Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.72 n.4 Johannesburg May. 2017
RESEARCH
An education intervention to improve oral health knowledge and behaviour in learners: A cluster randomized controlled trial
N NiranjanI; S KnightII
IManager of Coding and Nomenclature, SADA
IIPublic Health Medicine Physician and Senior Lecturer, Discipline of Public Health Medicine, School of Nursing and Public Health, College of Health Sciences, University of KwaZulu Natal, Durban, South Africa
ABSTRACT
INTRODUCTION: Preventive dental services are required to reduce the burden of caries and oral disease in children.
OBJECTIVE: To assess the efficacy of three, as opposed to one, oral health education lessons in influencing the oral health related behaviour and knowledge in Grade 5 learners.
STUDY DESIGN: Cluster randomized controlled trial.
METHODS: Participants: Ten public primary schools (5 intervention, 5 control) in Verulam; 337 grade 5 learners in each arm. Control arm: Viewing of an oral health education video. Intervention arm: As above repeated at three month intervals over nine months. Randomisation: At cluster level; schools randomly assigned to intervention and control arm after consent was obtained from individual participants; therefore participants remained blinded to which arm of the study they were assigned.
RESULTS: A significant improvement in oral health knowledge and practice was noted for both groups after the intervention (p < 0.05). However, the intervention group returned significantly better results compared with the control for all categories except toothbrush ownership, brushing frequency and knowledge of when to replace toothbrushes.
CONCLUSION: Repeated education resulted in significant improvements in the knowledge and oral health behaviour of learners compared with the responses after one oral health lesson.
INTRODUCTION
Dental caries is the most common childhood disease, affecting between 60 and 90% of all five-year olds throughout the world, negatively impacting on the quality of life of the child, restricting activities, reducing ability to learn and increasing the frequency of absenteeism from schools.1,2 Children with caries may need emergency dental visits or even hospitalization, which impacts on the parents' financial wellbeing, including time taken off work.2
The shortage of oral health professionals and fully equipped dental facilities in the public sector limits the availability of treatment services.3 Emergency relief of pain and sepsis is the most commonly performed clinical procedure at primary oral health care facilities.3,4 The burden of unmet treatment need can be significantly lowered by efforts to promote oral health and prevent the development of caries.4 Insufficient emphasis is placed on basic primary preventative oral health care and oral health education which would reduce the need for curative treatment among children at primary school age.3 In 2001, the South African (SA) Department of Health (DoH) proposed that at least 50% of all primary schools should be participants in organized preventive programmes by 2004.5 However, school-based oral health education programmes are erratic in distribution and implementation, and lack regular follow up and formal evaluation.3,6
According to data of the Health Professions Council of South Africa (HPCSA) there were 5320 registered dentists in 2010, but only 828 (15%) were working in the public sector.5,7,8 However, only 9.7 million (18%) of the 51 million people in SA9 were insured by private medical aids and therefore had access to private dental care.10,11 Most South Africans then are obliged to rely on the public sector for dental care, with a ratio of 1 dentist per 50 000 population compared with 1 dentist per 1800 population in the private sector.8 The inequitable distribution of dentists exacerbates the severity of the impact on the community of oral disease.4
High income countries that have invested in preventive dental services have shown a reduction in the prevalence of oral disease and consequently report savings in curative dental expenditure.12,13 Most low and middle income countries (LMICs) however have made less investment in oral health care and resources are primarily allocated to emergency relief of pain related to oral disease.14 In some LMICs it is estimated that the cost of conservative treatment of dental caries alone would exceed the total health care budget available for children.15 Poor communities are unlikely to prioritize oral health care unless adequately educated on the associated values and benefits.16
In SA, school attendance is compulsory from grade 1 to 9, or until age 15 years. School enrolment in grades 1 to 7 in 2012 was 99% of children of eligible age.17 The classroom therefore provides an ideal platform to deliver oral health education.17 Scholars are the most receptive age-group when seeking to improve sustainable oral health related behaviours.18 The earlier these habits are instilled, the more likely they are to last life-long.13,18 However, oral health messages need to be reinforced if a long lasting impact is to be ensured.13,18 Learners are also important channels for the further dissemination of health promotion messages to their families and community.13 A single oral health education intervention by a dentist or oral health worker was shown to improve oral hygiene practice for up to six months.1,19,20
The purpose of this study is to assess the efficacy of reinforced oral health education lessons on oral health related behaviour and knowledge in grade 5 learners as opposed to the effect of a single oral health education lesson.
METHODS
A cluster randomized controlled trial was used in government-funded primary schools in the town of Verulam, South Africa.
