Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.72 n.1 Johannesburg Feb. 2017
RESEARCH
How effective are resin-based sealants in preventing caries when placed under field conditions?
C PotgieterI; S NaidooII
IBChD (Stell/UWC), PDD (UWC), MSc (Dent). Department of Community Oral Health, University of the Western Cape
IIBDS(Lon), LDS.RCS (Eng), MDPH (Lon), DDPH.RCS (Eng), MChD (Comm Dent), PhD (US), PG Dipl Int Research Ethics (UCT). Senior Professor and Principal Specialist, Faculty of Dentistry, University of the Western Cape
ABSTRACT
Fissure sealants are considered to be amongst the most effective, least invasive, primary preventive measures against occlusal caries, but surprisingly are not that commonly used. This cross-sectional comparative study evaluated the retention rate and effectiveness in preventing caries of resin-based (RB) fissure sealants that were placed on the occlusal surfaces of the first permanent molar teeth under field conditions on Grade One learners in a rural low socio-economic area community. The control population was a matched sample of Grade Two children. Dental caries and sealant retention were determined by a calibrated examiner who was not involved in the placement of the sealants. On the 12 month follow-up, the caries incidence rate on fissure sealed first permanent molar teeth was 7.1%, while that of the control group was 9.1%, a non-significant result (p=0.39). Sealant retention was also lower than generally reported, only 7.8% being fully intact after 12 months. The placement of resin-based fissure sealants under sub-optimal conditions in the field was not found to be beneficial in reducing the incidence of dental caries. There may be a need for different types of sealant materials to be made available in the public sector for optimal effectiveness.
INTRODUCTION
Dental caries is the most common chronic infectious disease of childhood and poses a serious public health problem in both developing and industrialized countries.1 The affliction has been on the increase since the beginning of the 21st century, especially amongst children from lower socio-economic communities.2 In South Africa, many people are poor. The official unemployment rate is 26.7%,3 approximately one in every three households is living below the food poverty line4 and more than 80% of the population are dependent on the State for their oral health services.5 The number of children enrolled in no fee schools in South Africa has increased by more than 70% from approximately 5.2 million learners in 2007 to about 9.2 million learners in 2015.6 More than two thirds of 6-year-old children suffer from dental caries and more than 80% of these lesions are untreated.7 In low socio-economic and rural communities, it is often truly difficult for most children to go to the dental clinic for treatment. Time, finances, long distances to clinics and limited availability of transport are real-world challenges faced by many South African children on a daily basis. These difficulties have resulted in many children foregoing preventive and/or curative treatment.
Untreated dental caries results in pain and sepsis and only when the symptoms are severe do many children from lower socio-economic communities seek dental care. In most cases delay in care results in the caries lesion becoming too extensive to restore, resulting in dental extractions being often the most common treatment carried out in public oral health settings.8 Dental public health treatment data has revealed a significant increase over the past ten years in the number of tooth extraction procedures (often under general anaesthesia) and a decrease in the number of restorations and fissure sealants being done.8 Untreated dental caries negatively impacts the immediate and long-term quality of a patient's life. Consequently, a need was identified to urgently reverse these trends in the dental public health sector and to increase the provision of proven preventive oral health strategies such as fissure sealants. Prevention of dental caries and reducing the future costs of associated surgical, restorative and prosthetic procedures is therefore important from a public health point of view.8
Fissure sealants are recognized as one of the most effective and least invasive procedures to prevent and control dental caries and can ensure complete protection and total preservation of the occlusal surfaces of posterior teeth.9 However, despite strong evidence for the safety, effectiveness and cost-efficiency of fissure sealants, their use still remains low.10,11
The placement of fissure sealants is particularly low among school children from lower socio-economic communities in which parents are often unemployed, uneducated, live in low-cost housing and attended public schools.12,13 The social inequality in sealant utilisation is of particular interest as it seems to suggest that those children most in need are least likely to receive dental sealants.14
In an effort to address this inequality, school-based fissure sealant programmes (SBFSP) were introduced and have been shown to be an effective way of increasing delivery of this protective measure. The World Health Organization, Centres for Disease Control and Prevention (CDC) and the Association of State and Territorial Dental Directors (ASTDD) have subsequently endorsed the implementation of SBFSP.15 Programmes that focus on SBFSP are therefore justified due to the cost-saving attributes of fissure sealants, the lack of on-going access to care and the high probability that a cavity would not be restored promptly.
