Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Dental Journal
versión On-line ISSN 0375-1562
versión impresa ISSN 0011-8516
S. Afr. dent. j. vol.73 no.4 Johannesburg may. 2018
RADIOLOGY
The assessment of osseous changes in the temporomandibular joint using Cone Beam Computed Tomography
Shaik SI; Parker MEII
IPDD, MSc (MFR) (UWC), Department of Diagnostics and Radiology, Oral Health Centre, University of the Western Cape, Tygerberg Campus, Francie Van Zyl Street, Tygerberg, 7505, Cape Town, South Africa
IIBChD (UWC), MDent (RAD) (London) Department of Oral and Maxillofacial Radiology, Oral Hearth Centre, University of the Western Cape, Tygerberg Campus, Francie Van Zyl Street, Tygerberg, 7505, Cape Town, South Africa
ABSTRACT
INTRODUCTION: Clicking of the temporomandibular joint (TMJ) is not a normal occurrence. The clinical finding of chronic clicking of the joint can signify osseous changes and early signs of degenerative joint diseases.
AIM: To compare osseous changes seen in the mandibular condyles of patients presenting at the Oral Health Centre, Tygerberg Campus, with and without clicking of the temporomandibular joint.
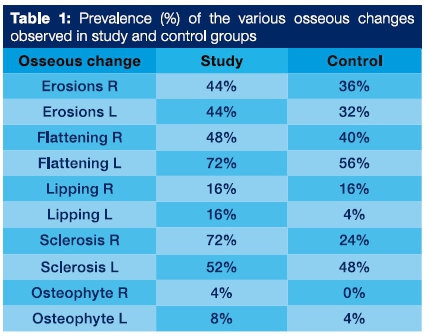
METHODS: From amongst patients routinely attending the Oral Health Centre, a sample of 25 were selected as presenting with asymptomatic clicking of the temporomandibular joints. A matched sample of patients who did not demonstrate clicking was collected as a control. The mandibular condyles of both groups (N=100) were examined for erosions, flattening, lipping, sclerosis and osteophyte formation.
RESULTS: The prevalence of sclerosis of the right joint in the study group was statistically significantly higher in comparison with the control group (P = 0.002). Age and gender showed no statistical significance between the two groups.
CONCLUSION: Osseous changes were found in both the control and study groups but were more consistently found amongst those having asymptomatic clicks of the temporomandibular joints.
Key words: Cone Beam Computher Tomography, TMJ, TMD, Clicking, degenerative joint disease
INTRODUCTION
There is a misconception amongst patients and practitioners that clicking of the temporomandibular joint (TMJ) on opening and/or closing does not warrant treatment unless there is associated pain. A click is however a clinical manifestation of disorders of the TMJ known as internal derangement - which relate to abnormal positional relationships between the mandibular condyle, the articular eminence and the articular disc that separates them. The important consideration is that chronic derangement of the joint frequently results in osteoarthritis.1
A click can present at almost any stage during normal motion and function of the TMJ and can vary in audibility and severity.2 The associated derangement can displace the articular disc in anterior, posterior, medial or lateral directions. When the displaced disc returns to its proper position, force may be exerted on the osseous structures of the TMJ resulting in compensatory or abnormal response.3 There is a possibility that a disorder of the TMJ, which is a chronic process, can result in disease progression if left untreated. The importance of diagnosing the early stages of derangement and treating the signs and symptoms could prevent or reduce the chances of degenerative joint diseases like osteoarthritis.4
The presence of erosions, sclerosis lipping, osteophyte formation and flattening of the condyle are indicative of an active degenerative procedure and their recognition is possibly diagnostic of the risk of future disease.1,4
MATERIALS AND METHODS
The study group comprised 25 patients (50 joints) who presented for routine dental treatment and, on examination, had demonstrated asymptomatic clicking of the TMJ. These patients consented to CBCT examination and were then referred to the TMJ clinic. The control group comprised 25 patients (50 joints) whose records were drawn from the files and who had been evaluated for treatment other than for temporomandibular joint disorders (TMD). The control group was contacted telephonically to confirm they presented no symptoms and were made aware of their records being used anonymously. Study group patients were exposed to low dose, high resolution cone beam computed tomography using a Newtom® VGI CBCT machine. Similar radiographs were available in the files of the patients in the control group. Three dimensional reconstructions of the condyles were made to allow full examination of the shapes of both the right and left condyles. Hence, 100 joints were examined. Osseous changes of the condyles that were recorded included: erosions, flattening, lipping, sclerosis and osteophyte formation. The patient's gender and age were recorded to allow for correlation with the findings. P-values were obtained using Chi-squared test applied to a cross tabulation for each variable by group.
