Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.72 no.10 Johannesburg Nov. 2017
http://dx.doi.org/10.17159/2519-0105/2017/v72no10a1
RESEARCH
The prevalence of occupational health-related conditions among oral health practitioners in KwaZulu-Natal, South Africa
R MoodleyI; S NaidooII; J Van WykIII
IB Dent Ther (UKZN), MSc Dental Public Health (UWC). Discipline of Dentistry, School of Health Sciences, University of KwaZulu-Natal, South Africa
IIMBChB (Natal), PhD (Utrecht). Discipline of Public Health Medicine, School of Nursing and Public Health, University of KwaZulu-Natal, South Africa
IIIPhD. Discipline of Clinical and Professional practice, School of Health Sciences, University of KwaZulu-Natal, South Africa
ABSTRACT
INTRODUCTION: Oral health practitioners may be affected by occupational health-related conditions associated with their work environment. There is a lack of relevant data on the prevalence of these conditions among dentists, dental therapists and oral hygienists in KwaZulu-Natal.
AIM: To describe the burden of occupational health-related conditions among oral health practitioners in KwaZulu-Natal, South Africa.
METHODS: This cross sectional study evaluated data obtained through a self-administered questionnaire that sought information on demographics, occupational health, psychosocial risk factors, work tasks and planning. Data was exported from QuestionPro and analysed in SPSS version 24. Frequencies and means with standard deviations were calculated for categorical and continuous variables respectively
RESULTS: Oral hygienists most frequently reported symptoms of musculoskeletal disorders affecting the neck (70%) and the hand (56.5%). Dentists reported the highest prevalence of shoulder pain (55.8%) and of percutaneous injuries (42,3%). The dentists, dental therapists and oral hygienists also reported latex allergy (10.4%) and percutaneous injuries (32.6%)
CONCLUSION: The prevalence of occupational health-related conditions reported by the oral health care workers indicate the need to raise awareness about occupational health and warrants the inclusion of these issues on education programs and dental curricula to ensure a healthy work environment.
Key words: Musculoskeletal disorders, percutaneous injury, allergy, dental amalgam, dental curriculum
INTRODUCTION
Occupational health aims at maintaining the physical, mental and social wellbeing of workers. Occupational related- health conditions in dentistry are associated with risks and hazards, and lead to poor health outcomes, affecting the quality of life of the oral health practitioner. Occupational hazards refer to the risk or danger associated with working conditions,1 and are classified as chemical, biological, physical, psychological and ergonomic.
1. Chemical: Dentists, dental therapists and oral hygienists are exposed to many hazards that include, among others, inhalation of gases during general anaesthesia, latex allergies, allergies to monomers and inhalation of mercury vapour.
2. Biological: The risk of infection by various bacteria and viruses associated with dental work. Dentists have a higher risk of contracting Hepatitis B than members of the general population.2 Proper infection control techniques, vaccines and continuous education are needed to reduce the risks of percutaneous injuries (PCI).3 Bio-aerosols in a practice may be controlled through measures including the use of protective gear, rinsing the patient's mouth with antiseptic prior to a procedure, high performance suction and the use of devices to reduce air contamination.4 Dental amalgam, which contains elemental mercury, is still used by dental practitioners in SA. Occupational exposure to mercury occurs when workers inhale vapours and through dermal absorption.5 The use of this material is controversial as mercury is a hazard to the environment when discharged into waste. The environmental impact of amalgam was the concern of dentists investigating the material, although they favoured its continuous use.6
3. Physical: Physical hazards include noise, vibration, radiation, ventilation, air quality and heat. Work related musculoskeletal disorders (MSD) refer to a range of inflammatory and degenerative disorders and diseases. These conditions may lead to pain and/or impairment of function and can affect the neck, arms, legs, back and hips.7 The afflictions can be minor disorders or disabling, irreversible injuries which are often aggravated by work. The acute, painful type of MSD is caused by a sudden failure in muscle function. The chronic type presents as a lingering pain caused by permanent strain on the muscles, leading to dysfunction.8 Musculoskeletal disorders are an occupational health related condition that is costly in both time and money and which may result in decreased productivity or even loss of a career.2 The cost of MSD and carpal tunnel syndrome (CTS) is on the rise, warranting further workplace interventions.9 Of relevance is the fact that dentists do have a significant risk of disability due to MSD.10
4. Psychological: includes job stressors, conflict, task demands and leadership.
5. Ergonomic: Ergonomic hazards refer to strains on the worker's body that harm the musculoskeletal system due to improper design of workstation, equipment and surgery.11
A healthy workplace is one where all workers collaborate to promote and maintain health, safety and well-being in a good physical work environment. Thus, a worker will not only be free of workplace injuries but concerns about psychosocial work issues are reduced.12
Given the changing recognition that dental practitioners should work in environments that do not place unnecessary strain on their bodies and do not cause occupational health related issues, hence, this study was conducted to investigate the prevalence of occupational health- related conditions among dentists, dental therapists and oral hygienists in KwaZulu-Natal, South Africa.
