Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.73 n.2 Johannesburg Mar. 2018
CASE REPORT
Oral pemphigus vulgaris with skin and ocular involvement
D TemilolaI; H HolmesII; S Mulder-van StadenIII; A AfroghehIV; J EngelbrechtV
IBChD. Division of Oral Medicine and Periodontics, Faculty of Dentistry, University of the Western Cape
IIBChiD, MSc, MChiD. Division of Oral Medicine and Periodontics, Faculty of Dentistry, University of the Western Cape
IIIBChiD, MChiD. Division of Oral Medicine and Periodontics, Faculty of Dentistry, University of the Western Cape
IVBChiD, MSSc, MChiD, IFCAP. Division of Oral and Maxillofacial Pathology, Faculty of Dentistry, University of the Western Cape, National Health Laboratory Service, Tygerberg Hospital
VDepartment of Ophthalmology, Stellenbosch University, Tygerberg Hospital (who provided clinical information)
CASE REPORT
A 54-year-old female was referred to the Oral Medicine Clinic at the University of the Western Cape (UWC), Oral Health Centre, Tygerberg campus, by her general practitioner. She complained of persistent painful oral ulcers that had appeared approximately nine months previously. Small vesicles had been noted by the patient prior to the development of the oral ulcers. The patient reported having taken a course of antibiotics and using an antibacterial mouthrinse with no response to treatment. She also complained of a left chronic conjunctivitis, with itching, burning and tearing of the left eye, for which she had used numerous over-the-counter eye drops with no symptomatic relief. Her eye symptoms had started a few weeks following the onset of the oral ulcers. The patient's medical history was otherwise unremarkable. She had no known drug allergies.
Extra-oral examination revealed diffuse erythema of the left ocular cojunctiva (Figure 1). Intra-oral examination disclosed multiple superficial, large, irregular areas of ul-ceration in the hard palate, soft palate, floor of mouth and buccal mucosa, all on a background of white-erythematous mucosa (Figures 2-4). Desquamative gingivitis of mandibular and maxillary gingiva was seen (Figure 5). The only unaffected oral sites were the tongue and the lips.





Based on the clinical features a differential diagnosis of pemphigus vulgaris and benign mucosal pemphigoid was considered. An incisional biopsy of the intact buccal mucosa adjacent to the area of ulceration was performed under local anesthesia.
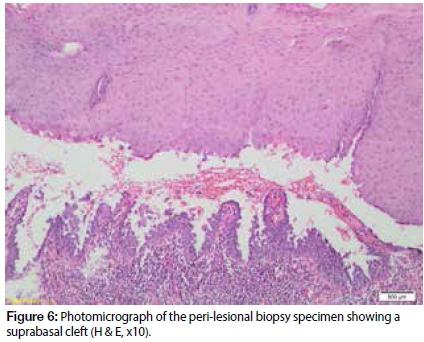
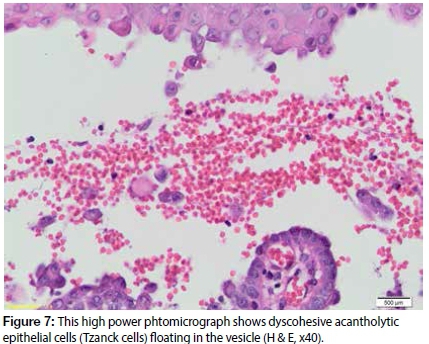
Histological evaluation of the biopsy specimen revealed squamous mucosa with an extensive cleft above the basal cell layer, with the basal cells remaining adhered to the basement membrane (Figure 6). The suprabasal cleft contained rounded acantholytic epithelial cells (Figure 7). The subepithelial connective tissue showed a chronic inflammatory cell infiltrate. Based on the clinical and microscopic features a final diagnosis of pemphigus vulgaris was established. The patient was placed on a course of systemic steroids (prednisone 60 mg/day for seven days). For ocular symptoms an ocular lubricant and a topical corticosteroid were prescribed by the ophthalmologist. After seven days of treatment there was complete remission of the ocular and oral mucosal lesions. However, the patient developed small erythematous vesicles on extensor surfaces of both thighs and was subsequently referred to the dermatologist (Figure 8).