Multi-stage sampling was conducted. A simple random sample of 10 of the 13 eligible schools was chosen. The principals of these 10 selected schools provided 'gate-keeper' permission for participation in the study. The sample was then randomised to five intervention and five control schools. All schools had either two or three Grade 5 classes. In schools with two Grade 5 classes, both classes were enrolled, and in schools with three Grade 5 classes, two of these were randomly selected. Age and sex were not selection criteria.
A total of 339 learners from five schools were enrolled into the control group and 337 learners from five schools comprised the intervention group.
The minimum effective sample size required for this cluster randomized trial to retain equivalent power to an individually randomized trial was 628. The intra-class correlation coefficient (determined from the pilot study) and the average cluster size were used to calculate the design effect. The effective sample size was calculated by dividing the total possible number that could be enrolled into the study by the design effect.21
Intervention
The grade 5 learners of the five intervention schools were instructed on basic oral health education by viewing a five minute video produced by Colgate®, covering instruction on correct brushing and flossing techniques, basic knowledge on toothpaste use, when and how often to brush, when to replace toothbrushes and when to visit a dentist. The video was screened on a television set or a projector was used, depending on the school's facilities. Either the investigator or the teacher handled the projection as no special skills or training were required for this method of administering oral health education. In the intervention group, the video showing was repeated at three month intervals over a period of nine months; i.e. August 2013, November 2013 and February 2014. A register was taken on each intervention day to ensure all enrolled learners were present at every screening of the video.
Learners in the control schools received instruction on oral health education, via the same video, once only at the start of the study.
No discussion was held following any viewing of the video to avoid any bias.
Data collection
The same standardized, anonymous questionnaire was used at baseline and at the end of the study (nine months later) for both the control and intervention groups to collect data on basic demographics of learners, oral health knowledge and practices. Pre-intervention data was collected from both groups in August 2013 and post-intervention data was gathered in May 2014. The intervention group exposed to repeated viewing received the last intervention in February 2014.
Data analysis
Nominal and categorical data were captured and analysed using Microsoft Excel. Frequencies for demographic variables, oral health knowledge and behaviour were calculated. Outcomes were measured as the mean difference between groups (mean of control schools post intervention minus mean of intervention schools post intervention). The paired t test was used to assess whether any of the mean differences between the control and intervention for each variable were statistically significant (p < 0.05).
Ethical considerations and permissions
The Biomedical Research Ethics Committee of the University of KwaZulu-Natal granted ethical approval for the study (BE308/12). Authority was obtained from the KwaZulu-Natal Department of Education to approach the principals of selected schools to seek their 'gate-keeper' permission for their schools to participate in the study. Parents/guardians of all learners from the selected classes were sent participant information letters explaining the nature and purpose of the study prior to commencement of the study. Learners who returned signed consent from their parents were enrolled. Consent was obtained prior to allocation therefore ensuring concealment of randomization. All learners in the selected classes provided verbal assent to participate in the study.
RESULTS
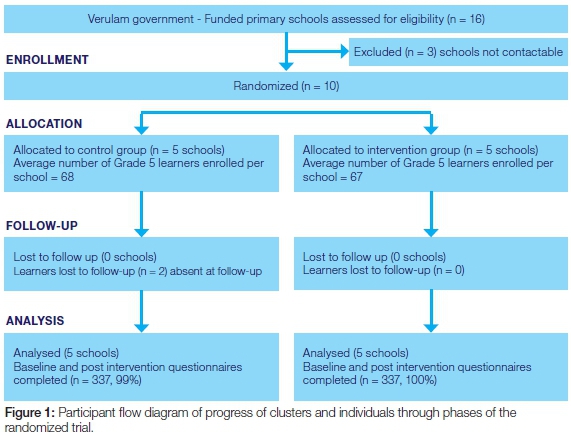
The study sample comprised 676 learners from Grade 5 classes in ten primary schools, enrolled from amongst a total of 1075 learners in 13 eligible schools in the study area. Two learners from the control were lost to follow up due to non-attendance on the intervention day. There was no loss to follow up in the intervention group. The final analysed study sample consisted of 674 learners, 337 control and 337 intervention, and these numbers were commensurate with the minimum effective sample size (Figure 1).
The baseline characteristics of the 337 participants in the control and 337 participants intervention group were compared (Table 1). There were 169 (51%) females analyzed in the control group from five schools and 188 (56%) females in the intervention group from five schools. There was no significant difference in gender distribution between the control and intervention groups (p = 0.12).
