Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.72 n.1 Johannesburg Feb. 2017
INSIGHTS
Insights into the clinical effectiveness of whitening products. Part 2 Dentist-supervised-at-home LED gel bleaching product
SR GroblerI; Y OsmanII
IBSc, BSc (Hons), MSc (Phys Chem), PhD (Dent), DSc (Anal Chem). Oral and Dental Research Institute, Faculty of Dentistry, University of the Western Cape, Tygerberg, Cape Town, South Africa
IIBChD, MChD, Hons BBA, MBA, PGDHM. Oral and Dental Research Institute, Faculty of Dentistry, University of the Western Cape, Tygerberg, Cape Town, South Africa
ABSTRACT
This section of the report is about the success of a dentist-supervised-at home LED gel tooth whitener, giving the results of a clinical study. The product (LED light gel with 44% carbamide peroxide) was applied by the dentist on teeth 11 and 21 in the chair for 10 minutes. The process was repeated three times, followed by an at-home treatment period (30 minutes/day) of 14 days with 35% carbamide peroxide. The treatment was as outlined by the manufacturers. The L* value improved (more white) after the in-chair treatment with the LED system but showed no further significant increase after the 14 day at-home treatment. However, the b* value improved (less yellow), after both the LED treatment and 14 day at-home treatment. The a* value did not improve significantly throughout the treatments. The LED system provides in-chair tooth whitening after a 14 day treatment although not as effectively as does Opalescence.
INTRODUCTION
Tooth whitening or bleaching has become more in demand in the past decade and several methods have been developed. One practised for many years, before the modern peroxide methods, was the use of fine ash to polish/clean teeth to make them cleaner and whiter. Today, tooth whitening can be over-the-counter bleaching (self-administered), in-office bleaching (professionally administered) and dentist-supervised take-home bleaching.1,2 Nowadays, tooth bleaching is mainly done with different peroxide concentrations, such as hydrogen peroxide or carbamide peroxide which decomposes to also give hydrogen peroxide. The hydrogen peroxide then forms free radicals like hydroxyl and perhydroxyl radicals, and superoxide anions, unstable reactive oxygen molecules which are transformed to oxygen and hydrogen peroxide anions.3 Some bleaching products have a low pH (4.0) which would have an etching/damaging effect on the teeth. Low pH products should always be used with considerable caution. Clients today expect to observe tooth whitening directly after a visit to the dentist, an expectation which has led to the introduction of higher concentrations of chemicals and the use of different light sources believed to accelerate the bleaching process through the activation of a catalyst. Many light sources are now available: lasers, uv light, light-emitting diodes (LED's), halogen lamps and plasma arc lamps. Each of these instruments is supposed to light-activate a specific product which helps with the bleaching process. One disadvantage with most of these lights is that the tooth is heated, while the intra-pulpal temperature should not increase by about 5.5°C. There is still a vast controversy as to the effect of lights in improving the bleaching of teeth. Therefore, the purpose of this clinical study was to determine the whitening effect of a relatively new Light Emitting Diode System. This is one of the lights which are claimed to not increase the tooth temperature significantly.
METHODS AND MATERIALS
Students (ethical approval # 10/3/29) with two sound central maxillary incisors (teeth 11 and 21), in good dental and medical health and not on any medical treatment, were selected for this study. Smokers, subjects with fluorosis and tetracycline-stained or previously bleached teeth were excluded. In accord with the manufacturer's instructions,4 the teeth were polished with the Brite White polishing tool and paste4, rinsed and blot dried. The LED product (gel with 44% carbamide peroxide) was applied by the dentist on teeth 11 and 21 in the chair for 10 minutes. The process was repeated three times, followed by an at-home treatment period (30 minutes) of 14 days with 35% carbamide peroxide. The colour of the teeth (at the centre of the crown, 6mm diameter probe) was measured (with a spectrophotometer) just before treatment, after the LED gel application stage and after the 14 day at-home treatment period.
RESULTS AND DISCUSSION6
In this study the applications were effected in the manner outlined by the manufacturer. Many studies adapt and modify applications for some or other reason but the efficacy of the process needs to be evaluated with due consideration of the possible influence of the adaptations. Comparison of results with such studies is therefore not feasible.