The dental workforce involved with treating patients directly, in South Africa (SA), is comprised of dentists, dental therapists, and oral hygienists. For the purpose of this article, they will be referred to as oral health practitioners. Oral health practitioners provide oral health care services both in the public and private sectors in SA.
METHODS
This cross sectional, descriptive study was conducted in 2017. Ethical clearance was obtained from the Humanities & Social Sciences Research Ethics Committee at the University of KwaZulu-Natal-HSS/1490/015D. Participants were informed of the purpose and procedures in the study. Written consent was obtained from all participants and they were informed of their right to withdraw at any time from the study. Anonymity of participants was maintained throughout the study by assigning participant reference identity numbers instead of names.
A self-administered questionnaire was developed, comprising questions on demographic information, occupational health, psychosocial risk factors and work tasks and planning. The questionnaire was piloted among 10 practitioners and edited prior to use.
A complete list of all dentists, dental therapists and oral hygienists based in KwaZulu-Natal (KZN) was obtained from the Health Professions Council of South Africa (HPCSA). A link to the online questionnaire was emailed via QuestionPro to all practitioners on the respective registers. Following a poor initial response by the dentists to the online survey, an attempt was made to contact the dentists who were registered with the South African Dental Association (SADA). All practitioners were invited to participate in the study through email, telephone and in person contact visits through their practices. The final study population consisted of dentists (n=400), dental therapists (n= 172) and oral hygienists (n=115).
Data was exported from QuestionPro and analysed in SPSS version 24. Frequencies and means with standard deviations were calculated for categorical and continuous variables respectively. Chi square and the independent samples t-test were used for bivariate comparison of categorical and continuous variables and the dependent variable under study respectively. The accepted level of significance was 0.05 (α=0.05).
RESULTS
Demographic details
A sample total of 353 (55.7%) of the total population of 687 individuals responded to the questionnaire, consisting of 150 (42.5%) males and 203 (57.5%) females. The demographic characteristics are summarised in Table 1. A post-graduate degree was the highest qualification for 24.6% of the respondents.
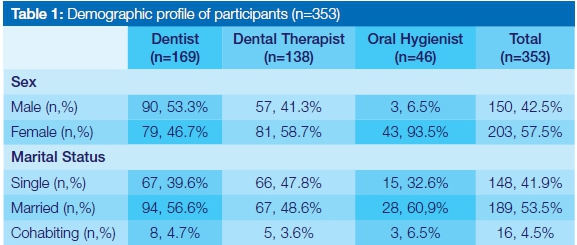
The response rates were 41% (n=169), 80% (n=138) and 40 % (n= 46) for dentists, dental therapists and oral hygienists respectively.
Chemical Exposures
Ten percent of the participants reported an allergy to latex, presenting as itchiness (n=15), redness (n=8), rashes (n=5), blistering (n=4), and sinusitis symptoms (n=3), with the highest prevalence being among dental therapists (18%).
Seventy five percent of practitioners (n=265) do not use amalgam in preference to resin based restorative materials in clinical practice. Indeed, 191 (54.1%) oral health practitioners stated that they never use amalgam while 26.1% (n=92) sometimes use it, 5.7% (n=20) often use it and 1.1% (n=4) always use it. Seventy-two percent of the participants did not have an amalgam trap in their practices. Of those using amalgam, the waste was disposed through waste recycling (n=26), bin (n=23), water or fixer in a bottle (n=55), drain (n=14), sharps container (n=8) and collected by company (n=8).
Biological Exposures
The majority of respondents 304 (86.1%) used a facemask during their work and 117 (33.1%) made use of an N95 mask. Thirty eight percent of the oral health practitioner never use extraction ventilation in their surgeries while 18% sometimes use it.
