mean score for hypersensitive teeth. Also, two subjects brushed more than three times a day, but, surprisingly, had the lowest mean number of hypersensitive teeth. The literature supports the notion that there is an association between the frequency of toothbrushing, gingival recession and occurrence of DH.23,24
Higher percentages of subjects in this study consumed carbonated drinks and orange juice as opposed to those who chewed the flavoured vitamin C. This is similar to the findings of Bamise et al.15 who reported a strong association between DH and the consumption of citrus drinks and carbonated drinks, but not with vitamin C. This implies that erosion may have contributed to the prevalence of DH among the subjects in this present study. Most people consume vitamin C rarely, except those on medications by prescription. However, most of those who take vitamin C also consume orange juice and carbonated drinks. Orange juice and carbonated drinks are commonly consumed on daily basis in Nigeria and the demand for these drinks has grown rapidly over the past decade.25,26 It may be expected to contribute to the development of DH. The drinks could either be primary etiological factors, causing dental erosion, or exert a secondary effect, by removing the smear layer from already exposed dentinal tubules.
There was however no significant difference in the mean number of hypersensitive teeth when those who drink orange juice, carbonated drinks and take chewable vitamin C often were compared with those who do not consume these items at all. This may signify the presence of other important etiological or predisposing factors in these subjects. It is also important to note that the contribution of the acidic drinks to the formation of erosive lesions may be influenced by behavioral characteristics of the consumers. These include the manner of intake (with or without straws), and the duration of contact with the teeth.27,28
Gingival recession was the most common etiological factor associated with DH among the subjects, followed by attrition, abrasion, fluorosis, erosion and abfraction in that order. Overall, 190 of the 508 hypersensitive teeth (37.4%) had some associated buccal gingival recession. Gingival recession exposes the CEJ as well as the cementum, predisposing the tissue to toothbrush abrasion. Hypersensitivity at sites with gingival recession in the absence of abrasion may partly be explained by the presence of exposed dentine at the CEJ due to anatomical variations. Addy et al.29 and Rees and Addy30 also report that most teeth in their sample of hypersensitive teeth had some degree of gingival recession. These findings are in contrast to reports by Bamise et al.,15 and Özcan and Çanaci6 who reported attrition as the most common etiological factor for DH in their studies. This probably reflects differences among populations studied by different researchers. In the study by Bamise et al.15 the consumption of coarse diets by patients was suggested as the reason for the attrition. The present study is in consonance with those of Bamise et al.,15 and Özcan and Çanaci6 in that attrition was the most common tooth wear lesion associated with DH. Although not evidenced in this study, the reason for the association may be due to the consumption of coarse diet in this population.
Presently, DH studies on populations that are endemic for dental fluorosis are rare. Zhang et al.12 in a Chinese study, associated DH to dental fluorosis in a rural community with dental fluorosis. Tonguc et al.11 compared two different populations and observed a significantly higher prevalence of DH in the population endemic for dental fluorosis. Dental fluorosis is prevalent in the present study area because of high fluoride content in the drinking water, as high as 4.6mg/l.31,32 Fluorosis may present with pitting of the enamel, which may result in dentine exposure. This study revealed the presence of DH in teeth with dental fluorosis accounting for 9.7% of the total number of teeth with DH. Unlike the study by Tonguc et al,11 this study did not compare the prevalence of DH among those with signs of fluorosis and those without.
DH resulting from abfraction is the factor recording the least influence in this study. Bamise et al.,15 and Özcan and Çanaci6 also observed abfraction as the least etiological factor associated with DH in their groups of subjects. It was however suggested that the low result with abfraction may be due to difficulty in diagnosing such lesions.6 Strong attention was paid in the current study to the diagnosis of these abfraction lesions, and yet it remained the least influential cause of DH. More controlled studies on abfraction and DH are indicated.