Oral health practitioners in the public sector should therefore make every effort to improve accessibility and to provide application of fissure sealants, especially among children from lower socio-economic communities who are particularly vulnerable to dental caries. In 2013, 356 resin-based fissure sealants were placed on the first permanent molar teeth of 100 Grade One children by a dentist working at the local public dental clinic as part of a routine school-based fissure sealant programme, but not as a controlled study. Recognising that transportation of the children to the dental clinic was problematic, the dentist decided instead to go to the primary school and do the fissure sealants there. This was done in an effort to ensure that these children from a low socio-economic area could benefit from the caries preventive properties of fissure sealants. However, the only sealant available to the dentist was resin-based.
The SBFSP programme
The commonly adopted 'high risk' approach for the prevention of dental caries in a population was not followed in this programme. A 2006 study showed that 'high-risk' children accounted for less than 6% of new carious lesions with the remaining 94% of new lesions coming from those children who were classified as being at lowest baseline caries risk.16 The identification and sealing of "high-risk" children was found in that study to be ineffective in reducing the overall incidence of dental caries in a population.16,17
In the 2013 programme the fissure sealants were therefore placed on the permanent molars of all eligible Grade 1 learners (100) who delivered a signed consent form, irrespective of the child's individual caries risk or oral health status. Inclusion criteria provided that a child was in Grade 1 and that the first permanent molar teeth were fully erupted and caries-free (zero baseline level of caries). In some children, not all four molar teeth met these conditions. In such cases, fissure sealants were placed only on the eligible teeth, resulting statistically in an average of 3.56 first permanent molar teeth sealed per child.
No mobile dental truck, portable suction or dental assistant were available. The sealants were placed in the staff room of the local primary school, the dentist working under natural light and making use of the two-handed placement technique. The children were seated on the fold-up dental chair, with no compressed air or suction available. There was no water rinsing or air drying of the occlusal surfaces. The occlusal surfaces of the targeted teeth were cleaned with wet cotton wool pellets and dried with dry cotton wool pellets. Isolation was achieved by placing cotton rolls lingually and buccally of the targeted teeth. The cleaned occlusal surfaces were conditioned by using the self-etch Adper-L-Pop system by 3M ESPE. The self-etching liquid was applied with the brushes that are standard provision with the system and was cured with a cordless curing light for 30 seconds.
The resin-based Clinpro® fissure sealant (3M ESPE) was applied onto the conditioned occlusal pits and fissures, manipulated with the brush tip to free potential air bubbles and cured for 30 seconds. No rotary instruments were available and therefore no occlusal adjustments were made at the time of placement.
Dental caries was clinically detected by visual inspection according to the WHO guidelines18 and only on children with signed consent forms. Children brushed their teeth before being examined while seated on a mobile dental chair in the classroom. The examiner used a surgical headlight for additional illumination. A mouth mirror, ball-ended dental probe, and a mobile 3-in-1 air syringe for proper drying of the tooth surfaces were used to assist with the intra-oral examination. Prior to the clinical dental evaluations, standardisation and calibration of the examiner was carried out on a group of pre-selected children.
The 2013 exercise was not part of any school Caries Preventive Programme or study, no initial caries screening had been done in a control group and no scientific sampling process was followed.
This study took advantage of the data from that programme and was therefore concerned with investigating the caries preventive effect of a resin-based fissure sealant when placed under field conditions on recently erupted first permanent molar teeth. Hence carious lesions detected at the 12 month follow-up were regarded as "incidence" cases.
