Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.72 n.2 Johannesburg Mar. 2017
RADIOLOGY
Maxillo-facial radiology case 148
CJ Nortjé
BChD, PhD, ABOMR, DSc. Faculty of Dentistry, University of the western Cape. E-mail: cnortje@uwc.ac.za
A 17 year -old female patient (Fig 1) who suffered from renal osteodystrophy, presented for routine dental treatment. Medical history revealed that at the age of six years she had suffered progressive failure of eyesight. A renal biopsy performed in 1975 was diagnosed as medullary cystic disease with progressive glomerular sclerosis. Treatment at that stage was refused and the patient attended the Dental Hospital only in 1979.

INTERPRETATION
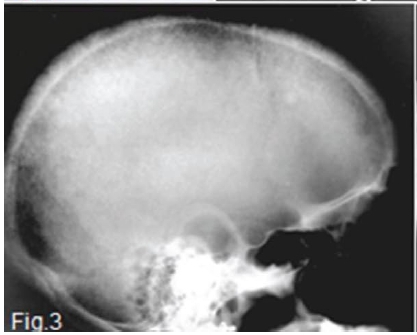
A diagnosis of secondary hyperparathyroidism was made. Her blood picture at the time was as follows: serum calcium within normal limits, urea increased 7-fold, creatinine 13-fold and alkaline phosphatase 7-fold. The pantomograph (Fig. 2) shows generalized relative rarefaction of the jawbones and absence of the lamina dura around the teeth giving the roots a tapered appearance. A unilocular radiolucency (red arrow) is discernible distal to the lower left 2nd molar tooth in the mandible, suggestive of a brown tumour. The skull radiograph (Fig. 3) shows a generalized granular appearance. The radiopaque outlines of the maxillary sinus are not discernible. (Figs 2 and 3). Figure 4 shows granularity of trabecular pattern in bones of the hand and wrist and subperiosteal erosion of the cortex (green arrow), especially in the mid phalanges, and erosion of the terminal tufts (yellow arrow).A biopsy specimen was taken from the mandibular radiolucent area. Microscopic examination revealed a cellular fibrous lesion containing irregular trabecular bone and a few scattered multinucleated giant cells. With the available clinical data a diagnosis of a brown tumour of secondary hyperparathyroidism was made.


Chronic renal failure is the most common cause of secondary hyperparathyroidism. Failing kidneys do not convert enough vitamin D to its active form, and do not adequately excrete phosphate. When this happens, calcium is taken up from the circulation and insoluble calcium phosphate forms in the body. Both processes lead to hypocalcaemia and hence secondary hyperparathyroidism. The condition can also result from malabsorption (chronic pancreatitis, small bowel disease, malabsorption-dependent bariatric surgery) in that the fat-soluble vitamin D cannot be reabsorbed. This leads to hypocalcaemia and a subsequent increase in parathyroid hormone secretion in an attempt to increase the serum calcium levels. The bone changes of secondary hyperparathyroidism are identical to those found in primary hyperparathyroidism.
Reference
1. Phillips VM, Breytenbach HS, Grotepass FW, Nortje CJ, van Wyk CW & van Buuren AJ.Secondary hyperparathyroidism. SADA, 1982; 37:373-375 [ Links ]














