Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Dental Journal
versión On-line ISSN 0375-1562
versión impresa ISSN 0011-8516
S. Afr. dent. j. vol.73 no.2 Johannesburg mar. 2018
CASE REPORT
Hyalinising clear cell carcinoma of the maxilla in a young adult female
F BhamjeeI; A JefthaII; H HolmesIII; R RobertsIV; T RobertsV
IBChD Department of Oral Medicine and Periodontics, Faculty of Dentistry, University of the Western Cape
IIMChiD, BChDDepartment of Oral Medicine and Periodontics, Faculty of Dentistry, University of the Western Cape
IIIMChiD, MSc, BChDDepartment of Oral Medicine and Periodontics, Faculty of Dentistry, University of the Western Cape
IVMBChB, MMed(UCT), FCPathfSAJAnat.Division of Anatomical Pathology. University of Cape Town and National Health Laboratory Service
VMChiD, BChiD. Department of Oral Pathology, Faculty of Dentistry, University of the Western Cape
CASE REPORT
A 23-year-old healthy female, with a history of smoking, presented to the Oral Medicine Clinic complaining of a growth on the right side of her upper jaw. She reported having noticed the lesion approximately one year prior to her initial presentation and explained that the absence of symptoms and the assumption that the growth was a dental abscess had delayed her seeking professional assistance. Recent symptoms of pain and accelerated enlargement were reported as having developed two months previously, the pain being described as mild and intermittent, but with increasing intensity while eating. This had motivated her to consult a private dental practitioner who subsequently referred her to the Oral Medicine Clinic for excisional biopsy.
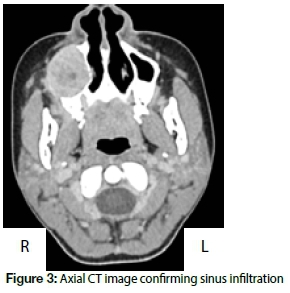
Her dental history was limited to previous dental extractions without prosthetic replacement and she acknowledged usually presenting for dental treatment only when in pain. The Extra-oral examination demonstrated a right submandibular lymphadenopathy and facial asymmetry due to the displacement of the right cheek by the intraoral lesion. An intraoral examination revealed a state of poor oral hygiene with retained roots, carious teeth and a collapsed partially edentulous occlusal scheme. In the first quadrant, a large exophytic, broad-based mass enveloped tooth 15, extending from the distal aspect of the retained root of tooth 14 to the mesial aspect of tooth 18 (Figure 1). The margins of the growth were diffuse and integrated into the surrounding keratinized gingival tissues at both facial and palatal surfaces. In colour and texture it also closely matched the surrounding tissues, being smooth surfaced, firm and not blanching on palpation. Minor surface ulcerations were noted on the occlusal surface of the lesion which contacted the lower edentulous ridge during mastication. A list of differential diagnoses for the clinical presentation included pyogenic granuloma, peripheral giant cell granuloma, fibrous epulis, and peripheral ossifying fibroma. A salivary gland neoplasm was suspected and included in the differential list once the destructive nature of the lesion was seen radiographically (Figure 2). Assessment of the orthopantomogram (OPG) revealed the presence of radiolucency in the first quadrant from the 15 to 18 regions, with obliteration of the sinus floor. The root of tooth 15 was mesially displaced and appeared to be "floating" up against the root remnant of tooth 14. Caries was noted on teeth 18, 38, 37 and 48 (Figure 2). An axial CT image confirmed infiltration into the right maxillary sinus (Figure 3).


A 1cm wide elliptical incisional biopsy was taken from the area immediately distal to tooth 15. The vertical incision was approximately 1-1.5cm deep. The biopsy specimen was placed into a 10% formaldehyde solution and sent to the pathology laboratory for histopathological evaluation. The histopathological report was consistent with a diagnosis of a hyalinising clear cell carcinoma. The biopsy was extensively assessed by multiple consultant oral pathologists in order to establish the diagnosis. The final consensus histopathological finding of HCCC was based on the following findings;
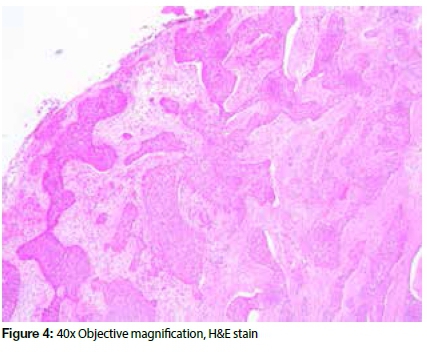
At 40x objective magnification (Figure 4, H&E) showed infiltrative nests and trabeculae of malignant cells, invading into a desmoplastic stroma. Peri-tumoural retraction artefact was noted.
