Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Dental Journal
versión On-line ISSN 0375-1562
versión impresa ISSN 0011-8516
S. Afr. dent. j. vol.73 no.4 Johannesburg may. 2018
DENTAL EDUCATION
Oral hygienists' self-perceivedcompetence on completion of a blended learning course in local anaesthesia at a South African university
Behardien NI; Gordon NII; Rayner CIII; Cupido MIV
IBChD, MSc; Senior lecturer/Stomatologist; Department of Maxillo-Facial and Oral Surgery. Faculty of Dentistry; University of the Western Cape. Tel: +27 21 937 3081 E-mail: nbehardien@uwc.ac.za
IIDipl OH; BA; MPH; Department of Oral Hygiene. Faculty of Dentistry; University of the Western Cape. Tel: +27 21 370 4455. E-mail: ngordon@uwc.ac.za
IIIDip OH; BA (Hons); MA; Department of Oral Hygiene. Faculty of Dentistry; University of the Western Cape. Tel: +27 21 370 4453. E-mail: crayner@uwc.ac.za
IVBChD, PDD; Lecturer/Dentist; Department of Maxillo-Facial and Oral Surgery. Faculty of Dentistry; University of the Western Cape. Tel: +27 21 937 3079. E-mail: macupido@uwc.ac.za
SUMMARY
INTRODUCTION: The expanding scope of practice of oral hygienists require universities to offer courses that would enhance their skills. Aim and objectives: To determine the self-perceived competence of oral hygienists to deliver local anaesthesia (LA) after completion of a blended-learning course.
DESIGN: This was a descriptive, prospective study.
METHODS: Data were collected at two stages, using self-administered questionnaires 1) immediately after the face-to face component of the course and 2) after the final assessment when participants had had the opportunity to deliver LA in their practices. Results and conclusions: All participants (n=25) were female, aged 26-55 years (mean=44 years). The most positive aspects of the course were the engagement with lecturers (90%), accessibility of notes (90%) and video clips (96%). At the end of the face-to-face period, participants (n=25) reported as having the knowledge (100%), skill (76%) and confidence (84%) to administer LA. Results from the second questionnaire (n=19) however, indicated lower scores for the same parameters. This could be explained by limited opportunity to practise LA prior to completion of the second questionnaire. The self-perceived competence of the participants and the practice dynamics appear to be determining factors as to whether LA is employed in their working environments.
INTRODUCTION
In South Africa, the course leading to qualification in the profession of oral hygiene has evolved from a two year diploma, initiated in 1974, to a three year Bachelor's Degree in Oral Health. Concomitantly, the clinical scope of practice was expanded in 20001 and 2013.2 Oral hygienists who wish to practise to the full in these revised scopes are required to attend the relevant courses at accredited universities. On successful completion, their registration is updated with the regulatory body, the Health Professions Council of South Africa (HPCSA), and they may then practise accordingly. In addition to these expanded scopes, independent private practice for oral hygienists was introduced in 2012.3 This allows for the transition of the oral hygiënist from the current legislation of supervised practice, to the independent private practitioner. One requirement for independent private practice is the completion of the 2000 Scope of Practice which includes the administration of local anaesthesia.4 These changes are intended to capacitate the profession with greater autonomy in its role within the broader dental field.
The development of the profession of oral hygiene in South Africa over the past 20 years reflects the maturation of the profession globally.5,7 Continuing education, through short courses, is a feature of all professions in the health sciences.8 The purpose is for practitioners to keep abreast of progress in their fields, and ultimately to provide quality care to patients.5,9-12.