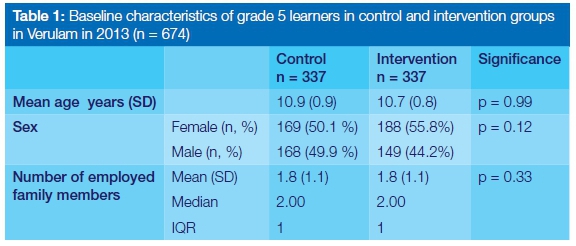
The age range of learners in Grade 5 at baseline in the control group was from 10 to 14 years and from 9 to 14 years in the intervention group. The mean age of learners was 10.9 (SD 0.9) years in the control group and 10.7 (SD 0.8) years in the intervention group with a median of 11 years for both groups. There was no statistical difference in age between groups (p = 0.99).
Learners reported on the number of employed family members in their homes as a crude measure of economic background. There was no statistical difference between the groups at the start of the study, p = 0.33, with a mean of 1.8 (SD 1.1) employed householders and a median of two.
Learners' oral health practices and knowledge were compared pre- and post-intervention and between the control and intervention groups at the end of the study (Table 2). At the start of the study, 326 (96%) learners from the control group and 315 (93.5%) of the intervention group owned their own toothbrush. Significantly more learners owned their own toothbrush at the end of the study in both groups (p = 0.02 for control and p < 0.01 for intervention). There was no significant difference in toothbrush ownership between the control and intervention at the end of the study (p = 0.15).
In the control group 281 (83%) of learners reported brushing their teeth daily, 55 (16%) brushed occasionally and 3 (0.9%) did not brush. The control showed significant improvement in brushing practice after intervention with 293 (86%) brushing daily, 44 (13%) brushing occasionally and 2 (0.6%) never brushing (p < 0.01). At the start of the study in the intervention group 277 (82%) brushed daily, 51 (15%) brushed occasionally and 9 (2.7%) did not brush, while after the intervention 328 (97%) brushed daily, 9 (2.7%) brushed occasionally and none reported never brushing (p < 0.01). The intervention group showed significantly better brushing practice habits post-intervention compared with the control group (p < 0.01).
At the start of the study, 257 (76%) learners from the control and 273 (81%) from the intervention knew they should be brushing twice daily, however only 224 (66%) from the control and 207 (61%) from the intervention actually performed the ritual. At the end of the study significantly (p < 0.01) more learners in both groups were aware and actually practiced twice daily brushing, than at the beginning. There was no significant difference between the groups regarding frequency of brushing practice at the end of the study (p = 0.28), however in the intervention group significantly (p < 0.01) more learners knew at the end of the study how often they should brush compared with the control.
Both groups revealed significant improvement in knowledge of brushing duration after intervention (p < 0.01), and the intervention group had significantly better results compared with the control (p < 0.01).
With regard to brushing technique, both groups showed significantly better knowledge of the correct technique as compared with the start of the study (p < 0.01) and the intervention group recorded significantly better results than did the control group (p < 0.01).
At the start of the study 96 from the control and 103 from the intervention knew how to floss. After the intervention, 189 from the control and 336 from the intervention knew the technique (p < 0.01), the intervention group having significantly better results than the control (p < 0.01). Significantly (p<0.01) more learners from the intervention group possessed floss at the end of the study compared with the control. Both groups showed significantly more learners flossing than at the start of the study (p < 0.01 for both groups), whilst the intervention group had significantly more learners flossing than the control, post-intervention (p < 0.01).
Both groups showed significant improvement in knowledge as to when to replace their toothbrushes compared with pre-intervention (p < 0.01 for both). There was no significant difference between the two groups at the end of the study (p = 0.05).
After the intervention significantly more learners in the intervention group 272 (80.7%) compared with the control 176 (51.9%) knew the correct amount of toothpaste to apply when brushing (p < 0.01). In the intervention group, significantly (p < 0.01) more (91% vs. 59%) learners knew how often they should visit a dentist compared with the controls at the end of the study.