When asked about the reasons for PCIs the following were indicated: needle stick injuries (n= 64), elevators during extractions (n=15), patient moved (n=9), eye splash (n=9), bites by patients (n=5), rotating burs (n=4) and scaler injury (n=2).
Physical exposures
Nearly 93% of practitioners work in awkward postures. Nearly 50% sometimes work with their hands above elbow height. Nearly 95%, at some stage during the working day, remain in the same posture for prolonged periods (Table 2).
It was the oral hygienists who most frequently reported symptoms of MSD, reporting a prevalence of 70% and 56.5% for neck and hand pain respectively. Dentists complained of the highest prevalence of shoulder pain (55.8%) and of percutaneous injuries (42.3%) (Table 3).
The participants had consulted medical practitioners in many instances. A variety of reasons for the ailments had been offered.
For neck pain: muscle spasm (n= 24), muscle strain (n=17), posture (n=16), muscle stiffness (n=15), muscle tension (n= 15), poor cervical spondylosis (n=13), degeneration of discs (n=4), work related (n=4), fatigue (n=2), repetitive strain injury (n=2), pinched nerve (n=2), stress (n=2) and osteoarthritis (n=1). Twenty-six respondents (n= 26) did not seek medical attention, despite reporting discomfort.
For hand pain: carpal tunnel issues (n=20), pain and inflammation (n=14), fatigue (n=14), strain (n=12), arthritis (n = 10), tendonitis (n=7), stiffness (n=6), numbness (n= 6) and burning sensation (n=3). Thirty two sufferers did not seek medical attention.
For shoulder pain: muscle strain (n= 21), muscle spasm (n=16), posture related (n=13), stiffness (n=11), inflammation (n=9), fatigue (n=8), rotator cuff (n= 7), frozen shoulder (n= 4), stress (n= 4), repetitive strain injury (n=2), arthritis (n= 1), fibromyalgia (n= 1), spondylosis (n=1) and trigger points (n=1). Twenty nine respondents did not seek medical attention.
Significantly more female dentists (55.2%) reported shoulder complaints as compared with their male counterparts (44.8%) (p=0.024). There was significant association between the number of years in practice and neck complaints (p = 0.013) with the frequency increasing with age.
Psychological exposures
There was a significant relationship among dental therapists between the deadlines relating to their daily tasks and neck pain (p=0.05) and hand and wrist pain (p=0.00).
One third of the participants (n=116) (33.9%) confirmed they had the ability to influence the planning of their work tasks. Nearly 45% were always able to plan their daily tasks. Several (40.5%) perceived that they never have a heavy workload and rarely work over eight hours a day. (Table 4).
Ergonomic exposures
Bending and twisting the upper body while working was significantly associated with pain in the hands and wrists (p=0.05). Working in awkward postures was significantly associated with neck complaints (p=0.002), hand and wrist pain (p=0.015) and shoulder pain (p=0.001). Working in the same posture for prolonged periods was significantly associated with neck pain (p=0.027), neck complaints (p=0.003) and shoulder pain (p=0.02). For all participants, the data revealed significant relationships between gender and shoulder pain (p=0.05), the ability to determine daily tasks and hand pain (p=0,032), variation in clinical work and hand pain (p=0.013), bending and twisting and shoulder pain (p =0.01), awkward postures and neck complaint (p=0.001), awkward postures and hand and wrist complaints (p=0.05), awkward postures and shoulder complaints (p=0.001), same posture for prolonged periods and neck pain (p=0), same posture for prolonged periods and hand pain (p =0.05) and same posture for prolonged periods and shoulder complaints (p=0.003).
The other occupational health related conditions reported were lower back pain, depression, airway infections, headache, dry eyes, recurrent colds and flu, irritable bowel syndrome, knee problems, fibromyalgia, tennis elbow and trigger finger.
DISCUSSION
This research set out to find data on the prevalence of occupational health-related conditions among oral health practitioners in KwaZulu-Natal, South Africa. Information on the prevalence of neck, shoulder and hand pain was obtained together with possible reasons for the experience. Data on allergy, use of amalgam, use of mask, posture, work habits and ventilation were also gathered.