Ethical Considerations
The study protocol was granted ethical approval by the Senate Research Ethics Committee of the University of the Western Cape. Informed consent was obtained from the principals of each participating school and from the parents or guardians of the children who were to participate in the study. It was emphasized that strict confidentiality would be maintained at all times and that the parents or guardians could withdraw their child from the study at any time without being penalised in any way. Irrespective of whether they were part of the present study or not, all Grade 2 learners of the participating primary schools received instructions on good oral health behaviour as well as a toothbrush and toothpaste. Children with any treatment needs were referred to the nearest clinic to have the necessary treatment and for the placement of fissure sealants if appropriate.
METHODS
Control Group
The school chosen as the source of the control group was in close proximity to the school attended by the children on whom the sealants had been placed, and was in the same socio-economic area. On 12 month follow-up the study group had had a drop-out rate of 20%, which resulted in a sample size of 80 children. A systematic cluster sampling process was then undertaken to identify the control group. Matching was done until the control group comprised the same number of children (80).
Data capture and analysis
A structured Microsoft Excel spread sheet data capture sheet suited to the aim and objectives of the study was designed to ensure that it was clear, simple and unambiguous, minimized potential errors by the researcher and coder and enabled efficient and meaningful analysis of the data.
Basic descriptive analyses were done using the Microsoft Excel environment, while further statistical analyses used the statistical computing programme "R".19 Several statistical tests were carried out to determine whether any significant differences (p=0.05) existed between different elements of the captured data. The Relative Risk (RR) was computed using the Cochrane Software (version 5.2) program for absence and/or caries presence at the end of the observation period of 12 months.
RESULTS
Examiner calibration. The intra-examiner agreement kappa statistic was 0.9083.
At the time of sealant placement in 2013, exactly 100 Grade 1 learners were eligible and received fissure sealants in accordance with the placement criteria. This amounted to 356 first permanent molar teeth that were sealed (an average of 3,56 teeth per child). On 12 month follow-up, the remaining 80 children presented 281 previously sealed teeth to be examined for fissure sealant retention and caries experience (an average of 3,51 teeth per child).
Main results:
Caries incidence rate at 12 month follow-up of sealed versus unsealed teeth:
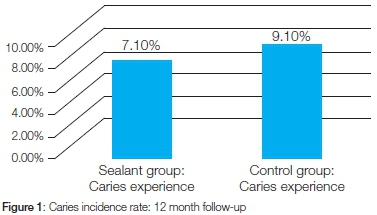
The caries incidence rate at 12 month follow-up among the RB sealed teeth was 7.1% compared with 9.1% among the unsealed teeth (Figure 1).
RB sealant retention at 12 month follow-up:
Only 22 (7.8%) of the 281 RB treated teeth that were available for assessment had fully intact sealants left. A total of 256 sealants (91%) had already been lost and three of the 281 previously sealed teeth had been extracted during the 12 month period.
Analysis of subgroups:
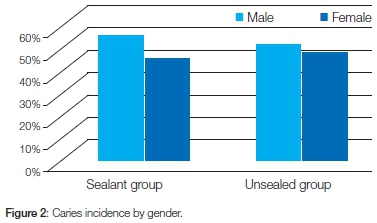
There was no statistically significant association between the caries incidence rate in male versus female subjects (p=0.6864) (Figure 2). In the sealed group, 55% (11 out of 20) of the carious teeth were found in males and 45% (9 out of 20) in females. The unsealed group showed a similar pattern 52% (15 out of the 29) carious teeth found in males and 48% (14 out of the 29) in females.
Caries prevalence by tooth number is shown in Table 1 and while the mandibular molars had more carious lesions than the maxillary molars, this was not statistically significant (p=0.159).

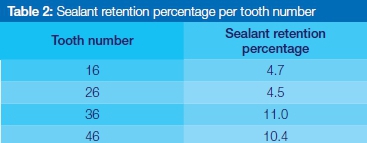
The 12 month follow-up screening revealed that more partially or fully retained sealants were found on the mandibular molar teeth (Table 2). This was shown to reflect a significant difference between sealant retention on upper and lower molar teeth (p=0.044).
