Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.73 n.5 Johannesburg Jun. 2018
http://dx.doi.org/10.17159/2519-0105/2018/v73no5a4
RESEARCH
Prevalence and aetiological factors of maxillofacial trauma in a rural district hospital in the Eastern Cape
L PillayI; M MabongoII; B BuchIII
IBDS(SSRMC, MUR), MSc Dent(Wits), Zithulele Hospital, Eastern Cape Department of Health, South Africa
IISIS (UNITRA), B Den (Medunsa), BDS(Wits), MSc Dent(Wits), MChD (MFOS)(UWC), Cert. Orofacial Pain (Rugter, USA), FCFS (Bangalore, India). Head, Clinical Unit, Department of Oral and Maxillofacial Surgery, School of Oral Health Sciences, University of the Witwatersrand, Johannesburg
IIIBSC Hons (Natal),SED (UCT), BDS (Wits), MSc Dent (Wits). Emeritus Professor, University of Pretoria, Visiting Professor and Part Time Consultant, Division of Maxillo-Facial and Oral Radiology, Department of General Dental Practice, School of Oral Health Sciences, University of the Witwatersrand, Johannesburg
ABSTRACT
AIM: To determine the prevalence, aetiological factors and demographic data of patients presenting with injuries sustained from maxillofacial trauma over a six month period at Zithulele Hospital
MATERIALS AND METHODS: In a retrospective, descriptive study, data collected and analysed included records of all patients who had suffered maxillofacial trauma, their demographics, clinical features and the aetiology. The radiographic records were assessed by a maxillofacial surgeon and a radiologist for a diagnosis as well as gaining opinions regarding the types of fractures observed.
RESULTS: A total of 239 patients sustained maxillofacial trauma. The most common aetiological factor was interpersonal violence (55%) followed by road traffic accidents (16%), falls (10%), animals (4%) and other causes (2%). The male to female ratio was 2.6:1 and the 18-24 years age group endured the most trauma. A total of 210 (88%) patients sustained soft tissue injuries while 29 (12%) experienced hard tissue injuries, with 39 fractures diagnosed. A total of 165 maxillofacial radiographs were assessed, 37% were diagnostically acceptable, 56% had poor diagnostic value and 7% had no diagnostic value.
CONCLUSION: Maxillofacial trauma is prevalent in rural parts of South Africa. Males aged 18-24 years are frequent victims, with interpersonal violence being the major aetiology.
INTRODUCTION
Maxillofacial trauma is any injury sustained to the face, jaws and related structures and includes both soft and hard tissue injuries. The maxillofacial region, composed of the following bones: frontal, nasal, ethmoid, zygomatic, maxillary bones and the mandible, is divided into three parts: the upper face, midface and lower face.1 The lower third of the face is formed by the mandible along with its dento-alveolar arch. The middle third of the face is the area between the supraorbital margins and the occlusal plane of the upper teeth and the upper third of the face is the region above the supraorbital margins. Amongst these, the most commonly fractured is the mandible followed by fractures in the nasal, zygomatic and maxillary bones.2
LITERATURE REVIEW
Facial injuries are a common feature in trauma units worldwide and are known to cause significant deformity, loss of function and in severe cases, can be life-threatening.3 The type of injuries range from harm to soft tissue to damage to hard tissue. Soft tissue injuries include burns, lacerations, bruises, avulsions and abrasions and in the face may involve damage to the major salivary glands, muscles, cranial nerves, eyes and connective tissue.4 Hard tissue injuries include trauma to the dentition, dislocations of the temporomandibular joint and fractures to the bony maxillofacial complex. A major concern with soft tissue injuries is wound contamination and, for cosmetic reasons, tissue scarring.5
The management of these injuries is carefully planned and coordinated by maxillofacial and plastic surgeons. Depending on the object and the velocity reached when it contacts soft tissue, soft tissue injuries can range from superficial harm to deep penetrating wounds with significant tissue loss. The biomechanics of trauma is the biological response of tissue to the mechanics of the impact.6,7 The extent of maxillofacial trauma can be determined by considering the biomechanics involved during the injury, information which is usually obtained through a correlation of the results of a thorough clinical examination with a detailed history of the traumatic event.