These practitioners re-enter higher education as adult learners. They may have different motivations for returning, and may be at different levels of preparedness for academic study. Adult learners typically require direct connections between their studies and goals.13 However, they are capable of persistent application and independent learning if bolstered by the possibility that their anxiety about success may be addressed by their instructors.13 This challenges universities to use methodologies and technologies to meet the needs of adult learners as well as to satisfy the objectives of the extended education.14
Blended-learning, asateaching and learning methodology, encompasses traditional face-to-face and e-learning by using the advantages of both methods.15 Traditional learning is considered vital in building a sense of community16 and e-learning has the potential to transcend time and space boundaries and to improve convenience and effectiveness for individual and collaborative learning.17 Interactive education, in addition, can enhance participant activity and provide an opportunity to practise skills which could improve professional practice to a greater extent than would didactic sessions.18,19 In supporting adult learning, Mattheos et al. (2010)14 suggest that "interactivity", "flexibility", "continuity" and "relevance to learners' practice" are major characteristics of a successful continuing education programme.
Ultimately the learning programme should ensure that the practitioner is competent with respect to the knowledge, skills, attitudes and values that would enable him/her to improve health outcomes for the patient.20 In assessing competence, objective assessment tools are regarded as the gold standard. Self-perceived competence, however, does provide an indication of the levels of skill and knowledge, together with an assessment of the motivation to maintain and improve those skills.21,6 For this study, self-perceived competence encompasses the dimensions of knowledge of, attitudes to, and skills to perform local anaesthesia.6,21
Including local anaesthesia in the scope of practice of oral hygienists aligns South Africa with international trends.5,6,10,22 The administration of local anaesthetic by oral hygienists was found to be associated with factors such as positive outcomes for their practice, as well as having a high value placed on the procedure5, together with enhanced respect.5,10,23 Hygienists showed confidence in their perceived competence to perform the procedure,6 and this contributed to the manner of delegating tasks in their practice environments.6
In South Africa, short continuing education courses have been offered on the 2000 Scope of Practice1 since 2001. There is, however, no published literature on the perceived competency of oral hygienists after completion of these continuing education courses.
The aim of this study, therefore, was to determine the self-perceived competence of oral hygienists in local anaesthesia after completion of a blended-learning course. The objectives were to determine participants' profile, their concerns prior to starting the course, their experiences of the learning programme, their self-perceived competence to administer local anaesthetic, and the use of local anaesthesia in their practice environments. The results may be used to inform any review of the blended-learning course in local anaesthesia.
MATERIALS AND METHOD
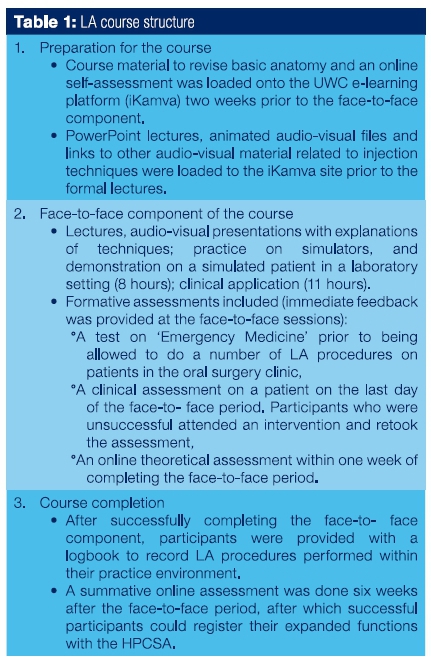
The study was conducted at the Faculty of Dentistry, University of the Western Cape (UWC) between July and September 2016. The study population was a single cohort of oral hygienists attending a continuous education course on the 2000 Scope of Practice1. A blended-learning approach was used. The course structure consisted of: pre-course reading; a one week face-to-face component, and assessments. The local anaesthesia component was embedded within this course (see Table 1).
This was a descriptive, prospective study. The sample comprised participants registered for the course (n=25). Two questionnaires were used, one to evaluate perceptions of the process (Questionnaire 1), and the second, perceptions of the outcome (Questionnaire 2).