DISCUSSION
From a public health point of view, one always needs to be cognisant of the impact that the adopted strategy will have on the total dental health and disease burden of the targeted population as a whole.16 Therefore, when a SBFSP is conducted, clinicians should also consider caries risk at the level of the school and community, instead of only assessing caries risk at the level of the patient or tooth.17 It was subsequently concluded that from a public health perspective, policies for caries preventive strategies should be based on a 'population' or 'directed population' approach, instead of a 'high-risk' approach.16
The caries incidence rate of the unsealed group in the study was 9.1% as opposed to 7.1% in the sealed group. This resulted in a 2% caries preventive effect of the resin-based fissure sealants. These had been placed under field conditions, showed a high loss (91%) over the period of the study and their effect in preventing caries was not statistically significant.
The patient response rate was 80%, a figure acceptable in epidemiological studies.20 The recommendation for placing fissure sealants on molars is that the procedure be completed preferably within the first year after complete eruption and not more than 4 years later than this.8 First permanent molar teeth usually erupt when a child is aged between 6 and 7 years.21 Fissure sealants should therefore be placed on children aged 6 to 8 years, depending on the eruption status of the targeted teeth. In the current study, the average age of children at time of sealant placement was 7 years and 4 months, which falls within the suggested guidelines. Although it is generally accepted that fissure sealants can safely be placed on teeth with early, non-cavitated carious lesions,17,22 all the sealants in this study were placed on caries-free teeth.
Favourable marginal adaptability of the sealants is a primary factor which can influence its caries inhibiting effect. The sealant must form a proper seal to minimize microleakage and marginal gap formation.23 When inadequate fissure sealants are not replaced, secondary caries may ensue.24,25 In turn, microleakage is significantly influenced by the condition of the enamel (sound or carious) and by the location of the caries in the fissures. The problem is generally found to be higher where the borders of the sealants are on carious enamel, where the sealant occlusal length is longer and where the entrance angle between the enamel surface and sealant is larger (shallow fissures).
Microleakage can also occur after fracturing of the sealant (i.e. not fully intact sealant, which can result due to stress or thermodynamic shrinkage of the sealant) and can lead to discoloration, secondary caries, tooth hypersensitivity and pulpitis.24 Paradoxically, when sealants are not placed properly, dental caries may actually increase, instead of the desired reduction.26 Microleakage was also found to be greater in glass ionomer (GI) than in RB sealants.27 However, recent studies have shown that the incorporation of bioactive glass (BAG) into GI compositions has resulted in an improvement of the bioactivity, tooth regenerative and reconstruction capacity of the GI composition.28 GI fissure sealants containing 45S5 bioactive glass, despite some marginal leakage, have been shown to be effective preventive dental materials for inhibiting secondary caries at the tooth/sealant marginal gap area.29
The 7.1% caries incidence rate in the study is almost three times higher than the average of 2.5% as reported in the systematic review by Condò et al.9 However, in that study, all the sealants considered had been placed under ideal conditions. This is relevant for there are fundamental differences between the placement of fissure sealants in a clinical (ideal) versus a non-clinical (in the field/at a school) setting. The two situations are mainly distinguished by assumptions about the availability of diagnostic and treatment options and utilisation of dental care patients.30 In a clinical setting there is a higher likelihood that practitioners can provide a continuous health care service with a comprehensive range of caries diagnostic and treatment options available (i.e. follow-up of fissure sealants with replacement where necessary). This is in contrast to children who are treated 'in the field' (i.e. at a primary school as in this study). These children are more likely to be episodic users of primary oral health services, with a reduced chance of receiving follow-up care (i.e. monitoring and replacement of fissure sealants).30