Patel et al. reported that 12.6% of the trauma patients in their study suffered post traumatic cranial nerve injury. The facial nerve was the most frequently damaged, followed by the oculomotor and optic nerves.8 It can therefore be said that the results of maxillofacial trauma can be quite complicated.
On completion of a comprehensive clinical examination, specific radiographs are usually requested for the diagnosis of facial fractures.9 A complete radiological examination forms a crucial part in the diagnosis of hard tissue injuries and in determining the location of foreign bodies within soft tissue. It provides valuable information on the site of the fractures, the degree of displacement and the effects on surrounding structures. Radiographs used routinely for the diagnosis of maxillofacial trauma include: lateral cephalometric projection; submentovertex; Waters view; posterior-anterior skull projection; reverse Townes; mandibular lateral projection and panoramic views. However, conventional radiographs are becoming less popular with the availability of computer tomography and magnetic resonance imaging.9
The treatment of maxillofacial trauma is more complex and challenging than trauma elsewhere in the body. Most of the treatment modalities for trauma sustained on other parts of the body are aimed at restoring function, whereas in the maxillofacial region aesthetics are a major concern and pose difficulties for the medical personnel.10 Studies have shown significant psychological and functional problems that are associated with maxillofacial trauma and depression is often seen when aesthetics are compromised.11
The most common causes of maxillofacial trauma have been reported to be: traffic accidents, mainly motorcycle accidents, followed by physical assaults, falls and sports-related accidents.12 The major factors influencing the incidence of maxillofacial trauma are age, gender, geographic region, substance abuse, compliance to traffic legislation, domestic violence and interpersonal violence.13 A South African investigation has determined the main cause to be interpersonal violence.14
Around the world, these causative factors are largely influenced by differences in socio-economic status, culture and environmental factors.15 Sports-related trauma tends to occur more frequently in higher socioeconomic areas, while Brasileiro et al. reported a high incidence of violence- related trauma in lower socioeconomic strata.16 A number of studies indicate substance abuse to be a major contributing factor to the occurrence of facial injuries within the variable of interpersonal violence.17 A South African study conducted by Desai et al, reported that 65% of their cases of maxillofacial trauma were associated with alcohol.18 This suggests that there is a significant correlation between alcohol consumption, interpersonal violence and maxillofacial trauma. Different geographical areas also demonstrate different patterns of cause and presentation.19
All age groups may be affected by maxillofacial trauma. The incidence has been shown to ranges from 1 to 99 years with a median of 22 years and mean of 25.8 years.20 In the geriatric population, studies have shown that falls were the most common cause of maxillofacial trauma, This is due to age-related changes in the sensory systems of these older people.21 Of note is the report that amongst the paediatric population, falls are also reported to be a major cause.22 These studies suggest that aetiologies are related to age and that certain age groups are more predisposed to specific aetiologies.
