Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.73 no.3 Johannesburg Abr. 2018
RESEARCH
Epidemiology of maxillofacial fractures at two maxillofacial units in South Africa
BM MogajaneI; M MabongoII
IBrampie M Mogajane: BDS, MSc Dent ( MFOS ). Department of Maxillofacial and Oral Surgery, University of Witwatersrand, Johannesburg, South Africa
IIMzubanzi Mabongo: BDS, MChD, FCFS. Head of Clinic Unit, Department of Maxillofacial and Oral Surgery, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
AIM: To compare epidemiologic characteristics of maxillofacial fractures seen in patients presenting at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) with those seen at Polokwane -Mankweng Hospital Complex (PMHC).
OBJECTIVE:To compare the patterns; aetiology and incidence of maxillofacial fractures between the two units.
MATERIALS AND METHODS: Cross sectional study of 194 patients with 226 maxillofacial fractures reported and treated at either CMJAH or PMHC between December 2013 and August 2014. Variables recorded include: age; sex; socioeconomic status; population group; aetiology; time of injury; identity of assailant (if known), the site of the fracture and associated injuries.
RESULTS: Of the total number of patients (194), 82% were male. The majority (75%) were in the age group of 20-39 years with a peak frequency in the 3rd decade. Assaults were by far the leading cause of maxillofacial fractures (60.3%), followed by road traffic accidents accounting for 17.5%. Most (65.5%) were sustained at night. The mandible was the most frequently fractured facial bone (73.0%), followed by the zygoma.
CONCLUSION: Interpersonal violence is by far the leading cause of maxillofacial fractures in both units. The general pattern of maxillofacial fractures was the same in both settings, and the differences in numbers reflect the relative population sizes.
INTRODUCTION
Maxillofacial fractures are frequently encountered because of the prominence and accessibility of the face in situations of violence.1 In almost all instances of this mishap, the attention of maxillofacial surgeons is sought.2,3 The global incidence of maxillofacial fractures is related to a variety of factors such as sex, age, level of industrialisation, socioeconomic status, geographical location and seasonal variations.4,5 Several studies have reported the peak age for the incidence of maxillofacial fractures to be 20-39 years.1,6-,8 whilst others found the peak age to be in the fourth decade of life.2 There are numbers of reports in the literature regarding multi-system trauma and facial fractures.2 Injuries to other parts of the head are commonly associated with facial fractures, which can also be markers for brain injury. A survey conducted in Kaduna, Nigeria, by Ajike et al. (2005) found an 8,5% concomitance of head injuries and that of these, orthopaedic injuries accounted for the majority (67.10%).2
The reported causes of maxillofacial trauma include assaults, motor vehicle accidents, falls, gunshot wounds, sport related injuries, industrial injuries and animal attacks.3 Interpersonal violence is the most common cause of maxillofacial injuries, and there is a decrease in injuries caused by motor vehicle accidents.3,10 However, studies on paediatric maxillofacial trauma report falls as the most common cause of maxillofacial injuries.11-13. In contrast Van As et al.14 reported that falls accounted for 19% of facial fractures of 107 children treated at the trauma unit, an incidence closely equal to the 22.3% reported by Ajike et al.2 Aetiologic factors may differ within the same country. Boffano et al. showed that in Oslo (Norway) assault-related maxillofacial fractures were the most common while in Bergen (Norway) they were the least frequent.1
Most studies showed that maxillofacial fractures are more common in males than in females.1,3,6,8 The highest reported male-to-female ratio is 6:18 while the is lowest 1,6:1.15 Women in developed countries participate directly in social activities and are thus more susceptible to traffic accidents and urban violence.16-18Facial injury rates in these women are more common than those in developing countries, showing that certain socioeconomic conditions contribute to a high rate of maxillofacial fractures.15,16,18,19
International trends show that mandible is the most commonly affected facial bone,2,6,11,20 although a Portuguese study found the naso-orbito-ethmoid complex to be the most affected region (67.46%) followed by the maxilla (57.42%).21 These findings are, however, in contrast with those reported by Gupta et al. who recorded the zygoma as the most affected maxillofacial bone, followed by the mandible.7 Schneider et al. agreed that zygomatic fractures were the most common, with orbital and mandibular fractures occurring less frequently.9 The mandible was identified by Bofano et al. as heading the list, with condylar, then angle and body fractures being found in deceasing frequency.1 The site of mandibular fracture is related to the different aetiological agents responsible for causing the fractures. Violence accounts for mainly body and angle fractures, whereas motor vehicle accidents incur mostly symphyseal and parasymphyseal fractures.21,22
There have been a number of epidemiological studies of maxillofacial fractures, mostly completed in metropolitan cities of South Africa,8,10,11,22 but no similar studies have been conducted in the rural provinces. The aim of this study is to analyse and compare the epidemiologic characteristics of maxillofacial fractures amongst affected patients presenting at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH), which is in Johannesburg, compared with those presenting at Polokwane-Mankweng Hospital Complex (PMHC), which is in the mainly rural province of Limpopo.