Nearly 74% of the sample were female. In another study conducted in KZN the male participants were more numerous than female (72.5%).13 In studies conducted among dental students in South African universities, the dominant gender was female in both Gauteng (74%) and in the Western Cape (65%),14,15 Female participation in a study on MSD prevalence conducted in SA was 34%.16 The data was different in the American study where 85% were male.6 Gender distribution showed 63% were female in a Brazilian study, in line with the results of this investigation.17 A quarter of the participants had a post graduate degree. The cohort of oral health practitioners was exercise conscious with almost 80 percent doing some form of exercise, in contrast to a report from the United Arab Emirates where more than half (61%) did not exercise regularly and 61% were male.18 Gender distribution in the profession in South Africa is changing with, 64% of dental graduates between 1985 and 2004 being male.19 The female to male ratios have also increased in South African universities.
Chemical exposures
The usage of dental amalgams is low among oral health practitioners in KZN and resin based restorative materials are preferred, hence the low prevalence of conditions due to amalgam use. The problem is with the method of disposal as the environmental factors are a cause for concern. A study conducted in Scotland emphasised that the urinary levels of mercury were four times higher in dentists than in the control subjects and the researchers suggested that safer handling, monitoring and disposal be implemented.34 The operator is exposed to mercury vapour which is absorbed by the skin and is inhaled, but these hazards can be avoided by proper handling.1 A 2006 study failed to find a correlation between blood levels and cytogenic damage in dentists exposed to mercury. Methyl mercury was detected in blood samples but this is not the type of mercury that is found in dental amalgam. Other sources of mercury may be more of a concern. Dietary consumption should not be overlooked.35 The current investigation found that 54.1% of participants never use dental amalgams while the others reported only rarely using the material as compared with the 62% of general dentists who reported using amalgams in a 2017 American study.6
The prevalence of allergy to latex was 10.4%, similar to the 8% reported in an Indian study.21 Flemish dentists reported a 22.5% prevalence of dental allergies of which nearly half were latex related, also presenting as pruritus, urticaria, eczema and asthma.36 Dental staff and students are intensive users of gloves which places them at risk to latex allergies. The type of gloves used in training sensitises students to latex allergy symptoms. Low protein non-powdered gloves were found to reduce the exposure to the latex allergen and to decrease airborne allergens.37,38 Rubber latex allergens were investigated in a South African study which found that only 20% of gloves analysed had the allergen content below the recommended threshold amount.39 Another study conducted in South African dental schools revealed similar results and considered that latex allergens posed an allergic health risk. In 2009 a study concluded that despite a global position to refrain from using latex, the use continues in the South African setting.40
Biological exposures
Percutaneous injuries were experienced by nearly 33% of the responding practitioners with dentists showing a prevalence of 43%. A prevalence of 36.8 % has been reported in Nigeria,32 of 42% in Romania41 and of 42% in the UAE.2 These levels places dental workers at risk of contracting HIV, Hepatitis B and Hepatitis C. The Hepatitis C virus is found in saliva and the danger is that no effective vaccination is available. The risks are greater if the source patient is positive. HIV found in the blood of patients poses minimal risk in dentistry when compared with Hepatitis. An oral health practitioner who is not vaccinated is at a higher risk of Hepatitis B virus infection, the exposure risk ranging from 0 to 30%, depending on the antigen level of the patient.42
Dental workers are exposed to bacteria, fungi and viruses found in saliva of their patients. In this study 54% of oral health practitioners reported not wearing the N95 mask, placing them at risk of infection. The N95 mask is recommended as health care workers are prone to blood borne pathogens and the N95 achieves a "high level of protection" including against meningitis and pneumonia.43 The aerosol between the patient and the clinician is a mix of flora of the oral environment. It is filled to levels higher than normal standard amounts with aerobic and anaerobic bacteria. To prevent the oral health practitioners from inhaling this potentially dangerous mist, a proper air filtration system is required to reduce contaminants in the air and to remove bacteria from circulation. Other effective measures are high performance suctions used in conjunction with a dental dam and an ultra violet light lamp to disinfect the air.4 Extraction ventilation should be considered by practitioners who do not have this operating in their surgeries. In this study only 31.3% of practitioners always use extraction ventilation, placing themselves and others at risk.