In studies on the gender distribution of maxillofacial trauma, Boffano et al. reported a male to female ratio of 11.8:1.23 The male to female ratio of maxillofacial trauma was higher in rural areas than in urban areas24 and the most commonly affected age group was between 21-30 years.25 In another South African study on the patterns of interpersonal violence, males were mostly affected and the face was the second most commonly injured area.26 Males are more at risk to trauma as compared with females, attributable to differences in behavioural activities.27 Studies have shown the type of injuries that males sustain are significantly more serious than those which are sustained by females, with a higher mortality and morbidity rate.28 The rapid change in the socio-economic status of populations has created both the opportunity and the need for females to perform a broader range of work. This has required greater physical demands and has increased their vulnerability to maxillofacial trauma.29
A South African study showed that alcohol consumption is a greater contributing factor in males.30 In 2014, the World Health Organizations global status on alcohol and health showed alcohol to be the leading risk factor for mortality in males and that females are predisposed to suffer alcohol related harm.31 Overall, the incidence and characteristics of maxillofacial trauma differ depending on the geographical area and socio-economic status of populations.24
In South Africa, the referral system in the health sector requires that patients are expected to present for immediate primary care at the primary healthcare centres and at community healthcare centres, for intermediate or generalist care at the district hospitals, and for advanced diagnostic procedures and treatment, at the tertiary hospital.32 Anecdotal evidence suggest that most primary health care facilities do not have adequate resources, such as radiology for diagnosing maxillofacial fractures, and that those primary health care workers who may be managing maxillofacial injuries are not familiar with correct diagnostic imaging and lack skills in the diagnosis of maxillofacial fractures. There has been no research conducted in the Eastern Cape on the epidemiology and aetiology of maxillofacial trauma. A project to investigate these factors will gain knowledge of the maxillofacial trauma in a South African rural region. This will allow clinicians within the region to adopt appropriate diagnostic aids and treatment modalities. Specialised training programs can then be developed, thus saving time and money and allowing for scarce resources to be allocated more effectively.
The aim of this study was to evaluate the prevalence, aetiological factors and demographic data of patients presenting with maxillofacial trauma over a six month period at Zithulele, a 140 bed district hospital located in rural Eastern Cape. The facility services a population of 130 000 inhabitants, and is about 300km from East London, where may be found the nearest maxillofacial surgeon to whom referral can be made.
MATERIALS AND METHODS
Study Design and Population
Study Design
A retrospective, descriptive study was undertaken to analyse the prevalence and aetiological factors of maxillofacial trauma at Zithulele Hospital, over a six month period (October 2015 - March 2016).
Study population
The method of convenience sampling was used to determine the study population within a specific time frame (October 2015 - March 2016). A total of 8262 patients who were triaged in casualty within the specified period were considered for inclusion in the study. Of this total, it was determined that the records of 239 patients who had sustained maxillofacial trauma met the requirements. Incomplete records, missing records and any recorded trauma not within the specified period lead to exclusion of the case from the study.
Data Collection
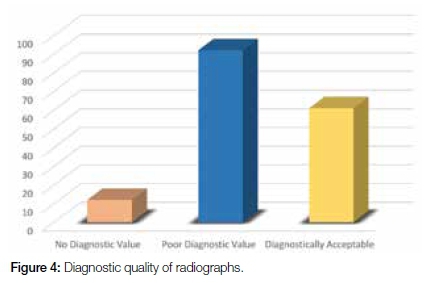
A data collection sheet was used by the principal investigator to record the data. Variables collected were aetiology, gender, age, diagnostic quality of radiographs, nature of injury (soft or bone) and site of fractures. A maxillofacial surgeon and a radiologist skilled in maxillofacial interpretation assessed the quality of the radiographs and their suitability as a basis for an adequate diagnosis. The patterns of hard tissue trauma were classified anatomically into different types of fractures with the assistance of these clinicians who were also requested to offer their own diagnoses and opinions of the types of fractures seen. The radiographs were classed as: a) no diagnostic value; b) poor diagnostic value; and c) acceptable diagnostic value.
Data Analysis
The assessor's interpretation of the radiographs was captured on an Excel sheet. Reliability was determined with Cohen's Kappa inter-rater reliability test. Descriptive statistics were used to demonstrate the results. Tables and graphs were used to illustrate the outcomes.
Ethical consideration
The Clinical Manager of Zithulele Hospital granted permission to conduct research at the Institution and the Human Research and Ethics Committee at the University of Witwatersrand granted ethical clearance to conduct this study (M160832).