MATERIAL AND METHODS
This is a cross-sectional study of patients who presented with maxillofacial fractures to the Maxillofacial Units of CMJAH and of PMHC. The study was conducted from December 2013 to August 2014. In both units the patients were assessed clinically and radiographically by consultants. Variables recorded on the data collection sheet were: age; gender; socioeconomic status (i.e. employed or unemployed); population group; cause of trauma; time of injury, identity of assailant (if known) and relationship with the patient. The anatomic sites of the fractures and associated injuries were recorded. Patients were not included in the study if they were not willing to participate, presented with maxillofacial fractures secondary to pathological lesions or had isolated soft tissue injuries.
Data was analysed with Statistica (version 12.5). Frequencies and percentages were used to describe categorical variables while continuous variables are presented as means and standard deviations. The Student t-test was used to assess any differences between means. Differences in proportions and relationships between categorical variables were assessed using the Chi-squared test. The significance level of the tests was a p-value less than 0.05.
Ethical clearance (M130842) for this cross sectional study was obtained from the Human Research Ethics Committees (Medical) of both the University of the Witwatersrand and the University of Limpopo, Polokwane Campus. Informed consent was obtained from each patient for their inclusion in the study.
RESULTS
Demographic data
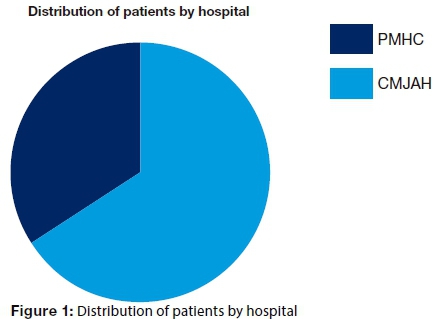
In a period of nine (9) months, data from a total of 194 patients with 226 fractures from both units were recorded and analysed. Of these patients, 128 (66.0 %) patients with 155 (68.6%) fractures were from CMJAH and 66 (34.0%) patients with 71(31.4%) fractures were from PMHC (Fig 1).
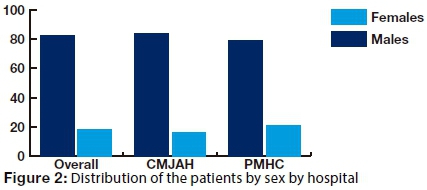
One hundred and fifty nine (82.0%) patients were males and 35 (18.0%) were females, giving an overall male to female ratio of 4.5:1. Of the 159 male patients, 107 (67.3%) were from CMJAH, and 52 (32.7%) were from PMHC, constituting 78.8% of patients from that unit. Thirty five patients were females, twenty one (60%) of these patients being from CMJAH, comprising16.4% of patients and 14(40.0%) were from PMHC, contributing 21.2% of patients. There was no significant difference (P=0.410) in proportions of the female patients between the two units (Fig 2).