Traditionally, resin-based fissure sealants have been the most commonly used dental sealant material and have been hailed by some as the "gold-standard" in dental sealant materials.31 It has been shown to be successful when placed under ideal conditions (i.e. clinical settings using a four-handed technique) and where follow-up visits can be done. Successful application of a RB sealant involves strict attention to detail and dry field isolation throughout the procedure.32 Hence, the procedure is very technique sensitive and is especially affected by saliva contamination, the most commonly reported reason for RB sealant failure.33 Resin-based dental sealants can only exert a protective effect on an intact tooth surface.34,35 The four-handed placement technique has therefore been advocated as the best way to ensure clinical success with RB sealants. This technique allows one operator to take control of the field of isolation (preferably with cotton rolls supplemented by portable water and a suction system) while the other performs the steps of the sealant placement protocol.36 The four-handed placement technique was furthermore associated with a nine percentage point increase in sealant retention over the two-handed placement technique (placement of sealants by a single operator).37 In cases where saliva contamination is least likely to occur, such as in a clinical setting with the use of the four-handed placement technique, the choice of either a RB or GI sealant is warranted.38,39
There is evidence that GI sealants should be considered when fissure sealants are to be placed under field conditions where saliva control may be a challenge and no follow-up is planned.40 This may be due to the hydrophylic properties of GI sealants which mean that they do not require an absolutely dry field of placement to be successful. Glass ionomer sealants also contain fluoride ions which are released and taken up by the tooth enamel. This assists in remineralisation of the enamel and thus renders the tooth structure less susceptible to demineralization.40 Furthermore, Pardi et al (2003)41 have noted that even after glass ionomer sealants appear to have been lost from the tooth surface, some small amounts can still be found in the pits and fissures and release fluoride which helps in remineralising the tooth enamel. This characteristic of GI sealants seems to suggest that a follow-up and replacement of a GI sealant programme is not as important as is the case with a RB sealant programme. Current clinical evidence furthermore suggests that high viscosity GI sealants are not inferior to RB sealants in terms of caries preventive properties.31 On the contrary, it seems that similar caries-preventive efficacies exist after a period of 48 months and the study even mentions a possibly superior caries preventive effectiveness of high viscosity GI sealants over RB sealants after 60 months.31 Therefore, when saliva contamination is likely to be a high risk factor, such as in the context and setting of the present study, a GI sealant material would ideally have been the preferred material of choice.31,40
CONCLUSION
The present study has shown that under field conditions, and among children, RB sealants are not ideal for caries protection. When one takes into account the context (a young child), the setting (under field conditions), follow-up (or lack thereof) and isolation challenges (saliva contamination) that are associated with a school based fissure sealant programme, materials alternate to resin-based fissure sealants should be considered.
Such appropriate choices should be made available, especially to oral health professionals in public dental clinics, to ensure enhanced effectiveness of the intervention strategy and to reduce the disparities that currently exist in oral health status and access to oral health preventive services.42
RECOMMENDATIONS
Interest and attention are increasingly being paid to the application of "smart" bioactive materials in the field of dentistry. The inclusion of a bioactive glass in a GI fissure sealant material is recommended for its potential to assist in the reduction of caries at the marginal gap area, thereby helping to prevent the formation of primary and secondary occlusal caries.29
LIMITATIONS
The fact that these sealants were not initially placed as part of any controlled study has resulted in potential sources of bias and limitations. Appropriate sample sizes of the case and control groups could not be statistically determined. No initial caries screening was undertaken for the control group. The researcher also could not conduct a re-examination of the targeted groups due to serious time constraints. Another limitation to all fissure sealant studies is the fact that the sealants themselves may be contributing factors in the development of secondary caries.