DISCUSSION
In South Africa, the vast majority of the population (84%) rely on public services for dental care.22 However, due to poorly distributed and inadequately equipped facilities, dental treatment is generally limited to emergency relief of pain and sepsis.4 Given that situation, it becomes important to enhance efforts to reduce the incidence of dental caries by implementing preventive oral health education and care programmes.4,6,23 The school environment encourages the development of life skills, self-esteem and improved health-related behaviour and is an apt setting for oral health promotion in children.23-25 The DoH did set a goal that 50% of all schools should receive oral health promotion programmes by 2004.5 However subsequent studies reported that such programmes have been fragmented and lacked proper evaluation for appropriateness was lacking.1,3,4,6
The study used a strategy of randomized cluster sampling. Ideally in randomized controlled trials, clusters of children should be as diverse as possible while still remaining representative of the general child population.26 In this study participants were enrolled based on their schools and therefore the cluster sampling technique allowed for convenience, reducing time and costs. The approach also prevented potential bias arising from contamination of samples where intervention participants may interact with control participants in discussing their experiences of the study. There was no significant difference between the groups regarding age, sex and economic background. All learners were between the ages of 9 and 14 as expected of learners in grade 5. There were slightly more girls (52%) in the study than boys which is commensurate with the population statistics in SA.27
In this study both groups received oral health education. The objective was to measure whether repeated oral health education (intervention) would result in greater improvement in knowledge and oral health behaviour than after a single oral health education experience (control). The results of this study showed that both groups benefitted significantly from oral health education, however the group that received repeated oral health education demonstrated significantly greater improvements in oral health knowledge and practices for most categories that were investigated in the study, thus confirming the hypothesis. Categories of assessment that did not reflect significant difference from the control were knowledge of when to replace toothbrushes, ownership of toothbrushes and frequency of daily brushing. This can be attributed to marketing and advertising from both toothbrush and toothpaste manufacturers making such information widely accessible and therefore confounding results. Both groups had poor knowledge regarding oral hygiene techniques at the start of the study and both improved in knowledge after the intervention. However repeated oral health education resulted in over 40% more learners than the control group knowing the correct brushing and flossing techniques. This is commensurate with the results of studies assessing the effect of health promoting schools on oral health indicators compared with non-supportive schools.23,28 (A health promoting school (HPS) is defined as "one that constantly strengthens its capacity as a healthy setting for living, learning and working".)25 In these studies, oral health education was given repeatedly and resulted in better knowledge and brushing habits and consequently a reduced caries incidence.23,28
Information related to correct tooth-brushing and flossing techniques are not as frequently or well described in the media and advertising and hence the most significant effects of the study are evidenced in these outcomes.
STUDY LIMITATIONS
The measurement instrument in this study is self-reported behaviour. As there were no oral examinations conducted on learners, there is no evidence that the improvements noted in oral health knowledge are causally associated with better oral hygiene as assessed by plaque and bleeding indices or a reduction in untreated caries. Oral health promotion in this circumstance was conducted in isolation and not in collaboration with general health promotion. No measure of cognitive abilities of participants was assessed at the start of the study. It was assumed that all participants would be of similar cognitive function having passed the previous grade.
CONCLUSION AND RECOMMENDATIONS
The study provides clear evidence that repeated oral health education results in improved oral health knowledge and behaviour; however the effect on caries status and oral hygiene has not been clinically assessed. Future studies should include oral examinations in testing the efficacy of different intervention strategies. Oral health promotion should be included as part of general health promotion. The results of this study are also encouraging in that the method of oral health education delivery allows the opportunity for task shifting, although this was not the objective of the study. This is useful given the scarcity of dental manpower resources in the public sector in SA.
An inference may be drawn from the study that the World Health Organization's HPS model may be a promising concept for implementation in South African primary schools as it recognizes the need for continued support through education, creation of a healthy environment and provision of health services.18,25,28