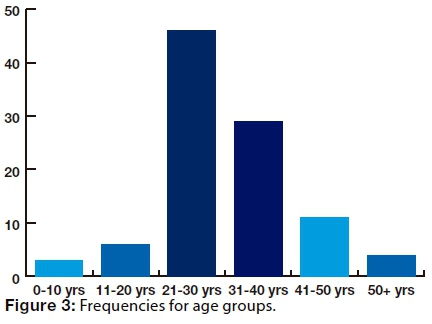
The minimum age was two years and the maximum age was 61 years. In both males (82%) and females (18%), the majority (75%) of patients were in the age group of 20-39 years with a peak frequency in the 3rd decade (Figure 3). The overall mean age was 30.6 (SD 10.02) years.
EMPLOYMENT STATUS
Overall, 84(43.3%) patients were employed and 110(56.7%) were unemployed. In the CMJAH sample, 57 (44.8%) patients were employed and 70(55.2%) patients were unemployed. In the sample from PMHC, 27(40.0%) patients were employed and 40(60.0%) patients were unemployed, with the unemployment rate being higher than overall rate. This rate, however, was not statistically significant (p=0.6790).
TIME OF INJURY.
One hundred and twenty seven (65,5%) patients sustained injuries during the night, while 66 (34.0%) patients suffered maxillofacial fractures during the day. This variable was not recorded in one patient (0.5%) from CMJAH. This difference between the samples in times of injury was statistically significant (p =0.0017).
POPULATION GROUP
The majority (91.1%) of patients were blacks (Africans), 3.6% were whites and 5.2% were of other groups. Amongst the sample from CMJAH, blacks constituted 87.5% of patients; 5.5% patients were whites and 7.0% were others. In PMHC, there was a significantly higher proportion (98.4%) of black patients than in CMJAH (P=0.011), and the remaining 1.6% patients were members of other population groups.
AETIOLOGY OF MAXILLOFACIAL FRACTURES
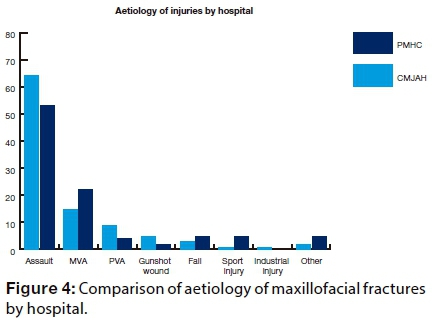
The combined data show that assaults (60.3%) accounted for the majority of fractures, followed by motor vehicle accidents (MVA) accounting for 17.5%. The contribution of other aetiological factors was as follows: pedestrian vehicle accidents 7.5% (PVA), falls 4.6%, gunshot wounds 4.1%, others 3.1%, sport injuries 2.6%, while industrial injuries accounted for the least number of fractures at only 0.3%.
In both units, assaults were the most common cause, accounting for 53.0% of the fractures in the PMHC group and 64.1% fractures in the sample from CMJAH, a rate slightly higher than the overall percentage (60.3%). Motor vehicle accidents followed with 22.7% in PMHC, a rate higher than the CMJAH figure (14.8%) and the overall rate (17.5%). However, no statistically significant differences (p=0.167) were detected when the data from the two units were compared. Pedestrian vehicle accidents accounted for 8.6% of maxillofacial fractures at CMJAH, a rate higher than PMHC (4.5%) and also of the overall rate of 7.5%. Gunshot wounds accounted for 5.5% at CMJAH, a rate higher than that seen at PMHC (1.5%) and also higher than the overall rate of 4.1%. Falls accounted for 6.1% of maxillofacial fractures at PMHC, a frequency higher than the CMJAH sample (3.9%) and the overall rate (4.6%). More patients (6.1%) sustained maxillofacial fractures due to sport injuries in the PMHC group than patients (0.8 %) at CMJAH, with a significant difference (p=0.028) in these data between the two units. The one patient who sustained maxillofacial fractures due to industrial injury was recorded from CMJAH. Other aetiological agents accounted for 6.1% maxillofacial fractures in the PMHC data and 1.6% amongst the presentations at CMJAH (Figure 4).