CONCLUSION
The majority of the subjects consumed acidic drinks but this was not shown to be a major contributory factor for DH. The use of hard bristled toothbrush is a risk factor for DH, especially when combined with the use of chewing stick. Gingival recession and attrition were the most common etiological factors. Although not one of the major etiological factors, dental fluorosis was identified as contributing to the occurrence of DH in the subjects studied. The findings from this study may be used to recommend individualization of preventive treatment for every patient as elicited from the history and examination to prevent further exposure of dentine, as well as to improve the efficacy and longevity of the treatment. In the samples studied, preventive emphasis will be on the type of toothbrush, and the use of chewing stick. Further studies to look at the association between the intakes of coarse diet, attrition and DH should be considered.
ACRONYMS
DH: dentine hypersensitivity
CEJ: cemento-enamel junction
References
1. Chabanski MB, Gillam DG, Bulman JS, et al. Clinical evaluation of cervical dentine sensitivity in a population of patients referred to a specialist periodontology department: a pilot study. J Oral Rehabil. 1997; 24(9): 666-72. [ Links ]
2. Ciaramicoli MT, Carvalho RCR, Eduardo CP. Treatment of cervical dentine hypersensitivity using neodymium:yttrium-aluminum- garnet laser: clinical evaluation. Lasers Surg Med. 2003; 33: 358-62. [ Links ]
3. Taani Q, Awartani F. Clinical evaluation of cervical dentin sensitivity (CDS) in patients attending general dental clinics (GDC) and periodontal specialty clinics (PSC). J Clin Periodontol. 2002; 29: 118-22. [ Links ]
4. Özcan E, Çanaci F. An analysis of aetiological factors related to dentine hypersensitivity and severity. J Dent Fac Atatürk Uni. 2010; 20(3): 145-52. [ Links ]
5. Grippo, JO, Simring M, Schreiner S. Attrition, abrasion, corrosion and abfraction revisited: a new perspective on tooth surface lesions. J Am Dent Assoc. 2004; 135(8): 1109-18. [ Links ]
6. Bamise CT, Olusile AO, Oginni AO, et al. The prevalence of dentine hypersensitivity among adult patients attending a Nigerian teaching hospital. Oral Health and Prevent Dent. 2007; 5(1): 49-53. [ Links ]
7. West NX. Dentine hypersensitivity: preventive and therapeutic approaches to treatment. Periodontol 2000 2008; 48: 31 -41. [ Links ]
8. Zero DT, Lussi A. Erosion-chemical and biological factors of importance to the dental practitioner. Int Dent J. 2005; 55: 285-90. [ Links ]
9. Rees JS: The biomechanics of abfraction. Proc Inst Mech EngH. 2006; 220: 69-80. [ Links ]
10. Grippo JO. Non-carious cervical lesions: the decision to ignore or restore. J Esthet Dent. 1992; 4(supplement): 55-64. [ Links ]
11. Tonguc MO, Ozat Y, Sert T, Sonmez Y, Kirzioglu FY. Tooth sensitivity in fluorotic teeth. Eur J Dent. 2011; 5: 273-80. [ Links ]
12. Zhang Y, Cheng R, Cheng G, Zhang X. Prevalence of dentine hypersensitivity in Chinese rural adults with dental fluorosis. J Oral Rehab. 2014; 41: 289-95. [ Links ]
13. Jälevik B, Klingberg GA. Dental treatment, dental fear, and behavior management problems in children with severe enamel hypomineralisation of their first permanent molars. Int J Pediatr Dent. 2002; 12: 24-32. [ Links ]