Limitations
A limitation in the study were hospital-held records that were not as descriptive as would have been those for a study with a predetermined format for capturing data. Some of the records were missing data or presented incomplete information. Many radiographs had no or poor diagnostic value making it difficult to accurately diagnose the type of fracture seen.
RESULTS
Prevalence of maxillofacial trauma
A total of 8262 outpatient records for the period 1st October 2015 - 31st March 2016 was considered During this period 239(2.89%) patients had sustained maxillofacial trauma.
Frequency of aetiological factors
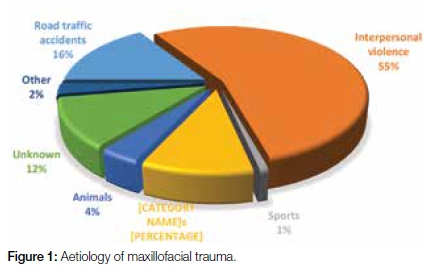
The most common aetiological factor was interpersonal violence which accounted for 131 patients (55%), the second most common being road traffic accidents (38 patients, 16%). Falls had resulted in 25 (10%) of the injuries and in nine cases, the trauma had been caused by animals (4%).Other causes (2%) included four patients who sustained burns to the face, one having been cut by a roofing sheet (Figure 1).
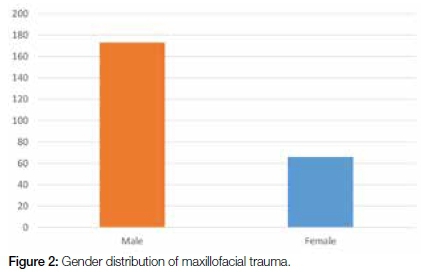
Females versus males
Of 239 patients, 173(72%) were male and 66(28%) female (Figure 2). The male to female ratio was 2.6:1. Data analysis showed that males were more prone to maxillofacial trauma than females (χ2 = 74.55, d.f. = 1, p < 0.001).
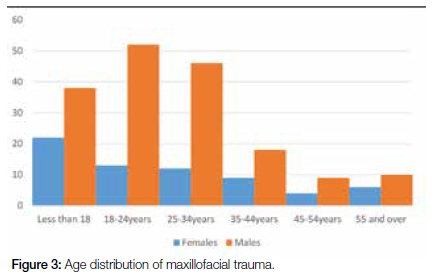
Age range
The age of patients ranged from 1 to 74 years, with a median of 24 and a mean of 26.3 (standard deviation: 15.4). The age group diagnosed with the most maxillofacial trauma was that between 18 to 24 years, accounting for 27% of the patients. The second most frequent age group fell into the category of under 18 years, 24% of the sample (Figure 3).
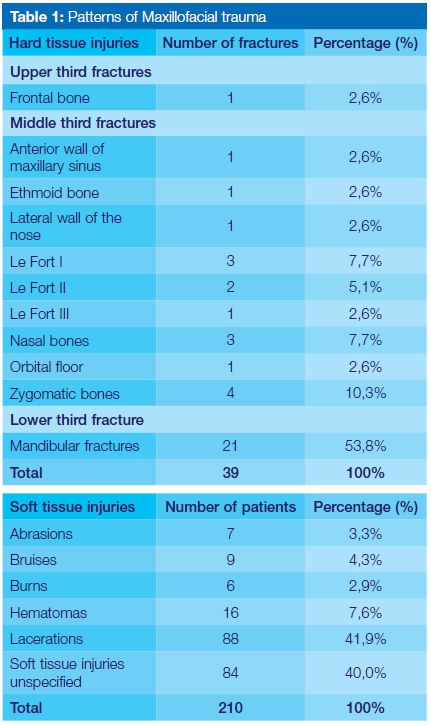
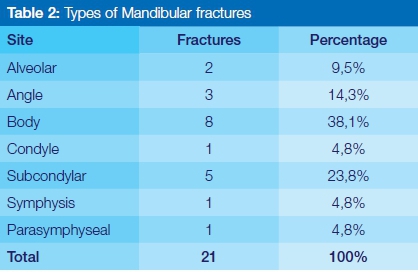
Patterns of trauma
A total of 210(88%) patients sustained soft tissue injuries while 29 (12%) suffered hard tissue injuries, often multiple. Of these, there were 39 fractures diagnosed. The most frequently fractured bone was the mandible at the body (Table 2). Zygomatic bone fractures were the second most frequently observed followed by the nasal bones and Le Fort I displacements. Among the soft tissue injuries, 41.9% sustained lacerations, 7.6% presented haematomas while in 40% of cases the soft tissue injuries were unspecified (Table 1).