The questionnaires consisted of open-ended and closed questions. The first questionnaire was self-administered and was completed on the last day of the face-to-face component. Information related to participant demographics; their views on local anaesthesia being included in the scope of practice; their concerns prior to starting the course and their experiences of the learning programme. Their self-perceived competence to administer local anaesthetic was sought. Participants were asked to respond to statements regarding their experiences of teaching and learning on a three point Likert type data of 'yes', 'no' and 'to some extent'. Their perceived competence was rated on a five point Likert type data ranging from 'definitely', 'yes', 'not sure', 'no', and 'definitely not'. Open-ended questions allowed participants to elaborate on their experiences and perceptions. Completed questionnaires were deposited at a central point to ensure confidentiality and anonymity.
The second questionnaire using Google Forms was made available to participants two months after completion of the face-to-face component. At this time, participants had successfully completed the summative assessment and had had the opportunity to administer local anaesthetics in their practices. Questions enquired about the administering of local anaesthesia in their work environments, their perceived competence in the techniques, and their perception of the value of local anaesthesia in their practice environments. The same five point Likert type data was used in the closed questions.
Ethics approval was obtained (Humanities and Social Sciences Research Ethics Committee: reg. HS/16/8/14). At the introduction of the local anaesthesia component of the course, participants were informed of the related research project. They were informed of the purpose of the study and that their feedback would inform the review of the module. They were informed that participation was optional, and that their responses (should they participate) would be anonymous and confidential. They were also informed that they could withdraw from the study at any point, without being disadvantaged.
The First Questionnaire was completed on the last day of the local anaesthesia contact session. Study information and consent letters were attached to the questionnaires and distributed to the oral hygienists. Those participating could complete these questionnaires in their own time and deposit the completed documents and consent forms in depositories placed in designated areas. In the Second Questionnaire, Google Forms was set up with an information letter and a tick box for consent. Participants who chose to participate were directed to the questionnaire which was also made available by email (with a return email address of an independent recipient to ensure anonymity).
Data were entered and analysed using the STATA/ IC12. Open-ended questions were themed and coded. Frequency distributions were generated. The Spearman's correlation coefficient was used to determine the strength of the relationship between variables. Statistical significance was set at p<0.05.
RESULTS
Demographics
The results below relate to the process indicators (Questionnaire 1)
Participant profile and concerns prior to the face-to-face period.
Participant profile
The response rate was 100%. All participants were female, aged between 26 and 55 years (mean=44; SD 6.9). English was the first language of 16.7%, second language of 70.8% and third language of 12.5% of participants. Twenty-four participants had a Diploma in Oral Health obtained between 1980 and 2002, while one participant had a Degree in Oral Health. Areas of employment Included general practice (68%), specialist practice (16%), public health sector (8%) and 'other' (4%). Experience in Information Technology included the use of the internet (96%), email (80%) and Facebook (37%).
Results of Questionnaire 1
Participant concerns
Concerns specific to the administering of local anaesthetic ranged from: inability to identify anatomical landmarks, mastering the skill of intra-oral injections, and injuring the patient. Concerns around learning were the ability to cope with the academic aspect of the module, anxiety about studying after a long break, and coping with the English medium. Concerns expressed as 'fear', 'anxiety' and being 'overwhelmed' were noted in the following statements. "Scared of injecting a person in the wrong place, causing permanent damage"; "Nervous whether I would cope with the anatomy, will I be able to admin (sic) LA". Participants also reported that patients may be sceptical of the ability of the oral hygiënist to administer local anaesthetic; that time would be required to allow development of confidence to do the procedure; and that the dentist may not be available to render the necessary support.
Participant engagement with and experience of the learning programme
A large number of participants (>90%) found the pre-course reading, feedback sessions and video clips useful In developing competence. Participants elaborated on positive experiences (Table 2) such as lecturer availability, expertise, and interest in teaching students, noted by comments such as, "I feel very confident administering local anaesthesia", "The lecturers put it across beautifully and they were very accommodating and patient with all the students". Negative experiences ("no", "to some extent" responses in Table 2) included insufficient time and opportunity to practise the skill, and a lack of Integrating theory with practice. These were noted by comments such as "I am feeling more confident, but think more clinical practice is necessary".