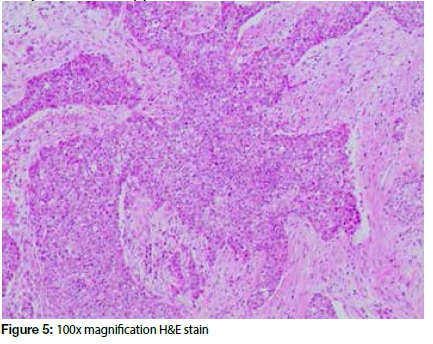
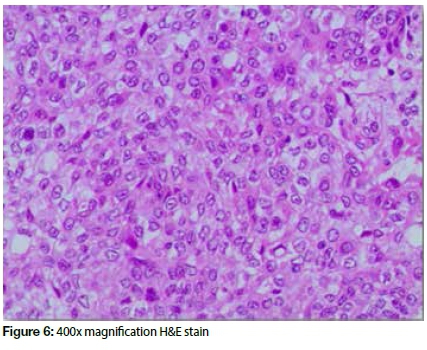
At 100x magnification (Figure 5), the H&E highlighted the epithelial nature of the carcinoma, with the malignant cells showing cellular cohesion and moderate amounts of cytoplasm. Figure 6 at 400x objective magnification shows the tumoural cellular morphology, with large nuclei, single central nucleoli, irregular and notched nuclear membranes, moderate amounts of pale eosinophilic-to-clear cytoplasm and defined cell borders. In areas, the cytoplasm had a finely vacuolated appearance,
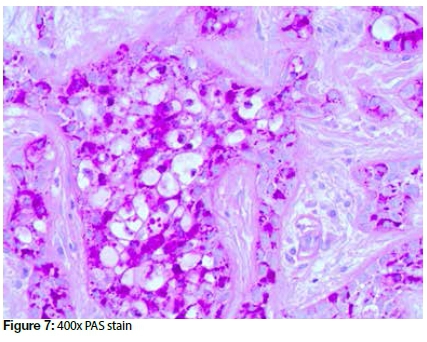
A PAS and DPAS at 400x (Figures 7 and 8) highlighted the observation that the tumoural cells contain intracytoplasmic PAS positive, Diastase PAS sensitive glycogen. AE1/AE3, p63 and EMA showed immunopositivity.

The patient was immediately referred to Head and Neck Oncology Unit at Groote Schuur Hospital for further management. Of considerable importance was the confirmation that the presenting lesion was the primary, with no evidence of metastases. The complete patient workup included serial blood tests, head and chest radiographic studies, head and body CT scans and regional lymph node biopsies. Surgical intervention included a partial maxillectomy with submandibular and cervical node neck dissection and tracheostomy. Postoperative radiotherapy was initiated after postoperative healing and stabilisation.