Physical exposures
The prevalence of neck pain reported by participants in this study was 65.8% with the hygienists showing a higher rate of 70%. Dental hygienists in Australia also reported a high prevalence of neck pain (85%).20 An Indian study found a high prevalence of neck pain amongst dentists (83%), higher than the present investigation which at 66% was higher than that of a Polish study (47%).21,22 Similar results were reported in a Queensland, Brisbane study (66.2%), Andhra Pradesh, India (52%) and Brazil (57.5%).23-25 Hand pain reported for hygienists (60.1%) in Australia closely approximates the results obtained in the current study.20 Nearly 60 % of dentists in this study had experienced hand pain in the last 12 months and the results obtained were much higher than the 29% prevalence in Poland,22 which was similar to results for dentists in Andhra Pradesh, India (26%) and Jordanian dentists (39%).24,28,29
A prevalence of shoulder pain (55.8%) was reported among the dentists and 47.5% by the hygienists. The prevalence for hygienists differed markedly from that reported among Australian hygienists at 70%.20 Dentists in KZN suffered more from shoulder pain than did Polish (20%), Jordanian (39%) and Indian dentists (29%),22,24,29 but less than those reporting in Queensland, Brisbane (66.2%).23 It may be that younger, less experienced dentists have a higher prevalence of MSD. The causes of neck pain are prolonged static postures, high loads on the trapezius muscle and forward bending. The forward leaning posture weakens the muscles in the shoulder causing rounding and pain.30,31
Back pain was not explored in this study but was reported as another occupational health-related condition. Back pain prevalence was at 47% in the Nigerian study.32 Australian hygienists reported a 68% prevalence.20 Lithuanian dentists appear particularly prone to back pain at a 91% prevalence,33 whilst a Jordanian study reported 56% of the participants suffered this problem.29
Females in this study were more prone to MSD and this was also seen in a study in the UAE.2 This could be due to females reporting more freely or possibly that surgeries and equipment are not designed for women. It may be of interest that a 2015 study showed that government workers suffered more from MSD than did private dentists. This phenomenon was not investigated in this study.21
Psychological exposures
Workload stress due to patients (42.2%) and long working hours (69.2%) has been reported.21 Working long hours was not an issue in the current investigation as only 9% of participants worked more than eight hours per day. Increase in MSD adds to the mental stress resulting in further strain.2,44 Stress levels rated by a group of dentists in Belgium on a VAS scale from 0 to 10 was 7 which indicated high stress levels.36 The practitioners in this study were in control of their workday as they could influence the pace of work, they could solve their day-to-day problems and were able to influence the tasks performed. Daily workloads and planning appointments can also assist in eliminating stress.
Ergonomic exposures
Neck position is critical in the prevention of MSD (65% prevalence of neck pain in this study). Forward head posture is common among dental workers as it improves visibility. This posture controls the muscles of the neck to support the head causing a tension neck syndrome, presenting symptoms, which include headache, pain in the neck, shoulders and inter-scapular muscles. The continuous contraction of these muscles leads to disc degeneration, rounding of the shoulders and rotator cuff impingement.26 It may have been ideal to have investigated the role of magnification loupes as their usage improves posture and thereby reduces neck pain as they prevent the practitioner from leaning forward. A recommendation from a study in 2007 was that loupes should be used from undergraduate level. The improved posture will decrease the occurrence of pain.27
In considering MSD and the associated pain, it is evident that that training in ergonomics should be included in the under-graduate curriculum and included in continuous professional development. The authors of a paper which reported that only 30% of dentists and 23.2% of orthodontists had received some sort of ergonomics training, went on to recommend that dental students be taught intervention measures to reduce the prevalence of MSD.23
Study limitations
The limitation of this study was that it was self-reported and thus information bias could have affected the results. Participants could have either under- or over- reported their symptoms. In addition there may have been an element of participation bias as participation was voluntary. Individuals who were well may not have participated and so the results may indicate a prevalence higher than is the true state of occupational health-related symptoms and disease in this population.
CONCLUSION
Occupational health-related conditions remain a problem in dentistry. MSD and PCI are preventable and with education and training, including CPD, the burden can be reduced. More research into the ergonomics of dental practice needs to be conducted and filtered down to oral health practitioners via CPD courses. Further research into the causes of MSD is required and a need for intervention studies in this area to help reduce the prevalence is needed. Mercury handling needs to be improved with a focus on disposal of amalgam waste. Research into newer dental materials and amalgam replacement material is indicated. Dental training and student supervision should include the prevention of occupational health-related conditions. More qualitative studies should be conducted into dental education and occupational health.