DISCUSSION
Pemphigus vulgaris (PV) is a rare vesiculobullous disease characterized by blistering of the skin and mucous membranes. Its incidence ranges from 0.42 to 1.62 cases per 100,000, affecting predominantly adults with a mean age of 50 years. The disease occurs equally in both genders.1 The term "pemphigus" originates from the Greek word "pemphis", meaning blister. The aetiology of PV is autoimmune,2 and its main clinical characteristic is the development of blisters of the skin and mucous membranes due to the abnormal production of IgG autoantibodies against desmosomes (desmoglein 1 and desmoglein 3). Desmosomes are intercellular junctions that provide strong adhesion between the keratinocytes.
The loss of desmosomes by IgG autoantibodies results in intraepi-thelial separation forming a blister.3 PV has been shown to have a strong genetic basis with a racial/ethnic-specific incidence in Ashke-nazi Jews and people of Mediterranean descent.
Initiating factors have been reported in the literature and include certain foods, infections, neoplasms, and drugs. The drugs commonly implicated are those in the thiol group - in particular captopril, pencillamine and rifampicin.2
Blisters, irregular erosions and ulcerations are the main clinical features of PV. When the blister ruptures, it leaves an erythematous, extremely painful ulcerated base, with loss of fluid and electrolytes. Mucosal lesions usually precede skin lesions, and may be the sole manifestation of the disease.4 Erosions are usually seen in mucous membranes of the oral cavity, but may also be observed within the nasopharynx, larynx, oesophagus, genital and ocular mucosa. Cases with simultaneous involvement of mucous membranes of different anatomical sites have been described in the literature.5 The oral lesions of PV are extremely painful and result in abundant salivation, halitosis, difficulty in swallowing and phonation.
The most common sites of oral involvement include the buccal mucosa, soft palate, labial mucosa, and gingiva, although any oral site may be affected.6
Skin lesions may occur in any region of the body, affecting predominantly the trunk and the limbs, especially large areas of bending folds such as the neck.
When ocular involvement is present, conjunctivitis is the most common manifestation. Chronic conjunctivitis leads to loss of goblet cells that produce mucus, resulting in burning and tearing of the eyes. Adequate eye care is required to prevent infection, scar formation and corneal perforation, which may result in blurring or loss of vision. 1,7-11
The differential diagnosis of PV includes several autoimmune and infective diseases that present with blisters, erosions and ulcera-tions such as benign mucosal pemphigoid, systemic lupus erythe-matosus, epidermolysis bullosa, erosive lichen planus, erythema multiform, herpes simplex and zoster. 11 For a definitive diagnosis, an incisional biopsy of a peri-lesional tissue should be performed and the clinical findings correlated with the microscopic features. In some cases, direct and indirect immunofluorescence studies may be used for confirmation of PV. Histopathological examination of the peri-lesional mucosa shows an intra-epithelial vesicle above the basal cell layer, with the basal cells remaining adhered to the underlying basement membrane (Figure 6). The vesicule often contains detached rounded keratinocytes with swollen hyperchromatic nuclei called Tzanck cells (Figure 7).
The mainstay of treatment for PV is systemic corticosteroids. Topical therapy of ocular and oral mucosal lesions may be required to relieve local pain and discomfort (e.g. creams, pastes, drops, intralesional injections).12,13 Prednisone is the drug of choice, the maximum daily dose of which is 120 mg (1-2 mg / kg/ day). The initial dose of prednisone is typically about 0.75 to 1 mg/kg/day. If the initial dose is ineffective in controlling the disease, the dose is increased by 25% to 50% every five to seven days.
Immunosuppressive drugs (such as aziatropin, cyclosporine, cyclo-sporphamide, prostaglandin, chlorambucil levamizol and immu-noglobulins) can be used in resistant lesions or aimed at reducing the steroidal dose and its side effects.14 Immunosuppressive therapy may result in the development of opportunistic infections such as candidiasis and herpes, and new therapy should be instituted for these conditions.11 Currently, low-level laser therapy combined with immunosuppressants has been shown to be effective in the management of PV.15
Low-level laser therapy could result in immediate and significant analgesia and improved wound healing within the observation period and follow-up. Furthermore, a decrease in the discomfort of the pa-tienthas been reported as well as no recurrence of the pemphigus vulgaris lesions.