RELATIONSHIP OF ASSAILANT TO PATIENT.
Of the one hundred and sixteen patients who sustained maxillofacial fractures due to assault, 51.7% knew their assailants. This was the case for 43 CMJAH patients (53.1%) but 38 patients did not know the perpetrators. Amongst the PMHC patients only 17(48.6%) knew their assailants.
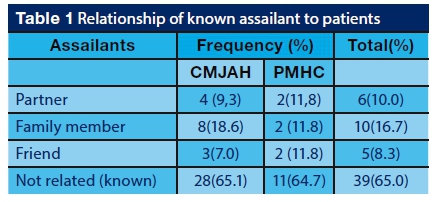
Analysis of the responses of the 60 patients who knew their assailants revealed that 9.3% from CMJAH and 11.8% from PMHC were assaulted by their partners. Ten patients, 18.6% from CMJAH and 11.8% from PMHC were assaulted by family members. Five patients, 7.0% from CMJAH and 11.8% from PMHC were assaulted by friends. Thirty-nine patients, 65.1% of those from CMJAH and 64.7% of those from PMHC, were assaulted by assailants known to them but not related.
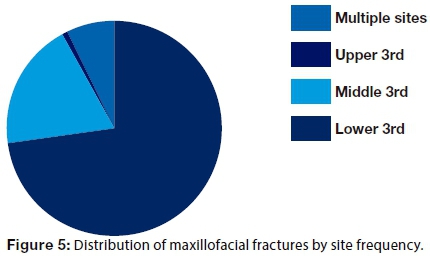
THE FRACTURE PATTERNS
In the total sample, a high proportion (73.0%) of fractures occurred in the lower third of the face, followed by middle third of the face (19.0%), multiple sites (7.0%) and upper third of the face (1.0%), (Figure 5).
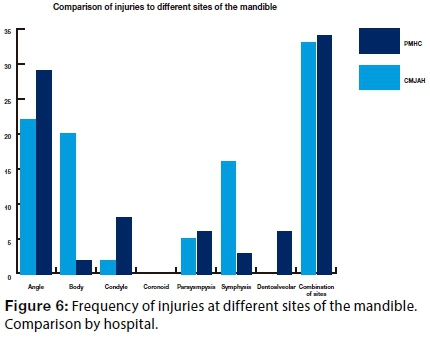
LOWER THIRD FRACTURES
Of the 141 mandibular fractures, an angle of the mandible was the most commonly affected site at both hospitals, (35.5% angle fractures from CMJAH and 33.8% from PMHC), followed by the mandibular body (25.7%). When comparing the proportions of mandibular body fractures between the two units, the difference was found to be statistically significant (p=0.002).
Symphyseal fracture constituted 13.7% of all mandibular fractures, the majority (15.5%) of which were recorded at CMJAH and only 9.9% in PMHC. A significantly higher proportion (p=0.0002) of parasymphyseal fractures (11.9%), were seen at PMHC (23.9%) as compared with the attendances for this problem at CMJAH (6.5%). Condylar fractures made up 11.1% of the total, contributing 15.5% to all fractures seen at PMHC and 9.0% at CMJAH. Much less frequent were dentoalveolar (1.8%), all four fractures being from the PMHC sample. Involvement of the coronoid process was recorded only once at each hospital (0.9%).