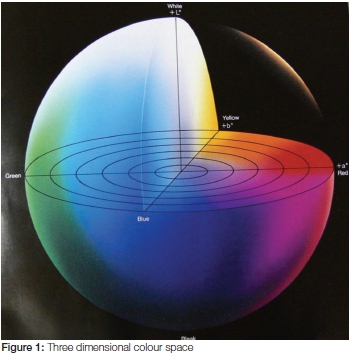
Measuring colour with a spectrophotometer is (for many reasons) by far the best method to use, for colours can then be quantified by numerical evaluation in a three dimensional colour space (L*a*b*).5 The total colour change (see Figure 1) is expressed as ΔE*ab which includes three components, ΔL*, Δa* and Δb* (The Δ shows a value which is the difference between before and after treatment). Hence, L* varies from a more black side (negative side) to a more white side (positive side), a* varies from a negative side (more greenish) to the positive side (more reddish), while b* varies from the more blue side (negative side) to the more yellow side (positive side).
The present LED system has the following specifications4 (according to the information provided by the manufacturer): a blue LED light (wavelength between 450 and 500 nm) which is claimed to activate their custom made gel which prevents heat formation, is FDA cleared and very successful in tooth colouring (up to 11 shade tabs). It is also claimed to boost the healing of mouth ulcers, cold sores and periodontal diseases.
The results for Teeth 11 and 21 did not differ significantly and therefore the data were pooled for the analysis. The L* value improved (more white) after the in-chair treatment with the LED system (LED light and gel with 44% carbamide peroxide with a specific catalyst) with no further significant increase after the 14 day treatment. However, the b* value improved (less yellow) after both the LED treatment and 14 day at-home treatment. The a* value did not improve significantly throughout the treatments. The total tooth whitening value (ΔE*ab = 1.8) was much lower than the 3.7 which was found for the Opalescence PF 10% (see part 17). The reason could be a combination of factors: in the case of the LED system the original in-chair treatment was 3x10 minutes with the LED light and the gel which also contained 44% carbamide (about 15% hydrogen peroxide). The light (LED) effective catalyst in the gel is probably partially responsible for the quick whitening process. Thereafter the at-home treatment was 30 minutes a day for 14 days with 35% carbamide peroxide (about 12% hydrogen peroxide), while in the case of Opalescence the treatment period was much longer (nightly, 6-8 hours) for 14 days with 10% carbamide peroxide. The longer nightly treatment is probably responsible for the superior whitening effect. Therefore, it seems that a longer daily treatment (overnight; Opalescence) with a low peroxide concentration (10% carbamide peroxide, about 3% hydrogen peroxide) gives better results than a shorter treatment period (30 minutes) with a higher peroxide concentration (LED system). Figure 2 gives an indication of what the visible colour improvement would look like. The original colour measurement was rated as A2.


CONCLUSION
This LED system gives relatively low tooth whitening with the main effect ΔE*ab = 1.8 but that is directly after the 3x10 minute in-chair treatment and there was only an additional insignificant increase (ΔE*ab = 0.2) after the 14 day at-home treatment. The advantage of the LED system is the in-chair effect, although with only half the success of Opalescence (ΔE*ab about 3.7). Low gingival and tooth sensitivity scores were also recorded.
References
1. Hattab FN, Qudeimat MA, al-Rimawi HS. Dental discolouration: an overview. J Esthet Dent 1999;11:291-310. [ Links ]
2. Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-15. [ Links ]
3. Perchyonok VT, Grobler SR. Tooth-bleaching: mechanism, biological aspects and antioxidants. Int J Dent Oral Hlth 2015; 1: doi http://dx.doi.org/10.16966/2378-7090.116. [ Links ]
4. Light Emitting Diode System; BriteWhite®Inc, Jasper, Alabama, USA. [ Links ]
5. Minolta, Precise colour communication, Minolta, Co., Ltd., Osaka, Japan, 1994; 9242-4830-92 IHCAJ. [ Links ]
6. Basson R, Grobler SR, vW Kotze TJ, Osman Y. Guidelines for the selection of tooth whitening products amongst those available on the market. SADJ 2013;68:122-9. [ Links ]
7. Grobler SR, Osman Y. Insights into the clinical effectiveness of whitening products - Part 1: Dentist-supervised-at-home bleaching product. SADJ 2016;71:363. [ Links ]
 Correspondence:
Correspondence:
Sias R Grobler:
Oral and Dental Research Institute
Faculty of Dentistry
University of the Western Cape
Private Bag X1, Tygerberg 7505, Cape Town, South Africa
E-mail: srgrobler@uwc.ac.za