In response to the question on how their concerns prior to the commencement of the course were addressed, three themes emerged. These were:
1. The organisation and planning;
2. The teaching staff; and
3. The teaching format.
Participants elaborated on the above with reference to the availability of study material; having excellent, knowledgeable and patient teachers; and a format of explanations followed by demonstrations. Their views were highlighted by the following comments: "Tell-show-do method was very effective in helping me understand and implement practices"; "adequate information was given, techniques explained very well and my fear dispelled"; "With all the lectures it all made sense"; "The practical made sense and helped with theory".
Participants' views on the teaching methods
The most useful methods were the face-to-face teaching In the classroom and in the clinical environment; the sequencing of lectures followed by practical application in the clinics; the use of video clips and; access to video clips in their own time. The different teaching and learning formats reinforced and consolidated important concepts pertaining to local anaesthesia. Lecturer interest in student learning, excellence in presentation and patience was emphasized with comments, such as, "Practical and videos together with understanding the anatomy (sic)"; "Teaching in classes made it personal and could elaborate on points that we did not understand"; "very nice teachers"; "made the global picture to a more understanding level, great".
The least useful teaching method was the simulated local anaesthesia model, consisting of battery operated jaws with 11 anaesthetic contact sensor points. Being orientated to injection techniques on a colleague, compared with practicing on the simulated local anaesthesia model, was reported to be more useful in developing skills and confidence to inject a patient.
Views on the inclusion of local anaesthesia within their scope of practice
All participants responded positively to the inclusion of local anaesthesia within the scope of practice of the profession. They noted an increased autonomy for the profession, greater independence in patient management, the provision of more comprehensive patient care,
improved patient comfort, and an improved efficiency in patient flow as noted by the following comments: "Expand our boundaries and make it easier to apply our knowledge and to be of great help in the practice"; "It is fantastic broadening our scope in these areas"; "Will only empower us".
Self-perceived competence to administer local anaesthesia
At the time that the questionnaire was administered, all participants had successfully completed the formative aspect of the assessment. The scales of 'no' and 'definitely not' were excluded as there were no reported values for these scales. All (100%) responded to having the knowledge and felt it important to have the right and competence to administer local anaesthesia (Table 3).
Perceived knowledge, competence and skills in local anaesthesia (Table 3: statements1-3) were used as a measure for self-perceived competence. The composite of self-perceived competence showed a very strong" correlation between local anaesthesia clinical skills (rs=0.919, p=0.0005) and local anaesthesia confidence (rs=0.911, p=0.0005); and a "strong" correlation between local anaesthesia skills and LA knowledge (rs=0.768, p=0.0005). A "very weak" (rs=0.00-0.19) relationship between most of the experiences of participants (Statements 1-9) of the learning programme and their perceived competence, with the exception of 'engagement with lecturers' (Statements 10,11,12) which was found to be "weak" (rs=0.20-0.39). Participants' self-confidence as a component of their self-perceived competence was "moderately" (rs=0.40-0.59) associated with 'engagement with lecturers'.
QUESTIONNAIRE 2
Practices and perceptions of local anaesthesia Administering of local anaesthesia in practice environment (n=19).
The response rate to the second questionnaire was 76% (n=19). Eighty-four percent (84%; n=16) reported that they administered local anaesthetic in their work environment. Participants reported that they used local anaesthesia for deep scaling and root planing (75%), restorative procedures (25%), management of tooth sensitivity (19%), removal of splints (6%) and orthodontic debanding (6%). The most common injection technique used was mandibular infiltration (n=16) followed by maxillary infiltration (n=13) and the mandibular block (n=11). None of the participants reported unsuccessful outcomes in the administration of local anaesthetic.