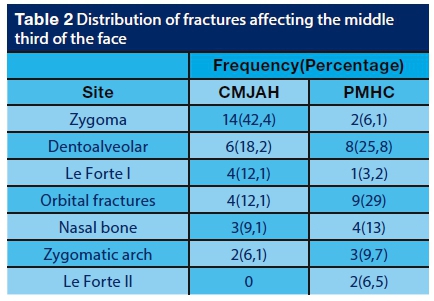
MIDDLE THIRD FRACTURES
Table 2 below shows a comparison of the frequencies of middle third fractures between the two units. Overall, the broken zygoma was the most (28.1%) common midface fracture. When comparing the two units, a statistically significant higher proportion (42.4%) of middle third fractures was noted to have involved the zygoma at CMJAH than the 12.9% occurrence at PMHC (p=0.0087. At PMHC, 25.8% of middle third fractures were on the dentoalveolar region. These fractures accounted for only 18.2% of middle third breakages at CMJAH, and no significant differences were demonstrated (p=0.462) between these data. There is, however, a significant difference (p=0.0010) when comparing the number of orbital fractures recorded at CMJAH (12.1%) and at PMHC (29.0%). Le Forte I and zygomatic arch fractures accounted 7.8% each of the total number of fractures of the middle third of the face. Comparison of the data for Le Forte 1 fractures did not reveal any significant differences. There was also no significant difference (p=0.0618) when comparing the proportions of nasal bone fractures between CMJAH (9.1%) and PMHC (13.0%). Le Forte II fractures accounted for 3.15% of those occurring in the middle third, and all these were recorded at PMHC.
UPPER THIRD FRACTURES
In this sample, frontal fractures accounted for only 1.0% of the total fractures in both units. There was no significant difference (p= 0.088) in the occurrence of the problem between CMJAH (1.6%) and PMHC (6.1%).
MULTIPLE FRACTURED SITES
Multiple fracture sites accounted for 7.0% of the total 227 fractures. The difference of the frequencies between CMJAH (5.5%) and PMHC (9.1%) was not statistically significant (p= 0.346).
DISCUSSION
The aim of this study was to analyse and compare epidemiologic characteristics of maxillofacial fractures between CMJAH, which is in Johannesburg and PMHC, which is in a mainly rural province of Limpopo. There have been a number of epidemiological studies of maxillofacial fractures completed mostly in metropolitan cities of South Africa,8,10 but no similar studies were undertaken in rural provinces. Understanding the patterns helps in determining the level of skills required in both provinces and will assist in the planning for maxillofacial services.
The patterns of maxillofacial fractures between the two units seem to be the same albeit the notable differences in the number of cases consulted in that period. This statistically significant difference in numbers of patients with maxillofacial fractures in the two units is attributed to differences in population sizes in the two provinces. The outcomes of this study do not concur with Al-Dajana et al. who found that most maxillofacial injuries were recorded from the rural counties in Antanario.14
In this study, more than 80.0% of the total study population were males and over 70.0% were between the ages of 20-39 years. These findings were in agreement with results from other studies. 7,10,22 The possible explanation for this finding is because these individuals are in active phase of life, and frequently take part in dangerous exercises and sports, drive motor vehicles carelessly and are more engaged in outdoor activities which are the leading causes of maxillofacial trauma.27,28 Anectodal evidence suggests that there are high levels of irresponsible use of alcohol in this age group as well.
Gupta et al. in 2009 maintained that prevailing socioeconomic, cultural and environmental factors, from one country to another and even within the same country, are the cause of variations in the aetiology of maxillofacial trauma.7 However, noted in this study are the critical issues that firstly, employment status is not a contributing factor in victims of trauma, and secondly, that most maxillofacial fractures occur in the evenings. This latter finding concurs with Al-Dajani et al. who found that most maxillofacial injuries occur at evenings, weekends and during summer.14 This suggests that people who socialise together in high risk geographical areas and in the evenings are more likely to sustain maxillofacial injuries irrespective of the employment status.
This study found that black Africans were the most common victims of maxillofacial injuries. This is a reflection of demographics and of the socioeconomic situation in the country, as these units are public hospitals which are used by people without medical insurance.