CONCLUSION
Dentists should be aware of the oral and ocular manifestations of PV, since these precede the appearance of cutaneous lesions. Ther efore, the dentist may not only be the first but also the most important health care professional responsible for the diagnosis of the disease, as early treatment may prevent life threatening complications such as loss of vision. Due to the multisystemic nature of PV, a multidisciplinary approach for the management of the disease is required, involving dentists, oral medicine specialists, pathologists, dermatologists, ophthalmologists and immunologists. Steroids and immunosuppressive agents are commonly employed in the management of PV to reduce the production of autoantibodies.
Currently, low-level laser therapy has been shown to be an effective and recommended alternative therapeutic option, providing improvements in the health and quality of life of patients.
ACRONYMS
PV : Pemphigus vulgaris
References
1. Tan JC, Tat LT, Francis KB, Mendoza CG, Murrell DF, Coroneo MT. Prospective study of ocular manifestation of pemphigus and bullous pemphigoid identifies a high prevalence of dry eye syndrome. Cornea. 2015; 34(4):443 - 8. [ Links ]
2. Kapoor S, Sikka P, Kaur G.P. Pemphigus vulgaris of oral cavity: A case report with its treatment strategies. International Journal of Nutrition, Pharmacology, Neurological Diseases 2013;3(2):146. [ Links ]
3. Pan M, Liu X, Zheng J. The pathogenic role of autoantibodies in pemphigus vulgaris. Clinical and Experimental Dermatology, 2011;36(7):703-7. [ Links ]
4. Shrivastava S, Nayak S, Nayak P, Sahu S. Oral pemphigus vulgar-is: a case report.IJSS Case Reports Reviews.2015;1(8):17-9. DOI: 10.17354/cr/2015/05. [ Links ]
5. Goes PEM, Luna AHB, De Figueiredo LS, Montenegro, EDAS, Da Silveira KG, Maia FPA, De Paiva MAF. Pemphigus vulgaris with oral mucosa and skin involvement: A case report. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 2015; 120(2):e57. [ Links ]
6. Chi AC, Ravenel MC, Neville BW, Bass EB Jr. A patient with painful ulcers. Journal American Dental Association 2006; 137:626-9. [ Links ]
7. Uludag HA, Uysal Y, Kucukevcilioglu M, Ceylan OM, Onguru O, Arca E. An uncommon ocular manifestation of pemphigus vul-garis: conjunctival mass. Ocular Immunology and Inflammation, 2013;21(5):400-2. [ Links ]
8. Palleschi GM, Giomi B, Fabbri P. Ocular involvement in pemphigus. American journal of ophthalmology 2007;144(1):149-52. [ Links ]
9. Merchant S, Weinstein M. Pemphigus vulgaris: the eyes have it. Pediatrics, 2003;112(1) :183-5. [ Links ]
10. Olszewska M, Komor M, Mazur M, Rogozinski T. Response of ocular pemphigus vulgaris to therapy. Case report and review of literature. Journal of Dermatological Case Reports 2008;2(1) :1. [ Links ]
11. de Souza RS, da Silva JB, dos Santos CC, Neto RG, Giovani EM. Manifestation of vulgar pemphigus in eyelid mucosa: clinical case report. Journal of Ophthalmology and Visual Neurosciences 2017;2:1-4. [ Links ]
12. Mignogna MD, Lo Muzio L, Mignogna RE, Carbone R, Ruoppo E, Bucci E. Oral pemphigus: long term behaviour and clinical response to treatment with deflazacort in sixteen cases. J Oral Pathol Med 2000; 29:145-52. [ Links ]
13. Cholera M, Chainani-Wu N. Management of pemphigus vulgaris. Advances in Therapy 2016;33(6):910-58. [ Links ]
14. Meurer M. Immunosupressive therapy for autoimmune bullous diseases. Clinics in Dermatology 2012;30:78-83. [ Links ]
15. Minicucci EM, Miot HA, Barraviera SR, Almeida-Lopes L. Low-level laser therapy on the treatment of oral and cutaneous pemphigus vulgaris: case report. Lasers Medical Science. 2012;27(5):1103-6. [ Links ]
 Correspondence:
Correspondence:
Dr. Haly Holmes
Division of Oral Medicine and Periodontology
University of the Western Cape Dental Faculty
Francie Van Zyl Drive, Tygerberg Campus
Tel: 27 21 9373102
Email: hholmes@uwc.ac.za