Perceived competence to administer local anaesthesia 'Responses of 'yes' and 'definitely' were combined. Participants' perceptions of their competence were lower after having had the opportunity to work in practice after the face-to-face period. However, the data was not matched for the two questionnaires and therefore statistical analysis was not performed. The view that administering of local anaesthetic added value to their work environment and that there was a need for oral hygienists to administer it, was not shared by all participants.
Barriers and facilitating factors to performing local anaesthesia in the work environment
Barriers
Participants who perceived that they lacked experience and the practical skills to perform local anaesthesia, and who perceived a lack of confidence of their role in their practice, reported to administer local anaesthetic to a limited extent or not at all. They elaborated that having the theoretical knowledge did not translate to their ability to perform local anaesthesia in practice and that confidence and competence improved with time expressed by comments such as "more practical sessions would have built this"; "Neither myself, nor my employer feel I am sufficiently experienced to start doing these procedures in practice"; "Orthodontist not open to me infiltrating".
Facilitating factors
Participants who felt supported and were clear about their role in their work environment, appear to do the procedure even when they did not feel fully confident, highlighted in the following comments "Patients depend on you and this builds more trust"; "The need to ease discomfort and sensitivity is very important so that I can offer a thorough treatment to patients"; "Freedom to administer LA with confidence without having to interrupt the dentist"; "I am very nervous when I do it, but I try my best"; "I'm confident as OH because I put a lot of value in our practice"; "Not dependent on waiting for the dentist".
DISCUSSION
Profile of participants
The participant profile affirms an interest by this group of oral hygienists, as one of the health services professions, to maintain and improve their competence over "lengthy careers and diverse practice areas"24 Ryan (2003),8 reported that the top motivators for engaging in continuing education by health services professionals were: developing professional knowledge, updating existing qualifications, increasing the status of the profession and demonstrating professional competence. Participants viewed the inclusion of local anaesthesia in the scope of the profession as "empowering, expanding boundaries and helping the practice" shows that attendance at the course is also seen as part of the development of their profession rather than a narrow focus on procedures. There may be other factors, such as the multiple life roles that they occupy as women,13 increased remuneration, and the fact that completion of the 2000 Expanded Scope1 is a prerequisite for independent private practice.
Experience of the learning programme Participants' experience of the blended-learning programme, generally, was positive. Their access to resources and skills to engage in this approach may have been contributed to this. These factors should be taken into account by course developers when using a blended-learning approach. Participants' pre-course concerns, to a large extent, were addressed through the quality of organisational, teaching, and teacher inputs, highlighting the views by Mattheos et al. (2010)14 on the characteristics of a successful continuous education course. Personal, relational and organisational factors to support good clinical learning experiences were also reported by nursing students26.
Although simulators have numerous benefits, ranging from use on demand; prevention of unethical or unnecessary practice on patients and honing of skills in a risk free environment,26 the participants of this course found the 'conduction anaesthesia model' to be of limited value. This could possibly be because the training model does not resemble the human mouth accurately enough or that the instruction in the use of the simulator was not structured within a framework as suggested by Kneebone (2005).27 The interactive nature and hands-on approach used in this course appeared to be appreciated by this cohort of adult learners. This may indicate that these adult learners, who re-entered higher education many years after acquiring their qualifications, may view technology less favourably.27
The views of participants in this course highlighted the advantages of using a blended-learning approach combined with an interactive clinical component. Participants stressed that they were welcomed into the dental environment and that they had access to course material in their own time.