Diagnostic quality of radiographs
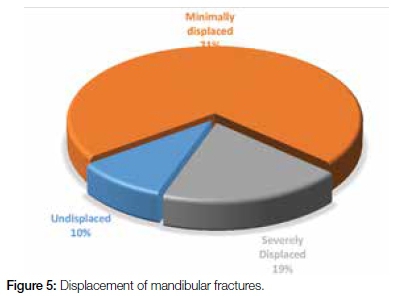
A total of 165 maxillofacial radiographs were sent to both a maxillofacial surgeon and a radiologist skilled in maxillofacial interpretation for assessment. Their findings indicated that 7% and 56% were of no or poor diagnostic value, whilst 37% were diagnostically acceptable (Figure 4). The were 39 fractures which had been diagnosed from those radiographs that had diagnostic value. Assessment of the panoramic images confirmed that 71% of the mandibular fractures were minimally displaced (Figure 5). Cohen's Kappa inter-rater reliability test was used to assess the agreement between the two assessors. This demonstrated a Kappa (κ) value of 0.97 (0.81-0.99), an almost perfect agreement.33
DISCUSSION
Maxillofacial trauma is still a common presentation in emergency units worldwide.3 The prevalence of maxillofacial trauma in this study was 2.89 %, rather lower than the 16% which was found in a similar study conducted in Australia (16%). This difference could be attributed to variation in the socioeconomic status of the study population and their exposure to risk factors.34 In fact, the prevalence found in this study is also lower than that reported from tertiary hospitals in other parts of South Africa.13 Variation of prevalence in different geographic regions could be influenced by factors such as urbanization, socioeconomic status, cultural differences, crime rate, period of study and environmental factors.
The most common aetiological factors were interpersonal violence (55%), road traffic accidents (16%) and falls (10%). This sequence was also reported in a Bulgarian study.2 The findings are closely related to a Brazilian study which identified a high incidence of violence-related trauma in lower socioeconomic areas.16 A recent study compared two maxillofacial units in South Africa, finding interpersonal violence to be the leading cause.13 In contrast, certain studies have revealed road traffic accidents to be the leading cause of maxillofacial trauma.28,35,36 However, in this study, only 16% of the patients had suffered road traffic accidents. Only one patient had sustained maxillofacial injuries from a gunshot, whereas in other parts of South Africa maxillofacial gunshot wounds are a common finding.37
In this study males were more frequently injured as compared with females, with a male to female ratio of 2.6:1. Other South African studies on maxillofacial trauma have shown a similar trend with males being mostly affected.13,18,37,38 Batista et al. reported a higher male to female ratio in rural areas as compared with urban areas.24 This higher prevalence in males can be correlated with a South African study which showed that alcohol consumption is a much more significant contributing factor in males as compared with females.30 Desai et al. found that 65% of maxillofacial trauma was associated with alcohol.18 Urban areas record much higher levels of alcohol consumption than do rural areas.39 Whilst alcohol usage predisposes females to alcohol-related harm,31 it is the leading risk factor for mortality in males, possibly related to behavioural activities which expose them to trauma.