RESULTS
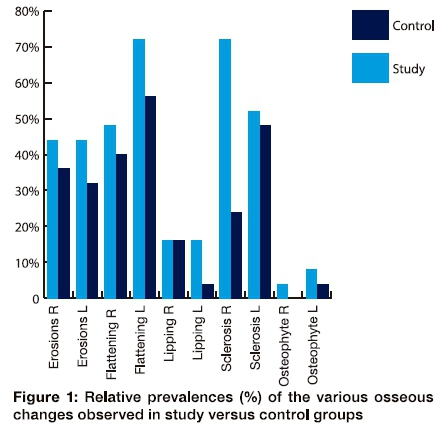
The mean age for the control group was 35.04 years and for the study group, 30.64 years. Neither age nor gender demonstrated any statistically significant significances in analysis. The relative prevalence of each of the variables examined are presented in Table 1, and graphically in Figure 1. In every instance except lipping, which showed equal findings for the right condyles, the study group recorded higher figures. However statistically significant differences were demonstrated only in the variable of sclerosis affecting the right condyles (p= 0.002).
DISCUSSION
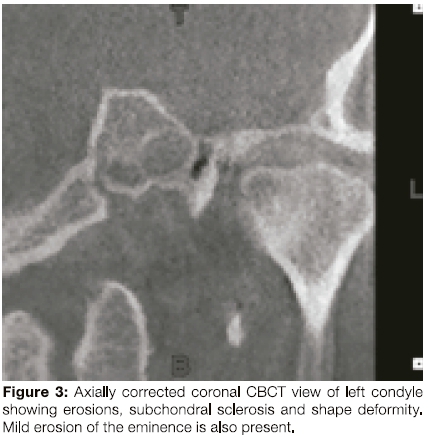
Osseous changes were observed in both the study and the control groups. In general, the study group demonstrated more evident changes with erosions (44%-32%), flattening (72%-40%) and sclerosis (72%-24%) being the more common findings. Lipping was relatively uncommon (16%-4%) and osteophyte formation (8-0%) was the least frequently occurring change seen. These data confirm previous notions that normal physiological wear of the joint may result in some osseous changes of the condyles in middle to older age group patients having asymptomatic joints.5 Some of these may be associated with osteoarthritis such as erosions, lipping subchondral cyst and osteophyte formation (Figures 2,3,4). Erosion of the condyle is the earliest manifestation of degenerative changes.


CONCLUSION
Osseous changes of the condyles were found in both the study and control groups. Almost every characteristic, except lipping, showed a higher prevalence amongst the study group. A prolonged clicking of the TMJ warrants a clinical examination and an adequate radiographic examination preferably with CBCT, If available.
ACRONYMS
TMJ: Temporomandibular Joint
TMD: Temporomandibular Joint Disorders
CBCT: Cone Beam Computed Tomography
References
1. BarghanS.TetradisS, Mallya SM. Application of cone beam computed tomography for assessment of the temporomandibular joints. Aust Dent J, 2012;57(1):109-18. [ Links ]
2. Badel T, Maritti M, Simunkovic SK, Keros J, Kern J, Krolo I. Radiological characteristics of osteoarthritis of temporomandibular joint without disc displacement. Periodicum Biologorum,2009;111(2):289-92. [ Links ]
3. Aly N, Hashim H, Saleh H, Abdullah D. Pilot study of the osseous morphological changes in the temporomandibular joint in subjects with bilateral missing lower posterior teeth. Inter J Sei Eng Res, 2011;2(11):1-23. [ Links ]
4. Mupparapu M, Chow I, Uppal A. Hard tissue structural changes in TMJ morphology prior to orthodontic therapy: A complex motion tomographic study. Quint Inter, 2011; 42:427-34. [ Links ]
5. Ahmad M, Hollender L, Andersen Q, Kartha K, Ohrbach R, Edmond T, John MT, Schiffman EL. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Path Oral Radiol Endod, 2009; 107(6): 844-60. [ Links ]
 Correspondence
Correspondence
Dr Shoayeb Shaik
Department of Diagnostics and Radiology, Tygerberg Campus
Francie Van Zyl street, Tygerberg, 7505
Cape Town, South Africa
tel: +27219373110
sshaik@uwc.ac.za