Assaults (60.3%), followed by road traffic accidents (17.5%) were the leading causes of maxillofacial fractures identified in this study. This concurs with some studies which reported assaults as the leading cause of maxillofacial fractures,8,14 but differ with several investigations which have found road traffic accidents to be the most common cause of maxillofacial fractures in developing countries.2,6,23-26 The current study found that a slightly higher proportion (64.1%) of fractures due to assaults was reported at CMJAH, while most maxillofacial fractures from road traffic accidents were from PMHC (22.7%). The higher numbers due to assaults in Johannesburg could be attributed to crowding and the challenging crime rate of that region, which contribute to interpersonal violence. Anecdotal evidence suggests that many people in rural provinces tend to use public transport, like buses, where a single accident can result in many casualties. It can also be postulated that the low proportion of maxillofacial fractures due to road traffic accidents in the Johannesburg region may be attributed to good quality roads and visible policing.
Another relevant finding was that there was a statistically significant difference (p = 0.028) between the two units of the proportions of patients who sustained maxillofacial fractures due to sport injuries. More patients ( 6.1%) reported at PMHC with sport-related injuries than at CMJAH (0.8%). This could be attributed to inadequate recreational facilities and fewer sporting codes in the rural province as opposed to Johannesburg. It is general knowledge that soccer and boxing are some of the more risky sporting codes in terms of exposing patients to maxillofacial fractures. Unfortunately, these are the most accessible sports in Limpopo.
A significant number of patients (64.9%) who sustained maxillofacial fractures due to assault knew their assailants, although they were not related to them. This finding suggests that violence resulting in maxillofacial trauma mostly affects individuals living in the same geographical area or socialising together. Unfortunately, this study did not determine whether these known assailants were reported to the law enforcement officers.
The mandible was the most affected site of the face accounting for 73.0% incidence in the total study population, followed by the zygoma. This concurs with other studies on maxillofacial trauma.6,8,20 These results are however in reverse with those reported by Gupta et al. in 2009 where zygoma was the most affected maxillofacial bone, followed by the mandible.7 The reason for the preponderance of the mandible as the commonly affected bone in maxillofacial trauma is because of its prominence, mobility and its selection as a target of intentional violence. Whilst the mandible is overall a strong bone, it nevertheless has several areas of weakness that are prone to fracture.27
The angle of the mandible was the most (35.0%) commonly affected site in this study population (Fgure 9). This does not agree with the European survey which reported the condyle as the most commonly affected part of the mandible, followed by the angle1. The majority of the fractured body and angle of the mandible were recorded on the right side, as opposed to studies where assault resulted in left side facial injuries.10 This finding suggests that probably most patients were assaulted from behind, or while running away from imminent danger or were kicked.
This study found that the CMJAH patients had a greater number of patients with zygomatic fractures due to road traffic accidents than did those at PMHC. This difference between the two units was statistically significant (p=0.0087). This association of zygomatic fractures with road traffic accidents has been reported in other studies,28-31 and points to possible failures to comply with traffic rules as these injuries suggest that seatbelts are not being used while driving.
This study shows that the patterns of trauma in the two regions are the same, and that any differences reflect the relative total population sizes in the two regions. The limitation of the study is the small sample size. The maxillofacial surgeons diagnosing the fractures were not calibrated. Future multicentre studies with large sample sizes will give better perspectives of the patterns of trauma in rural and urban areas.