The prevalence of maxillofacial trauma in this study was higher (52%) in patients younger than 24 years. This finding concurs with the study by Lee on the Global Trends in Maxillofacial Fractures, which showed a high prevalence of maxillofacial trauma in males aged 16 to 30 years and also agrees with the data of similar studies conducted in tertiary hospitals in South Africa.13,15,18,37
The majority of hard tissue injuries were fractures in the lower third of the face, while soft tissue injuries were mainly lacerations. This is consistent with various South African studies which have reported mandibular fractures to be the most common fractures of the face.13,37,38 However, due to the low number of maxillofacial fractures, no conclusions can be made on the site most commonly affected with fractures.
Imaging of the maxillofacial region can be challenging in trauma patients and conventional radiographs are becoming less popular as a result of the availability of computer tomography.40,41 The specialists who reviewed the radiographs agreed that most of these radiographs were inappropriate for the diagnosis of maxillofacial fractures. This suggests that either maxillofacial fractures were incidental findings or that the attending clinician had requested inappropriate radiographic projections for the diagnosis of these fractures. Since most of the mandibular fractures that were diagnosed on the panoramic radiographs were minimally displaced, almost all of these fractures could in fact be managed by closed reduction by a general dentist.
CONCLUSION
The prevalence of maxillofacial trauma at Zithulele Hospital for the study period was 2.89 %( 239 patients) indicating a low prevalence. Interpersonal violence is still the leading cause of maxillofacial trauma around the world and more especially in rural areas of the Eastern Cape. Younger males aged 18-24 years are still common victims of trauma, with interpersonal violence being a major contributing factor. Patients in rural areas are exposed to low velocity trauma that result in injuries easily managed by a generalist.
RECOMMENDATION
This information will allow clinicians within the region to adopt specific diagnostic aids and treatment modalities and will be useful in the creation of preventative programs involving the healthcare provider, police, schools and non-government organizations and which are designed to reduce the crime rate. Most of the identified mandibular fractures were minimally displaced indicating that onservative management would be possible by closed reduction at rural hospitals. Dentists should receive more intense training on minor oral surgical procedures if they intend working in rural parts of South Africa. There are very few maxillofacial surgeons who work in the public sector in the Eastern Cape. The Department of Health needs to work closely with the tertiary education centres to create more supplemental posts, thereby enhancing the possibility of increasing the number of maxillofacial surgeons in the Province.
The maxillofacial region is a complex region requiring a multidisciplinary team approach with detailed imaging for the diagnosis of fractures. The conclusions in this study regarding the radiographs suggest that more training is required on maxillofacial imaging to improve the diagnostic quality of radiographs. Medical doctors and dentists need to be adequately trained in the choice and interpretation of maxillofacial radiographs. This can be achieved by seminars, lectures and short courses on maxillofacial trauma, which could reduce the chances of fractures being missed or misdiagnosed.