ACRONYMS
ASTDD: Association of State and Territorial Dental Directors
CDC: Centres for Disease Control and Prevention
RB: Resin-based
SBFSP: School-based Fissure Sealant Programmes
References
1. SADA Head Office. Communique. SADJ 2016; 71(2): 52-3. [ Links ]
2. Bagramian RA, Garcia-Godoy F, Volpe AR. The global increase in dental caries. A pending public health crisis. American Journal of Dentistry 2009; 22(1): 3-8. [ Links ]
3. Statistics South Africa. Key statistics: Unemployment [Online]. Available from < http://www.statssa.gov.za/ >. [Accessed on 19 June 2016]. [ Links ]
4. Statistics South Africa. Income dynamics and poverty status of households in South Africa. [Online]. Available from < http://www.statssa.gov.za/publications/Report-03-10-10/Report-03-10-102014.pdf >. [Accessed on 4 March 2016]. [ Links ]
5. Van Wyk PJ, Van Wyk C. Oral health in South Africa. International Dental Journal 2004; 54: 373-7. [ Links ]
6. Department of Basic Education. National Assembly Written Reply Question 3825. 2016 [Online]. Available from: < http://www.education.gov.za/Newsroom/ParliamentaryQuestions/2015ParliamentaryQue stions/tabid/954/ctl/Details/mid/3960/ItemID/3502/Default.aspx > [Accessed on 22 July 2016] . [ Links ]
7. Van Wyk C, Van Wyk PJ. Trends in dental caries prevalence, severity and unmet treatment need levels in South Africa between 1983 and 2002. South African Dental Journal 2010; 65(7): 310-4. [ Links ]
8. Lalloo R, Turton MS. Fissure sealants on permanent first molars - consequences of a one-year delay. Community Dental Health 2008; 25: 191-2. [ Links ]
9. Condò R, Cioffi A, Riccio A, Totino M, Condò SG, Cerroni L. Sealants in Dentistry: a systematic review of the literature. Oral & Implantology 2013; Anno VI, 3: 67-74. [ Links ]
10. Zadik Y, Bechor R. Hidden occlusal caries: challenge for the dentist. N Y State Dent J 2008; 74(4): 46-50. [ Links ]
11. Centres for Disease Control and Prevention. Surveillance for Dental Caries, Dental Sealants, Tooth Retention, Edentulism, and Enamel Fluorosis: United States, 1988-1994 and 1999-2002. Surveillance Summaries 2005; MMWR (54). [ Links ]
12. Al Agili DE, Niazy HA, Pass MA. Prevalence and socio-economic determinants of dental sealant use among schoolchildren in Saudi Arabia. Eastern Mediterranean Health Journal 2012; 18(12): 1209-16. [ Links ]
13. Ayo-Yusuf OA, Okagbare TE, Ayo-Yusuf IJ. Prevalence and socio-economic disparities in fissure sealant placement among adolescents in the Limpopo Province, South Africa. Journal of the South African Dental Association 2011; 66 (8): 380-3. [ Links ]
14. Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. National Centre for Health Statistics. Vital Health Stat 2007; 11: 1-92. [ Links ]
15. U.S. Department of Health and Human Services. Oral Health in America: Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health. 2000. [ Links ]
16. Batchelor PA, Sheiham A. The distribution of burden of dental caries in schoolchildren: a critique of the high-risk caries prevention strategy for populations. BMC Oral Health 2006; 6:1-5. [ Links ]
17. Gooch BF, Griffen SO, Gray SK, Kohn WG, Rozier G, Siegal M, Fontana M, Brunson D, Carter N, Curtis DK, Donly KJ, Haering H, Hill LF, Hinson HP, Kumar J, Lampiris L, Mallat M, Meyer DM, Miller WR, Sanzi-Schaedel SM, Simonsen R, Truman BI, Zero DT. Preventing dental caries through school-based sealant programs. Updated recommendations and reviews of evidence. JADA 2009; 140: 1356-65. [ Links ]
18. Petersen PE, Baez RJ. Oral Health Surveys: Basic Methods, 5th ed. Geneva: World Health Organization, 2013. [ Links ]
19. R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, 2013. URL http://www.R-project.org/. [ Links ]
20. Joubert G, Ehrlich R. Epidemiology: A Research Manual for South Africa. 2nd Edition. Cape Town: ABC Press, 2007. [ Links ]
21. American Dental Association (ADA). Tooth eruption: The permanent teeth. JADA, 2006; 137: 127. [ Links ]
22. Beauchamp J, Caufield PW, Crall JJ, Donly K, Feigal R, Gooch B, Ismael A, Kohn W, Siegal M, Simonsen R. Evidence-based clinical recommendations for the use of pit-and-fissure sealants: A report of the American Dental Association Council on Scientific Affairs. Dental Clinics of North America 2008; 53(1): 131-47. [ Links ]