ACRONYMS
CMJAH : Charlotte Maxeke Johannesburg Academic Hospital
MVA : motor vehicle accidents
PMHC : Polokwane -Mankweng Hospital Complex
PVA : pedestrian vehicle accidents
References
1. Boffano P, Roccia F, Zavattero E, Dediol E, Uglesic V, Kovacic Z, Vesnaver A, Konstantinovic VS, Petrovic M, Stephens J, Kanzaria A. Assault-related maxillofacial injuries: the results from the European Maxillofacial Trauma (EURMAT) multicenter and prospective collaboration. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 2015;119(4):385-91. [ Links ]
2. Ajike SO, Adebayo ET, Amanyiewe EU, Ononiwu CN. An epidemiologic survey of maxillofacial fractures and concomitant injuries in Kaduna, Nigeria. Nigerian Journal of Surgical Research 2005;7:251-5. [ Links ]
3. Lee K. Global Trends in Maxillofacial Fractures. Craniomaxillofacial Trauma Reconstruction 2012; 5:213-22. [ Links ]
4. Sojat AJ, Meisame T, Sandar GKB, Clokie CML. The epidemiology of mandibular fractures treated at the Toronto General Hospital: A review of 246 cases. Journal Canadian Dental Association 2001;67:640-5. [ Links ]
5. Majumder B, Karmakar R, Bose T, Dasguptas S, Basu R. Some host factors and seasonal variations in the fatal road accidents occurring in Eastern Suburban Calcutta. Indian Journal of Public Health 1996;40:46-9. [ Links ]
6. Shayyab M, Alsoleihat F, Ryalat S, Khraisat A. Trends in the pattern of facial fractures in different countries of the world. International. Journal of Morphology 2012;30: 745-56. [ Links ]
7. Gupta AK, Garg R, Gupta A, Bajaj K. A retrospective analysis of 189 patients of maxillofacial injuries presenting to a tertiary care hospital in Punjab, India. Journal Maxillofacial Oral Surgery 2009;8:241-5. [ Links ]
8. Desai J, Lownie JF, Cleaton-Jones PE. Prospective audit of mandibular fractures at the Charlotte Maxeke Johannesburg Academic Hospital. South African Journal of Surgery 2010; 48:120-6. [ Links ]
9. Schneider D, Kàmmerer PW, Schön G, Dinu C, Radloff S, Bschorer R. Etiology and injury patterns of maxillofacial fractures from the years 2010 to 2013 in Mecklenburg-Western Pomerania, Germany: A retrospective study of 409 patients. Journal of Cranio-Maxillofacial Surgery 2015; 43(10):1948-51. [ Links ]
10. Beaumont E, Lownie JF, Cleaton-Jones PE, Newton NPD. An analysis of fractures of the facial skeleton in the three populations in the Johannesburg urban area. Journal of the Dental Association of South Africa1985; 40:633-8. [ Links ]
11. Bamjee Y. Paediatric maxillofacial trauma. Journal of the Dental Association of South Africa 1996;51: 750-3. [ Links ]
12. Jung TK, De Silvahl, Konthasingha PP, Tong DC. Trends in paediatric maxillofacial trauma presenting to Dunedin Hospital. New Zealand Dental Journal 2015; 111: 76-9. [ Links ]
13. van As AB, van Loghem AJ, Biermans BFJ, Douglas TS, Wieselthaler N, Naidoo S. Causes and distribution of facial fractures in a group of South African children and the value of computed tomography in their assessment. International Journal of Oral and Maxillofacial Surgery 2006;35: 903-6. [ Links ]
14. Al- Dajani M, Quinonez C, Macpherson AK, Clokie C, Azarpazhooh A. Epidemiology of maxillofacial injuries in Ontario, Canada. Journal Oral and Maxillofacial Surgery 2015; 73:693.e1-693.e9. [ Links ]
15. Lindqvist C, Sorsa S, Hyikas T, Santaytha S. Maxillofacial fractures sustained in bicycle accidents. International Journal of Oral Surgery 1986;15:12-8. [ Links ]