DISCUSSION
Hyalinizing clear cell carcinoma (HCCC) is a rare low-grade malignancy with an infiltrative growth pattern. It affects mainly the minor salivary glands of adult women and accounts for less than 1% of all salivary gland tumours. The WHO classifies HCCC as being a variant of a clear cell epithelial-myoepithelial carcinoma. Many researchers, however, now think it should be classified as a separate entity with its own characteristic histological features.1 In the oral cavity, HCCC generally arises from the minor salivary glands, with the most frequent site of occurrence being the tongue, followed by the palate, floor of the mouth, buccal mucosa, retromolar trigone and jaws. Other sites include the parotid glands, the hypopharynx and the nasopharynx.1 HCCC generally develops in women in the fifth to seventh decades presenting as a slow-growing, painless submucosal mass without surface ulceration, unless it has been secondly traumatized. Numbness, pain and even limitation of movement have been noted in lesions involving the tongue. Bone destruction and movement of teeth have been reported when the lesion affects the jaws.1 The presented case is unique as the age of presentation is significantly younger than that recorded in previous literature. Microscopically, these tumours contain a significant proportion of neoplastic cells with a clear cytoplasm and morphologically do not fit into other categories of salivary gland malignancies. The microscopic diagnosis of HCCC is challenging as the spectrum of its microscopic features frequently overlaps those of other salivary gland neoplasms which also contain clear cells.2 Similarly, non-salivary, metastatic and odontogenic tumours that show clear cells should be included in the histologic differential diagnosis. To be excluded are the salivary gland tumours with a clear cell component such as epithelial -myoepithelial carcinoma, myoepithelial carcinoma, clear cell mucoepidermoid carcinoma, acinic cell carcinoma, polymorphous low-grade adenocarcinoma and clear cell oncocytoma. Metastatic possibilities include renal cell carcinoma and balloon cell melanoma. Odontogenic tumours with a clear cell component include entities such as calcifying epithelial odontogenic tumor (Pindborg tumour) and clear cell odontogenic carcinoma. Generally, the hyalinizing nature of the stroma can be a feature that points to a diagnosis of HCCC as well as the PAS and DPAS positive glycogen rich clear cells.34 Treatment of HCCC involves local excision with healthy margins followed by reconstruction. If lymph node metastases are detected or considered to be likely based on clinical and radiographic investigation, partial or modified neck dissection is performed.3 Postoperative radiotherapy, used to improve metastatic control in malignant salivary gland tumours in general, is suggested when the surgical margins are unclear or if the lesion demonstrates aggressive behaviour. Chemotherapy has generally not been considered to be effective in the management of salivary gland tumours. The rare nature of the lesion as well as the paucity of documented literature, limits our ability to draw conclusions regarding optimal management of these lesions.3
CONCLUSION
A diagnosis of hyalinising clear cell carcinoma of the maxilla in a female in the second decade of life is a rare entity. The diagnostic protocol followed was in keeping with the admittedly scant current evidence from the literature of this tumour of minor salivary gland origin. Thankfully, the patient had no lymphatic involvement and was clear of all malignancy at the one year follow-up.
Tumours of the minor salivary glands remain rare in occurrence but this experience emphasizes the need for prompt diagnosis of swellings within the oral cavity at any age.
Declaration: No conflict of interest declared.
ACRONYMS
AE1 and AE3: Cytokeratin
CEA : Carcinoembryonic antigen
CT : Computed tomography
DPAS : Periodic acid-Schiff-Diastase
EMA : Epithelial membrane antigen
H&E : Haemotoxylin and Eosin stain
HCCC : Hyalinising clear cell carcinoma
OPG : Orthopantamogram
PAS : Periodic acid-Schiff stain p63: Tumour suppressor protein
SMA : Smooth muscle actin
References
1. Angiero, F, Stefani M. Hyalinizing clear cell carcinoma arising on the anterior palatoglossal arch. Anticancer Research. 2007. 27: 4271-8. [ Links ]
2. Solar A.A , Schmidt B.L and Jordan R.C.K. Hyalinizing clear cell carcinoma : Case series and comprehensive review of the literature. Cancer. 2009 115:75-83. [ Links ]
3. Kauzman A, Tabet J-C, Stiharu T-I. Hyalinizing clear cell carcinoma: A case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011. 112:e26-e34s. [ Links ]
4. Berho M, Huvos A.G. Central hyalinizing clear cell carcinoma of the mandible and the maxilla : a clinicopathologic study of two cases with an analysis of the literature. Hum Pathol.1999. 30:101-5. [ Links ]
 Correspondence:
Correspondence:
A Jeftha
Division of Oral Medicine and Periodontology, University of the Western Cape
Dental Faculty Francie Van Zyl Drive, Tygerberg Campus
Tel: 27 21 9373158
Email ajeftha@uwc.ac.za