Perceived competence of participants Participants responded positively to the availability of course material, yet there was a weak relationship between their self-perceived competence on completion of the face-to-face component and their engagement with material. The relationship between feedback and engagement with lecturers is moderate to weak. These results suggest that although participants may find the study programme positive, their self-perceived competence is influenced primarily by their engagement with lecturers through feedback and clarification of questions. Formative assessment with immediate feedback was done at different stages of the learning programme. The value of feedback in ensuring credibility and effectiveness of the learning process was also highlighted by Mattheos et al. (2010).14
Participants' self-perceived competence was "very strongly" correlated with their self-perceived confidence and clinical skills and "strongly" correlated with their self-perceived knowledge at the end of the face-to-face component. Although all participants had successfully completed the formative assessment at that time, and were considered competent to perform the procedure under supervision of the dentist, not all participants felt that they were competent. All participants indicated that they had the knowledge to perform local anaesthesia, but approximately one quarter did not perceive that they had the skill to do so (Table 3). This was emphasised in the open-ended questions by the comments of participants regarding the requirement of more clinical time, and, that knowledge does not necessarily translate to skills. An assumption of the learning programme was that, prior to their doing the summative assessment, participants would have the opportunity to perform local anaesthesia in their practice environments under supervision of the dentist, and in so doing, improve their clinical skills. The results show that such a process may have to be formalised in further continuing education courses offered by the university.
The use of local anaesthesia in their practice environments. The views of the participants that oral hygienists should be able to perform local anaesthesia are consistent with those expressed in the international literature.5 In rating their competence at the end of the course, most of the group of oral hygienists (84%) considered they had the knowledge to perform local anaesthesia, yet only 60% reported as being confident they had the skill. These perceptions may indicate that it takes time to develop mastery of this clinical technique.27 A concern for the professional development of these participants is that self-perceived competence is an indication of the motivation to maintain and improve skills,6,21
Although the literature confirms it has been shown that oral hygienists can perform this procedure safely,5,10,22 concerns expressed by participants and by their dentists as employers regarding patient safety are valid. Those universities providing further education for Oral Hygienists may need to consider the option of engaging the employer dentist in the courses.
The frequency of local anaesthetic being administered by oral hygienists varied by practicetype, with local anaesthesia being more frequently provided in specialist periodontal practices than in general practices.5,10 Oral hygienists who completed a continuing education course reported that more than 90% of dentists delegated this procedure to them. Eighty-eight percent (88%) were administering local anaesthetic within one month of completion of the course and used the procedure primarily for root planing and debridement, and where tooth sensitivity was anticipated 10 as is also reported in this study. Although the literature indicates that dental hygienists have been shown to perform this procedure safely,5,10,22 concerns regarding patient safety were expressed by this cohort and their employers. This may have contributed negatively to their perceived competence,10 as also reported in this study.
More than half of the oral hygienists who completed a continuing education course found; local anaesthesia to be very valuable to their practice; that employers and patients appreciated their skill, that more comfortable treatment could be provided; and that their practices ran more efficiently.10 This study indicated that providing the participant the confidence and capacity to perform local anaesthesia in the practices setting, independent of the dentist, increased their work satisfaction, built patient trust, contributed to reduction of patient discomfort, and allowed treatment to be completed without the need to disturb the dentist.
Suggestions for the review of this course.
Course developers should consider several concerns prior to delivery of the course. Requests by the oral hygienists for more clinical exposure during the face-to-face component and the dynamics within their own work environments should be taken into account in any review of this course. As continuing education is most often offered as short courses, it may not be possible to increase the practical time significantly during the face-to-face period. It is well documented that all learning cannot take place in the formal didactic environment, and course developers should investigate practical ways in which learning can be extended into the work environment by engaging employers.28 The necessary conditions are already prescribed by the HPCSA (Board for Dental Assisting, Dental Therapy and Oral Hygiene). Such collaboration may address concerns of professional boundaries as well as to focus on how patient outcomes can be improved. This notion creates an added role for the university in advocating a dental team approach in practice, with a focus on professional development and improved patient outcomes.
A limitation of the course was that the process of facilitating the entry of participants into the work environment was not done. Continuing education involving clinical skills could potentially influence the workings of a dental practice.
Limitation of the study
The results should be viewed against the following: the size of the sample; the fact that the process and outcome questionnaires were not paired and thus could not be compared; and, the low response rate to the second questionnaire. The results of this study cannot be generalised to continuing education courses on expanded functions for oral hygienists or for continuing education courses in general.