ACRONYMS
DoH: Department of Health
HPS: Health Promoting School
LMICs: low and middle income countries
References
1. Cooper AM. Primary school-based behavioural interventions for preventing caries. Cochrane Collab. 2011;(5):1-47. doi:10.1002/14651858.CD009378. [ Links ]
2. Sheiham A. Early childhood caries and overall health. Br Dent J. 2006;(201):625-6. [ Links ]
3. Singh S, Myburgh N, Lalloo R. Policy analysis of oral health promotion in South Africa. Glob Health Promot. 2010;17(1):16-24. [ Links ]
4. Singh S. Dental caries rates in South Africa : implications for oral health planning. South African J Epidemiol Infect. 2011;26(4):259-61. [ Links ]
5. South African National Oral Health Strategy. Department of Health. http://www.doh.gov.za/docs/policy/norms/full-norms.html#oral. Published 2010. Accessed April 10, 2012. [ Links ]
6. Petersen PE, Kwan S. Evaluation of community-based oral health promotion and oral disease prevention--WHO recommendations for improved evidence in public health practice. Community Dent Health. 2004;21(4 Suppl):319-29. [ Links ]
7. Health Professions Council of South Africa. HPCSA. http://www.hpcsa.co.za/ Local copy: /indicators/HumanResources/HPCSA/. Published 2014. Accessed July 25, 2014. [ Links ]
8. HRH Strategy for the Health Sector 2012/12-2016/17. Department of Health. http://www.doh.gov.za/docs/stratdoc1/2012/hrhstrat.pdf. Published 2012. Accessed July 12, 2015. [ Links ]
9. Census 2011 Statistical release - P03014,. Statistics South Africa. http://www.statssa.gov.za/publications/P03014/P03014.pdf. Published 2012. Accessed July 12, 2015. [ Links ]
10. General Household Survey 2013 Statistical Release - P0318. Statistics South Africa. http://www.statssa.gov.za/publications/P0318/P0318.pdf. Published 2014. Accessed July 12, 2015. [ Links ]
11. Econex. The South African Private Healthcare Sector: Role And Contribution To The Economy; 2013. [ Links ]
12. Postma T, Ayo-Yusuf O, Wyk PJ Van. Socio-demographic correlates of early childhood caries prevalence and severity in a developing country - South Africa. Int Dent J. 2008;(58):91-7. [ Links ]
13. Benzian H, Hobdell M, Mackay J. Hit or miss: a window of opportunity for global oral health. Br Dent J. 2011;210(4):147. [ Links ]
14. Ritchie CS, Joshipura K, Hung H, Douglass CW. Nutrition as a mediator in the relation between oral and systemic disease: associations between specific measures of adult oral health and nutrition outcomes. Crit Rev Oral Biol Med. 2002;13(3):291-300. doi:10.1177/154411130201300306. [ Links ]
15. Petersen PE, Kwan S. Evaluation of community based oral health promotion and oral disease prevention Report of a workshop convened at World Health Organisation (WHO) Headquarters, World Heal Organ. 2004;(June 2003):19-20. [ Links ]
16. Dye BA, Thornton-Evans G. Trends in oral health by poverty status as measured by Healthy People 2010 Objectives. Public Health Rep. 2010;125(6):817-830. doi:10.2307/41434848. [ Links ]
17. Department of Education. Education Statistics in South Africa. Department of Education. http://www.education.gov.za/EMIS/StatisticalPublications/tabid/462/Default.aspx. Accessed April 8, 2014. [ Links ]
18. Jurgensen N, Petersen PE. Promoting oral health of children through schools - Results from a WHO global survey 2012. Community Dent Health. 2013;30:204-18. [ Links ]
19. Watt RG, Marinho V. Does oral health promotion improve oral hygiene and gingival health? Periodontol 2000. 2005;(37):35-47. [ Links ]
20. Friel S, Hope A, Kelleher C. Impact evaluation of an oral health intervention amongst primary school children in Ireland. Health Promot Int. 2002;17(2):119-126. http://heapro.oxfordjournals.org/content/17/2/119.short. [ Links ]
21. Donner A, Klar N. Pitfalls of and controversies in, cluster randomization trials. Am J Public Health. 2004;94(3):416-22. doi:https://doi.org/10.2105/AJPH.94.3.416. [ Links ]
22. Council for Medical Schemes. The Council for Medical Schemes Annual Report 2014/2015. CMS. https://www.medicalschemes.com/files/AnnualReports/AR2014_2015.pdf. Published 2016. Accessed December 21, 2016. [ Links ]
23. Moysés ST, Moysés SJ, Watt RG, Sheiham A. Associations between health promoting schools' policies and indicators of oral health in Brazil. Health Promot Int. 2003;18(3):209-18. [ Links ]
24. Habbu S, Krishnappa P. Effectiveness of oral health education in children - a systematic review of current evidence (2005 -2011). Int Dent J. 2015;(65):57-64. [ Links ]
25. School and Youth Health. World Health Organisation. http://www.who.int/school_youth_health/gshi/hps/en/. Published 2015. Accessed August 12, 2015. [ Links ]
26. Katzenellenbogen J, Joubert G, Abdool Karim S. Epidemiology: A Manual for South Africa. 1st ed. Cape Town: Oxford University Press; 1997. [ Links ]
27. Mid-year population estimates 2011 - P0302,. Statistics South Africa. http://www.statssa.gov.za/publications/P0302/P03022011.pdf. Published 2012. Accessed August 11, 2015. [ Links ]
28. Petersen PE, Peng B, Tai B, Bian Z, Fan M. Effect of a school-based oral health education programme in Wuhan City, Peoples Republic of China. Int Dent J. 2004;(54):33-41. [ Links ]
 Correspondence:
Correspondence:
Nirvada Niranjan:
Cell: 084 555 6581
E-mail: nniranjan@sada.co.za