References
1. Angelopoulos C. Anatomy of the maxillofacial region in the three planes of section. Dental Clinics of North America 2014;58(3):497-521. [ Links ]
2. Deliverska EG, Rubiev M. Facial fractures and related injuries in Department of Maxillo-Facial Surgery, University Hospital "St. Anna", Sofia, Bulgaria. Journal of IMAB - Annual Proceeding (Scientific Papers) 2013;19(2):289-91. [ Links ]
3. Alvi A, Doherty T, Lewen G. Facial fractures and concomitant injuries in trauma patients. The Laryngoscope 2003;113(1):102-6. [ Links ]
4. Hogg NJ, Horswell BB. Soft tissue pediatric facial trauma: a review. Journal-Canadian Dental Association 2006;72(6):549. [ Links ]
5. Parashar A, Sharma RK. Unfavourable outcomes in maxillofacial injuries: How to avoid and manage. Indian Journal of Plastic Surgery 2013;46(2):221. [ Links ]
6. Gong SW, Lee HP, Lu C. Dynamic response of a human head to a foreign object impact. IEEE Transactions on Biomedical Engineering 2008;55(3):1226-9. [ Links ]
7. Clasper J. The interaction of projectiles with tissues and the management of ballistic fractures. Journal of the Royal Army Medical Corps 2001;147(1):52-61. [ Links ]
8. Patel P, Kalyanaraman S, Reginald J, Natarajan P, Ganapathy K, Bapu KS, Thamburaj AV, Chendhilnathan B, Balamurugan M. Post-traumatic cranial nerve injury. Indian Journal of Neurotrauma 2005;2(01):27-32. [ Links ]
9. Ali I, Gupta A. Imaging in maxillofacial trauma. Central India Journal of Dental Sciences 2012; 3 (4):223-233. [ Links ]
10. Kretlow JD, McKnight AJ, Izaddoost SA. Facial soft tissue trauma. Seminars in Plastic Surgery 2010; 24(4): 348. [ Links ]
11. Levine E, Degutis L, Pruzinsky T, Shin J, Persing JA. Quality of life and facial trauma: psychological and body image effects. Annals of Plastic Surgery 2005;54(5):502-10. [ Links ]
12. Leles JL, Santos ÊJ, Jorge FD, Silva ET, Leles CR. Risk factors for maxillofacial injuries in a Brazilian emergency hospital sample. Journal of Applied Oral Science 2010;18(1):23-9. [ Links ]
13. Chrcanovic BR. Factors influencing the incidence of maxillofacial fractures. Oral and Maxillofacial Surgery 2012;16(1):3-17. [ Links ]
14. Mogajane BM, Mabongo M, Rikhotso E, Masipa JN. Comparison of epidemiologic characteristics of maxillofacial fractures between two maxillofacial units. 2012 (In press). [ Links ]
15. Lee K. Global trends in maxillofacial fractures. Craniomaxillofacial Trauma and Reconstruction 2012;5(4):213. [ Links ]
16. Brasileiro BF, Passeri LA. Epidemiological analysis of maxillofacial fractures in Brazil: a 5-year prospective study. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics 2006;102(1):28-34. [ Links ]
17. O'Meara C, Witherspoon R, Hapangama N, Hyam DM. Alcohol and interpersonal violence may increase the severity of facial fracture. British Journal of Oral and Maxillofacial Surgery 2012;50(1):36-40. [ Links ]
18. Desai J, Lownie JF, Cleaton-Jones P. Prospective audit of mandibular fractures at the Charlotte Maxeke Johannesburg Academic Hospital. South African Journal of Surgery 2010;48(4):122-6. [ Links ]
19. Jin Z, Jiang X, Shang L. Analysis of 627 hospitalized maxillofacial-oral injuries in Xi'an, China. Dental Traumatology 2014;30(2):147-53. [ Links ]
20. Gassner R, Tuli T, Hächl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9543 cases with 21067 injuries. Journal of Cranio-Maxillo-Facial Surgery 2003;31(1):51-61. [ Links ]
21. Channar K a LI, Memon AB. Pattern and causes of maxillofacial trauma among senior citizens. Pakistan Oral and Dental Journal 2016;36(3):372-4. [ Links ]
22. Jung TK, De Silva HL, Konthasingha PP, Tong DC. Trends in paediatric maxillofacial trauma presenting to Dunedin Hospital, 2006 to 2012. New Zealand Dental Journal 2015;111(2). [ Links ]