ACRONYMS
MSD: musculoskeletal disorders
PCI: percutaneous injuries
References
1. Chopra, S, Pandey, S. Occupational hazards among dental surgeons. Medical Journal Armed Forces India 2007;63:23-25. [ Links ]
2. Al-Ali, K, Hashim, R. Occupational health problems of dentists in the United Arab Emirates. International Dental Journal 2012;62:52-6 . [ Links ]
3. Ayatollahi, J, Ayatollahi, A, Bagher M, et al. Occupational hazards to dental staff. Dent Res J (Isfahan) 2012;9:2-7. [ Links ]
4. Szymanska, J. Dental bioaerosol as an occupational hazard in a dentist's workplace. Annals of Agricultural and Environmental Medicine 2007;14:203-7. [ Links ]
5. World Health Organisation. Elemental Mercury and Inorganic Mercury Compounds: Human Health Aspects. (2003). [ Links ]
6. Bakhurji, E, Scott, T, Mangione, T, Sohn, W. Dentists' perspective about dental amalgam: current use and future direction. Journal of Public Health Dentistry 2017;77(3):207-15. [ Links ]
7. Buckle, P. W. & Devereux, J. J. The nature of work-related neck and upper limb musculoskeletal disorders. Applied Ergonomics 2002;33:207-17. [ Links ]
8. World Health Organisation. Preventing musculoskeletal disorders in the workplace. 2011. [ Links ]
9. Bhattacharya, A. Costs of occupational musculoskeletal disorders (MSDs) in the United States. International Journal of Industrial Ergonomics 2014;44:448-54, doi:http://dx.doi.org/10.1016/j.ergon.2014.01.008. [ Links ]
10. Cherniack, M, Dussetschleger, J, Bjor, B. Musculoskeletal disease and disability in dentists. Work 2010;35:411-8. [ Links ]
11. Gupta, A, Ankola, AV, Hebbal, M. Dental ergonomics to combat musculoskeletal disorders: a review. International Journal of Occupational Safety and Ergonomics 2013;19:561-71. [ Links ]
12. World Health Organisation. Healthy Workplaces: A Model for Action: for Employers, Workers, Policy-Makers and Practitioners. (2010). [ Links ]
13. Moodley, R, Naidoo, S. The prevalence of musculoskeletal disorders among dentists in KwaZulu-Natal. South African Dental Journal 2015;70:98-103. [ Links ]
14. Bhayat, A, Madiba, TK. The self-perceived sources of stress among dental students at a South African Dental School and their methods of coping. South African Dental Journal 2017;72:6-10. [ Links ]
15. Wilson, V, Rayner, CA, Gordon NA, et al. Perceived stress among dental students at the University of the Western Cape. South African Dental Journal 2015;70:255-9. [ Links ]
16. Botha, P, Chikte, U, Esterhuizen, T, Barrie, R. Self-reported musculoskeletal pain among dentists in South Africa: A 12-month prevalence study. South African Dental Journal 2014 69:208-13. [ Links ]
17. Bellissimo-Rodrigues, WT, Bellissimo-Rodrigues, F, Machado, AA. Infection control practices among a cohort of Brazilian dentists. International Dental Journal 2009;59:53-8 [ Links ]
18. Hashim, R, Al-Ali, K. Health of dentists in United Arab Emirates. International Dental Journal 201;63:26-9. [ Links ]
19. Hons, BM, et al. Gender and race distribution of dental graduates (1985-2004) and first year dental students (2000-2005) in South Africa. South African Dental Journal 2005;60:206-9. [ Links ]
20. Hayes, MJ, Smith, DR, Taylor, JA. Musculoskeletal disorders and symptom severity among Australian dental hygienists. BMC Research Notes 2013;6:250. [ Links ]
21. Reddy, V, Bennadi, D, Satish, Gura, U. Occupational hazards among dentists: a descriptive study. Journal of Oral Hygiene & Health 2015. 3:185.doi:10.4172/2323-0702.1000185. [ Links ]
22. Kierklo, A, Kobus, A, Jaworska, M, Botulinski, B. Work-related muculoskeletal disorders among dentists-a questionnaire survey. Annals of Agricultural and Environmental Medicine 2011;18(1):79-84. [ Links ]
23. Sakzewski, L, Naser-ud-Din, S. Work-related musculoskeletal disorders in Australian dentists and orthodontists: risk assessment and prevention. Work 201;52:559-79. [ Links ]