CONCLUSION
The results clearly show that the blended-learning approach was successful in developing participants' knowledge and skill to administer local anaesthesia. In spite of successful completion of the course, their self-perceived competence and work environment dynamics were determining factors to whether or not they would actually perform the procedure in practice. These factors should be taken into account when developing continuing education courses. Course developers should consider means of mediating with employers to enable the integration of oral hygienists with expanded functions into the practice environment. If not, the goals of professional development and improved patient care may not be met.
ACRONYMS
HPCSA: Health Professions Council of South Africa. LA: Local Anaesthesia.
References
1. South Africa. Government Gazette. Dept. of Health. Regulations defining the scope of the profession of oral hygiene. October 2013. Vol 580. No 36944. Available: https://search.opengazettes.org.za/text/9617?dq=21736&page=1 [Accessed 2018-03-19] [ Links ]
2. South Africa. Government Gazette. Department of Basic Education. The South African Schools Act, 1996. November 2015. Vol. 605. No 39406. p. 1-12. Available: http://www.greengazette.co.za/pages/national-gazette-37230-of-17-january-2014-vol-583_20140117-GGN-37230-003 [Accessed 2018-03-08] [ Links ]
3. South Africa. Government Gazette. Regulations Gazette No. 35200. March 2012. Vol. 561. No 9726. Available: https://www.greengazette.co.za/documents/regulation-gazette-35200-of-30-march-2012-vol-561-no-9726_20120330-GGR-35200.pdf [Accessed 2018-03-08] [ Links ]
4. South Africa. Government Gazette. Health Professions Act, 1974. Regulations relating to the scope of practice of the profession of Oral Hygiene. Part 1 OF 3. July 2017 [cited 2018 Mar 19]; 625(40996):1-776. Available: https://archive.opengazettes.org.za/archive/ZA/2017/government-gazette-ZA-vol-625-no-40996-dated-2017-07-21.pdf [Accessed 2018-03-19] [ Links ]
5. Boynes SG, Zovko J, Bastin MR, Grillo Μ A, Shingledecker BD. Dental hygienists' evaluation of local anesthesia education and administration in the United States. J Dent Hyg. 2011; 85(1):67-74. [ Links ]
6. Virtanen Jl, Tseveenjav B, Wang NJ, Widström Ε. Nordic dental hygienists' willingness to perform new treatment measures: Barriers and facilitators they encounter. Scand J Caring Scl. 2011; 25(2):311-6. [ Links ]
7. Gatermann-Strobel B, Perno Goldie M. Independent dental hygiene practice worldwide: A report of two meetings. Int J Dent Hyg. 2005; 3(3):145-54. [ Links ]
8. Ryan J. Continuous professional development along the continuum of lifelong learning. Nurse Educ Today. 2003; 23(7):498-508. [ Links ]
9. Carroll C, Booth A, Papaloannou D, Sutton A, Wong R. UK Healthcare professionals' experience of on-line learning techniques: A systematic review of qualitative data. J Contin Educ Health Prof. 2009; 29(4):235-41. [ Links ]
10. Anderson JM. Use of local anesthesia by dental hygienists who completed a Minnesota CE course. J Dent Hyg. 2002 [cited 2018 Mar 19]; 76(1):35-46. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11935929 [ Links ]
11. Bennett S, Bennett JW. The process of evidence-based practice In occupational therapy: Informing clinical decisions. Aust Occup Ther J. 2000; 47(4):171-80. [ Links ]
12. Towle A. Changes in health care and continuing medical education for the 21st century. BMJ. 1998; 316(7127):301-4. [ Links ]
13. Williamson MM, Greenwood CM. The Non-traditional student of the 1990: Adults re-entering college. 2018; 5(2):69-79. [ Links ]