23. Boffano P, Roccia F, Zavattero E, Dediol E, Uglesic V, KovaCic Z, Vesnaver A, Konstantinovic VS, Petrovic M, Stephens J, Kanzaria A. Assault-related maxillofacial injuries: the results from the European Maxillofacial Trauma (EURMAT) multicenter and prospective collaboration. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 2015;119(4):385-91. [ Links ]
24. Batista AM, Marques LS, Batista AE, Falci SG, Ramos-Jorge ML. Urban-rural differences in oral and maxillofacial trauma. Brazilian Oral Research 2012;26(2):132-8. [ Links ]
25. Majambo MH, Sasi RM, Mumena CH, Museminari G, Nzamukosha J, Nzeyimana A, Rutaganda E. Prevalence of oral and maxillofacial injuries among patients managed at a teaching hospital in Rwanda. Rwanda Journal of Health Sciences 2013;2(2):20-4. [ Links ]
26. Asbury, S.L. Patterns of interpersonal violence presenting to a Level One trauma centre in Johannesburg. 2013 (In press). [ Links ]
27. Pham-Dang N, Barthélémy I, Orliaguet T, Artola A, Mondié JM, Dallel R. Etiology, distribution, treatment modalities and complications of maxillofacial fractures. Medicina Oral, Patologia Oral y Cirugia Bucal 2014;19(3):e261. [ Links ]
28. Alves LS, Aragão I, Sousa MJ, Gomes E. Pattern of maxillofacial fractures in severe multiple trauma patients: a 7-year prospective study. Brazilian Dental Journal 2014;25(6):561-4. [ Links ]
29. Olasoji HO, Tahir A, Arotiba GT. Changing picture of facial fractures in northern Nigeria. British Journal of Oral and Maxillofacial Surgery 2002;40(2):140-3. [ Links ]
30. Peltzer K, Davids A, Njuho P. Alcohol use and problem drinking in South Africa: findings from a national population-based survey. African Journal of Psychiatry 2011 ;14(1). [ Links ]
31. World Health Organization, World Health Organization. Management of Substance Abuse Unit. Global Status Report on Alcohol and Health, 2014. World Health Organization; 2014. [ Links ]
32. Mojaki ME, Basu D, Letskokgohka ME, Govender M. Referral steps in district health system are side-stepped. South African Medical Journal 2011;101(2):109. [ Links ]
33. Viera AJ, Garrett JM. Understanding inter-observer agreement: the Kappa statistic. Fam Med. 2005 ;37(5):360-3. [ Links ]
34. Shahim FN, Cameron P, McNeil JJ. Maxillofacial trauma in major trauma patients. Australian Dental Journal 2006;51(3):225-30. [ Links ]
35. Ajike SO, Adebayo ET, Amanyiewe EU, Ononiwu CN. An epidemiologic survey of maxillofacial fractures and concomitant injuries in Kaduna, Nigeria. Nigerian Journal of Surgical Research 2005;7(3):251-5. [ Links ]
36. Garg V, Singh H, Vij K. Trends of maxillofacial trauma at a tertiary care hospital in rural area of Southern Punjab. Journal of Indian Academy of Forensic Medicine 2012;34(1):49-51. [ Links ]
37. Tsakiris P, Cleaton-Jones PE, Lownie MA. Airway status in civilian maxillofacial gunshot injuries in Johannesburg, South Africa. South African Medical Journal 2002;92(10):803-6. [ Links ]
38. Beaumont E, Lownie JF, Cleaton-Jones FE, Neetyon NP. An analysis of fractures of the facial skeleton in three populations in the Johannesburg urban area. Journal of the Dental Association of South Africa 1985;40(11):633. [ Links ]
39. Peltzer K, Ramlagan S. Alcohol use trends in South Africa. Journal of Social Sciences 2009 ;18(1):1-2. [ Links ]
40. Prasad VN, Khanal A. Computed tomography evaluation of maxillofacial injuries. Journal of College of Medical Sciences-Nepal 2017;12(4):131-6. [ Links ]
41. Goel A. Comparative study of clinical manifestation, plain film radiography and computed tomography for diagnosis of maxillofacial trauma. Modern Plastic Surgery 2015;5(04):47. [ Links ]
 Correspondence:
Correspondence:
Dr Lingeswara Pillay:
Zithulele Hospital, Mqanduli, 5080
Cell: 079 143 0669
E-mail: lingeshpillay1@gmail.com