24. Muralidharan, D, Fareed, N, Shanthi, M. Musculoskeletal disorders among dental practitioners: does it affect practice? Epidemiology Research International 2013 vol 2013Article 716897, 6 pages, 2013.doi 10.1155/2013/716897. [ Links ]
25. Alexandre, PCB, da Silva ICM, da Souza, LMG, et al. Musculoskeletal disorders among Brazilian dentists. Archives of Environmental and Occupational Health 2011;66:231-5. [ Links ]
26. Bhandari, S, Bhandari, R, Uppal, R, Grover, D. Musculo-skeletal disorders in clinical dentistry and their prevention. Journal of Orofacial Research 2013;3:106-14. [ Links ]
27. Maillet, J, Millar, M, Burke, JM, et al. Effect of magnification loupes on dental hygiene student posture. Journal of Dental Education 2008;72:133-44. [ Links ]
28. Toohey, S. Designing Courses for Higher Education. Buckingham, Open University Press, London, 1999. [ Links ]
29. Barghout, NH, Al-Habashneh, R, Al-Omiri, MK. Risk factors and prevalence of musculoskeletal disorders among Jordanian dentists. Jordan Medical Journal 2011;45(2): 195-204. [ Links ]
30. Leggat, P A, Smith, DR. Musculoskeletal disorders self-reported by dentists in Queensland, Australia. Australian Dental Journal 2006;51:324-7. [ Links ]
31. Biswas, R, Sachdev, V, Jindal, V, Ralhan, S. Musculoskeletal disorders and ergonomic risk factors in dental practice. Indian J Dent Pract 2001;4:70-4. [ Links ]
32. Fasunloro, A, Owotade, FJ. Occupational hazards among clinical dental staff. J Contemp Dent Pract 2004; 5:134-52. [ Links ]
33. Puriene, A, Aleksejuniene, J, Petrauskiene, J, Balciuniene, I, Janulyte, V. Self-reported occupational health issues among Lithuanian dentists. Industrial Health 2008;46:369-74. [ Links ]
34. Ritchie, K, Burke, FJT, Gilmour, WH, et al. Mercury vapour levels in dental practices and body mercury levels of dentists and controls. British Dental Journal 2004;197:625-32. [ Links ]
35. Atesagaoglu, A, Omurlu, H, Ozcagli, E, Sardas, S, Ertas, N. Mercury exposure in dental practice. Operative Dentistry 2006;31:666-9. [ Links ]
36. Gijbels, F, Jacobs, R, Princen, K, Nackaerts, O, Debruyne, F. Potential occupational health problems for dentists in Flanders, Belgium. Clinical Oral Investigations 2006;10:8-16. [ Links ]
37. Tarlo, SM, Sussman, GL, Holness, DL. Latex sensitivity in dental students and staff: a cross-sectional study. Journal of Allergy and Clinical Immunology 1997;99:396-400. [ Links ]
38. Carrozzi, F, Katelaris, C, Burke, T, Widmer, R. Minimizing the risks of latex allergy: The effectivness of written information. Australian Dental Journal 2002;47:237-40. [ Links ]
39. Ratshikhopha, ME, Singh, TS, Jones, D, Jeebhay, MF, Lopata, AL. High concentrations of natural rubber latex allergens in gloves used by laboratory health personnel in South Africa. South African Medical Journal 2015;105:43-6. [ Links ]
40. Mabe, DO, Bello, B, Singh, T, et al. Allergenicity of latex rubber products used in South African dental schools. SAMJ: South African Medical Journal 2009;99:672-4. [ Links ]
41. Bârlean, L, Dănilă, I, Săveanu, I, Balcoş, C. Occupational health problems among dentists in Moldavian Region of Romania. Revista Medico-chirurgicala a Societatii de Medici si Naturalisti din Iasi 201;117:784-8. [ Links ]
42. Gupta, N, Tak, J. Needlestick injuries in Dentistry. Kathmandu University Medical Journal 2012; 9:208-12. [ Links ]
43. Benson, SM, Novak, DA, Ogg, MJ. Proper use of surgical n95 respirators and surgical masks in the OR. Journal of the Association of periOperative Registered Nurses (AORN) 2013; 97: 457-67. [ Links ]
44. Rada, RE, Johnson-Leong, C. Stress, burnout, anxiety and depression among dentists. The Journal of the American Dental Association 2004;135:788-94. [ Links ]
 Correspondence:
Correspondence:
Rajeshree Moodley
Discipline of Dentistry, School of Health Sciences
University of KwaZulu-Natal
South Africa.
Tel: +27 31 260 8871.
E-mail: moodleyra@ukzn.ac.za