14. Mattheos Ν, Schoonhelm-Klein Μ, Walmsley AD, Chappie ILC. Innovative educational methods and technologies applicable to continuing professional development in perlodontology. Eur J Dent Educ [Internet]. 2010 May 1 [cited 2017 Dec 3]; 14(SUPPL. 1):43-52. Available from: http://doi.wiley.eom/10.1111/j.1600-0579.2010.00624 [ Links ]
15. Liu Q, Peng W, Zhang F, Hu R, Li Y, Yan W. The Effectiveness of Blended Learning in Health Professions: systematic review and meta-analysis. J Med Internet Res. 2016; 18(1) [ Links ]
16. Kemp N, Grieve R. Face-to-face or face-to-screen? Undergraduates' opinions and test performance in classroom vs. online learning. Front Psychol. 2014; 5(NOV):1-11. [ Links ]
17. Moreira IC, Ventura SR, Ramos I, Rodrigues PP. Development and assessment of an e-learnlng course on breast imaging for radiographers: a stratified randomized controlled trial. J Med Internet Res [Internet]. 2015 Jan 5 [cited 2018 Mar 19]; 17(1):e3. Available from: http://www.ncbl.nlm.nih.gov/pubmed/25560547 [ Links ]
18. Davis D, Davis N. Selecting educational interventions for knowledge translation. CMAJ. 2010; 182(2):89-93. [ Links ]
19. Young Linda J (School of Dentistry, University of Minnesota, Minneapolis) Newell Kathleen J (School of dentistry, University of Minnesota M. Can a clinical continuing education course change behavior In dental hygiene practice? Am Dent Hyg Assoc [Internet]. 2008; 82(4):1-10. Available from: http://jdh.adha.Org/content/82/4/33.short%0Ahttp://jdh.adha.o rg/content/85/3/211.short [ Links ]
20. Frank JR, Snell LS, Cate 0 Ten, Holmboe ES, Carraccio C, Swing SR, et al. Competency-based medical education: Theory to practice. Med Teach. 2010; 32(8):638-45. [ Links ]
21. Lai NM, Teng CL. Self-perceived competence correlates poorly with objectively measured competence in Evidence Based Medicine among medical students. BMC Med Educ. 2011; 11(1). [ Links ]
22. Brand HS, Bekker W, Baart JA. Complications of local anaesthesia. An observational study. Int J Dent Hyg. 2009; 7(4):270-2. [ Links ]
23. DeAngelis S, Goral V. Utilization of local anesthesia by Arkansas dental hygienists, and dentists' delegation/satisfaction relative to this function. J Dent Hyg [Internet]. 2000 [cited 2018 Mar 19]; 74(3):196-204. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11314639 [ Links ]
24. Lundgren BS, Houseman CA. Continuing competence in selected health care professions. J Allied Health. 2002; 31(4):232-40. [ Links ]
25. Dale B, Leland A, Dale JG. What factors facilitate good learning experiences in clinical studies in nursing: Bachelor students' perceptions. ISRN Nurs [Internet]. 2013; 2013:1-7. Available from: http://www.hlndawi.com/journals/isrn/2013/628679/ [ Links ]
26. Scalese RJ, Obeso VT, Issenberg SB. Simulation technology for skills training and competency assessment In medical education. J Gen Intern Med. 2008; 23(1 SUPPL): 46-9. [ Links ]
27. Kneebone R. Evaluating Clinical Simulations for Learning. Acad Med. 2005; 80(6):549-53. [ Links ] "
28. Cameron S, Rutherford I, Mountain K. Debating the use of work-based learning and inter-professional education in promoting collaborative practice In primary care: a discussion paper. Quality in Primary Care.2012; 20: 211-17 [ Links ]
 Correspondence:
Correspondence:
Dr Nashreen Behardien
Department of Maxillo-Facial and Oral Surgery
Faculty of Dentistry, University of the Western Cape
Private Bag X1, Tygerberg, 7530 South Africa
Tel: +27 21 788 2991
Fax: +27 21 788 8802
E-mail: nbehardien@uwc.ac.za