23. Shapiro J, Eidelman E. The influence of mechanical preparation of enamel prior to etching on the retention of sealants - a three year follow-up. J Pedod 1984; 8: 272-7. [ Links ]
24. Yang SY, Kwon JS, Kim KM. Inhibition of enamel demineralization by pit and fissure sealant containing 45S5 bioactive-glass. Dental Materials 2013; 29 Suppl 1:e63. [ Links ]
25. Celiberti P, Lussi A. Penetration ability and microleakage of a fissure sealant applied on artificial and natural enamel fissure caries. Journal of Dentistry 2007; 35(1): 59-67. [ Links ]
26. Lee SH. Pit and fissure sealing-advanced technique. Korean Dent Assoc 2011; 49:22-32. [ Links ]
27. Ganesh M. Comparative evaluation of the marginal sealing ability of Fuji VII and Concise as pit and fissure sealants. The Journal of Contemporary Dental Practice 2007; 8(4): 1-8. [ Links ]
28. Khoroushi M, Keshani F. A review of glass-ionomers: From conventional glass-ionomer to bioactive glass-ionomer. Dent Res J (Isfahan) 2013 Jul-Aug; 10(4): 411-20. [ Links ]
29. Yang K, Kwon S, Kim KN. Enamel surface with pit and fissure sealant containing 45s5 bioactive glass. Journal of Dental Research 2016; 1-8. [ Links ]
30. Kumar J, Siegal M. Workshop on guidelines for sealant use: recommendations. The Association of State and Territorial Dental Directors, the New York State Health Department, the Ohio Department of Health and the School of Public Health, University at Albany, State University of New York. J Public Health Dent 1995; 55(5 spec no): 263-73. [ Links ]
31. Mickenautsch S, Yengopal V. Caries-preventive effect of high-viscosity glass ionomer and resin-based fissure sealants on permanent teeth: a systematic review of clinical trials. 2016. [Online]. Available from < http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4723148/ >. [Accessed on 06 April 2016]. [ Links ]
32. Simonsen RJ. Pit and fissure sealant: review of the literature. Pediatr Dent 2002; 24 (5): 393-414. [ Links ]
33. Azarpazhooh A, Main PA. Pit and fissure sealants in the prevention of dental caries in children and adolescents: a systematic review 2008. [online]. Available from: <http://www.cda-adc.ca/jcda/vol-74/issue-2/171.html> [accessed: 02 April 2014]. [ Links ]
34. Kühnish J, Mansmann U, Heinrich-Weltzien R, Hickel R. Longevity of materials for pit and fissure sealing - results from a meta-analysis. Dental Materials 2012; 28: 298-303. [ Links ]
35. Rock WP, Anderson RJ. A review of published fissure sealants trials using multiple regression analysis. J Dent 1982; 10: 39-43. [ Links ]
36. Aleksejūnienė J, Brondani MA, Pattanaporn K, Brukiene V. Best practices for dental sealants in community service-learning. Journal of Dental Education 2010; 74(9): 951-60. [ Links ]
37. Griffin SO, Jones K, Gray SK, Malvitz DM, Gooch BF. Exploring four-handed delivery and retention of resin-based sealants. JADA 2008; 139(3): 281-9. [ Links ]
38. Yengopal V, Mickenautsch S, Bezerra AC, Leal SC. Caries-preventive effect of glass ionomer and resin-based fissure sealants on permanent teeth - a meta-analysis. J Oral Sci 2009; 51: 373-82. [ Links ]
39. Emmerling Munoz H, Carver Silva J. Pit and fissure sealants: an overview. Rdh 2013; 33(10): 95-100. [ Links ]
40. Lindemeyer RG. The use of glass ionomer sealants on newly erupting permanent molars. Journal of the Canadian Dental Association 2007; 73(2): 131-4. [ Links ]
41. Pardi V, Pereira AC, Mialhe FL, Meneghim MC, Ambrosano GMB. A 5-year evaluation of two glass-ionomer cements used as fissure sealants. Community Dent Oral Epidemiol 2003; 31: 386-91. [ Links ]
42. Tomar SL, Reeves AF. Changes in the oral health of us children and adolescents and dental public health infrastructure since the release of the Healthy People 2010 Objectives. Academic Paediatrics 2009; 9: 388-95. [ Links ]
 Correspondence:
Correspondence:
Carl Potgieter
Department of Community Oral Health, University of the Western Cape
Tygerberg
E-mail: odndentist@gmail.com