14. Viera APGF, Hancock R, Dumitriu M, Limeback H, Grynpas MD. Fluoride's effect on human dentine ultrasound velocity (elastic modulus) and size. Eur J Oral Sci. 2006; 114: 83-8. [ Links ]
15. Bamise CT, Olusile AO, Oginni AO. An analysis of etiological and predisposing factors related to dentin hypersensitivity. J Contemp Dent Pract. 2008; 1(9): 52-9. [ Links ]
16. Rees JS, Jin LJ, Lam S, et al. The prevalence of dentine hypersensitivity in a hospital clinic population in Hong Kong. J Dent. 2003; 31: 453-61. [ Links ]
17. Al-Sabbagh M, Beneduce C, Andreana S, et al. Incidence and time course of dentinal hypersensitivity after periodontal surgery. Gen Dent. 2010; 58: e14-9. [ Links ]
18. Addy M. Dentine hypersensitivity: new perspectives on an old problem. Int Dent J. 2002; 52(Suppl 1): 367-75. [ Links ]
19. Absi EG, Addy M, Adams D. Dentine hypersensitivity. The effects of tooth brushing and dietary compounds on dentine in vitro: a SEM study. J Oral Rehab. 1992; 19: 101-10. [ Links ]
20. Eid MA, Selim HA, Al-Shammery AR. The relationship between chewing sticks (Miswak) and periodontal health. Part III. Relationship to gingival recession. Quintessence Int. 1991; 22: 61-4. [ Links ]
21. Çolak H, Aylikçi BU, Hamidi MM, et al. Prevalence of dentine hypersensitivity among university students in Turkey. Niger J Clin Pract. 2012; 15: 415-9. [ Links ]
22. Bamise CT, Kolawole KA, Oloyede EO, et al. Tooth sensitivity experience among residential university students. Int J Dent Hyg. 2010; 8: 95-100. [ Links ]
23. Levitch LC, Bader JD, Shugars DA, et al. Non-carious cervical lesions. J Dent. 1994; 22: 195-207. [ Links ]
24. McCraken GI, Heasman L, Stacey F, et al, A clinical comparison of an oscillating/rotating powered toothbrush and a manual toothbrush in patients with chronic periodontitis. J Clin Periodontol. 2004; 31(9): 805-12. [ Links ]
25. Abdullahi MK, Yakubu AA. Determinants of Non-Alcoholic Beverages (NAB) consumption in North-Western Nigeria: A study of Sokoto Metropolis. Nig J Basic Appl Sci. 2013; 21(4): 273-81. [ Links ]
26. Bamise CT, Olusile AO, Kolawole KA, Peter AO. Beverages drinking habits and tooth sensitivity experience among adolescent secondary school students. JRD. 2014; 2(2): 150-8. [ Links ]
27. Zero DT. Etiology of dental erosion: extrinsic factors. Eur J Oarl Sci. 1996; 104: 162-77. [ Links ]
28. Edwards M, Ashwood RA, Littlewood SJ, Brocklebank LM, Fung DE. A videofluoroscopic comparison of straw and cup drinking: the potential influence on dental erosion. Br Dent J. 1998; 185: 244-9 [ Links ]
29. Addy M, Mostafa P, Newcombe RG. Dentin hypersensitivity: the distribution of recession, sensitivity plaque. J Dent. 1987; 15: 242-8. [ Links ]
30. Rees JS, Addy M. A cross-sectional study of dentine hypersensitivity. J Clin Periodontol. 2002; 29: 997-1003. [ Links ]
31. Bura B, Goni IB. Tracing the factors influencing occurrence of fluoride in groundwater of the Middle Zone aquifer in Borno State, North-Eastern Nigeria. J Min Geo. 2012; 48(2): 177-84. [ Links ]
32. Waziri M, Musa U, Hati SS. Assessment of fluoride concentrations in surface waters and groundwater sources in Northeastern Nigeria. Res Environ. 2012; 2(2): 67-72. DOI: 10.5923/j.re.20120202.10 [ Links ]
 Correspondence:
Correspondence:
Dr. Paul ikhodaro idon
Department of Dental Surgery
University of Maiduguri Teaching Hospital
Maiduguri, Borno State, Nigeria
Tel: 234 803 389 0578
E-mail: idonp85@gmail.com