16. Thom JJ, Mogeltoft M, Hansen PK. Incidence and aetiology pattern of jaw fractures in Greenland. International Journal of Oral and Maxillofacial Surgery 1986;15:372-9. [ Links ]
17. Gassner R, Tuli T, Emshoff R, Waldhart E. Mountain biking- a dangerous sport in comparison with bicycling on oral and maxillofacial trauma. Journal of Oral and Maxillofacial Surgery1999; 28:188-91. [ Links ]
18. Peden M, Holmgren E P, Dierks EJ, et al. Facial computed tomography use in trauma patients who require a head computed tomogram. Journal of Oral and Maxillofacial Surgery 2004;62:913-8. [ Links ]
19. Kruger E, Smith K, Tennant M. Jaw fractures in the indigenous and non-indigenous populations of Western Australia, 1999-2003. International Journal of Oral and Maxillofacial Surgery 2006; 35: 658-62. [ Links ]
20. Adeyemo WL, Ladeinde AL, Ogunlewe MO,James O. Trends and characteristics of oral and maxillofacial injuries in Nigeria: a review of the literature. Head and Face Medicine 2005; 1:7-15. [ Links ]
21. Alves L, Aragão I, Sousa M C,Gomes E. Pattern of maxillofacial fractures in severe multiple trauma patients: a 7-year prospective study. Brazilian Dental Journal 2014:25: 561-4. [ Links ]
22. Singh AS, Altini M, Bouckaert MM. An audit of maxillofacial fractures in patients attending the Medunsa Oral Health Centre, University of Limpopo, Medunsa Campus. Unpublished MSc thesis,2009. [ Links ]
23. Conforti PJ, Haung RH, Likavec M. Management of closed head injury in the patient with maxillofacial trauma. Journal of Oral and Maxillofacial Surgery 1993;51:298-303. [ Links ]
24. Hohlrieder M, Hinterhoelzl J, Ulmer H, Lang C, Hackl W, Kampfl A, Benzer A, Schmutzhard E, Gassner R. Traumatic intracranial haemorrhages in facial fracture patients: review of 2,195 patients. Intensive Care Medicine. 2003;29(7):1095-1000. [ Links ]
25. Holmgren EP, Dierks EJ, Homer LD, Potter BE. Facial computed tomography use in trauma patients who require a head computed tomogram. Journal of Oral and Maxillofacial Surgery 2004;62(8):913-8. [ Links ]
26. Udeabor SE, Akinbami BO, Yarhere KS, Obiechina AE. Maxillofacial fractures: Pattern of presentation, and treatment in University of Poet Harcourt teaching hospital, Port Harcourt, Nigeria. Journal of Dental Surgery .2014; 1-5. [ Links ]
27. Oji C. Jaw fractures in Enugu, Nigeria.1985-1995. British Journal of Oral and Maxillofacial Surgery. 1999;37:106- 9. [ Links ]
28. Cheema SA, Amin F. Incidence and causes of maxillofacial skeletal injuries at the Mayo Hospital in Lahore, Pakistan. British Journal of Oral and Maxillofacial Surgery.2006; 44:232-41. [ Links ]
29. Covington DS, Wainwright DJ, Teichgraeber JF, Parks DH. Changing patterns in the epidemiology and treatment of zygoma fractures: 10 year review. Journal of Trauma and Acute Care Surgery.1994;37:243-8. [ Links ]
30. Ungari C, Filiaci F, Riccardi E, Rinna C, Iannetti G. Etiology and incidence of zygomatic fracture: a retrospective study related to a series of 642 patients. European Review of Medical Pharmacological Sciences. 2012; 16: 1559-62 [ Links ]
31. Van der Spuy J.W. Trauma, alcohol and other substances. South African Medical Journal 2000, 90: 244-6. [ Links ]
 Correspondence:
Correspondence:
Brampie M Mogajane
Craniomaxillofacial Surgeon, Department of Maxillo-Facial and Oral Surgery
School of Oral Health Sciences, Faculty of Health Sciences
University of the Witwatersrand
Johannesburg Tel (011)
717-2243, or Tel: 011 488 4606, Fax 086765 4436
mogajaneb@yahoo.com














