Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.72 n.1 Johannesburg Feb. 2017
RESEARCH
Types of dental emergency services provided to dentally fit soldiers in Area Military Health Unit Gauteng, South Africa
TK MadibaI; A BhayatII
IB Dent Ther, BDS, DHSM, MChD (Community Dentistry). Senior Lecturer and Head of Clinical Unit, Department of Community Dentistry, School of Dentistry, Faculty of Health Sciences, University of Pretoria, South Africa
IIBDS, MSc, MPH, M Dent (Community Dentistry). Department of Community Dentistry, School of Oral Health Sciences, University of Pretoria
ABSTRACT
BACKGROUND: The prevention and treatment of dental diseases are important in maintaining a combat-ready military force.
AIM: To determine the type of dental emergency treatments provided over 12 months to soldiers who had been classified as dentally fit.
METHODS: A retrospective analysis was carried out of the dental records of members of the South African National Defence Force in Gauteng who had been screened and certified to be dentally fit in 2009. The records of the participants were followed up for a year thereafter to determine the profile of dental emergency treatments rendered. Data analysis included frequencies and correlations using chi-square tests. The level of significance was set at p<0.05.
RESULTS: Of the 6352 soldiers deemed to be dentally fit, 1947 (30.7%) returned for treatment within 12 months. Most required dental restorations (59%) followed by extractions (13%) and crown/bridge repairs (12%). In general, males, soldiers between 41 and 50 years, non-commissioned officers, Whites and Oral Health Fitness II (OHF) received more dental emergency services compared with their counterparts.
CONCLUSIONS: A large number of soldiers previously determined as dentally fit required restorations and extractions within a year. The treatment procedure profile was influenced by OHF classification, race, age and military rank.
Keywords: Dental procedures, Dental Fitness Classification, Military.
INTRODUCTION
Dental emergencies within the military environment are a potential threat to any military mission as the result could be the removal of soldiers from their assigned places of duty. The prevention and treatment of dental diseases are therefore essential in maintaining a combat-ready military force as dental emergencies have a direct effect on a person's health and could reduce combat effectiveness and the capability of a deployed force to accomplish its assigned mission,1 a major concern for military planners.2 A study of a deployed armoured division reported that dental complaints ranked second only to upper respiratory tract infections as a cause of lost duty time.3 This meant that the prevalence of dental conditions was extremely high and debilitating for the soldiers. Dental complications may therefore have dire consequences as the poor dental health of one individual can compromise the effectiveness of the entire unit.4
Dental readiness is an integral component of the overall medical readiness program of the South African National Defence Forces (SANDF), which defines full readiness as being healthy in all categories, including oral health. The SANDF uses the Oral Health Fitness (OHF) classification to categorise the dental readiness status of all military personnel, a system similar to that used by members of the North Atlantic Treaty Organization (NATO), which is defined in the Standard Agreement (STANAG) 2466.5 This classification consists of four OHF categories:
• Class I: fully dentally fit and requires no dental treatment;
• Class II: minor dental treatment is required but the condition/s are not expected to cause a problem within the next year;
• Class III: treatment is required and the condition/s is/are expected to cause a problem within the next year
• Class IV: dental examination has expired after 12 months or the member has never been classified.
Personnel who are classified as OHF class I and II meet the criteria for dental readiness and are therefore considered deployable and ready for any operational assignment.5,6 This status is valid for a single year and soldiers must be screened annually to ensure that their medical status is updated. The aim of the dental readiness program is to ensure that all personnel are either in Class I or II and those who do not fall into these categories need to be treated to achieve Class I or II status. According to the OHF classification system, the SANDF strives to achieve oral health fitness by focusing treatment towards those conditions, which, if left untreated, could result in a dental emergency within 12 months. A dental emergency is defined as any condition that has the potential to cause pain, uncontrolled haemorrhage, acute infection or loss of masticatory function, which may significantly impact on the patient's performance of duties.5
It is essential to determine the types of emergency treatment required by OHF I and II soldiers as it helps in the planning and managing of soldiers required for deployment. It also gives a breakdown of the type of services most commonly required and this will assist in the employment of suitably qualified personnel and the calculation of resources that may be required. This study focused on the type of dental emergency treatment rendered to members in OHF classes I and II as they were regarded as dentally fit and deployable. No similar study has produced baseline data for the planning and monitoring of dental services for soldiers.
The aim of the study was therefore to determine the type of dental emergency treatment provided over a one year period to soldiers who had previously been classified as dentally fit using the OHF classification criteria.
METHODS
This was a cross-sectional retrospective record-based study, which included all the records of members of the SANDF who had received an OHF classification of I and II in Area Military Health Unit, Gauteng, during 2009. The records of the 12 months following the initial screenings were examined to identify whether the soldiers had received any dental emergency treatment during this time. Those procedures were recorded using a standardized data capturing tool and included the number of extractions, restorations, endodontic treatments, crown and bridge related problems, denture problems, tooth sensitivity and medication. The "restorations" category included amalgam, composite and temporary restorations. The "extractions" included the removal of teeth, root rests, impacted teeth and surgical extractions. The "crown and bridge" related problems included re-cementing of an existing prosthesis and delivering of a new prosthesis. Since there were very few soldiers who presented with denture problems, sensitivity of teeth or required medication for dental problems, these services were combined to form a miscellaneous group which was classified as "other services".
In addition to the type of services being rendered, demographic information such as gender, race (self identified), OHF and military rank was also recorded. As far as rank was concerned, the soldiers were divided into the following three groups: Generals and senior officers, Junior and Warrant officers and Non- Commissioned officers (includes Privates, Lance Corporals, Corporals, Sergeants and Staff Sergeants).
A total of 6352 soldiers had received an OHF classification of I or II in Gauteng during 2009 and all of their records were captured and analyzed. All data was confidential and anonymity was ensured by not including any names. Ethical clearance was obtained from the University of Pretoria Ethical committee (Ref 98/2011). Data analysis was carried out with the use of SPSS version 23. Group differences were assessed using chi-square statistics and odds ratios. Data analysis included frequencies of dental emergency procedures and chi-square tests. The level of significance was set at p<0.05.
RESULTS
The sample of 6352 soldiers had a mean age of 40 years, and 46,4% had received an OHF classification of I, whilst 53,6% were categorized as OH II. The majority of participants were Blacks (72%) followed by Whites (21%) with Coloureds and Asians at 6% and 1% respectively. As far as gender was concerned the majority were males at 70%. Almost a third of the sample, (31% n = 1947) developed a dental emergency within the twelve month period of the study and had to receive treatment. The dental emergency rate was therefore 1947 of 6352 which was translated to 307/1000 per annum.
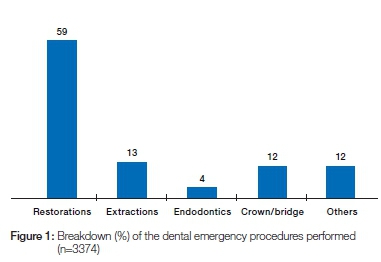
A total of 3374 dental emergency procedures were performed on the 1947 soldiers with an average of 1.7 emergency procedures per individual. Most common were restorations (59%), extractions (13%), crown and bridge related treatments (12%) and endodontic treatment (4%) (Figure 1).
The association between dental emergency procedures and gender, age, race, rank and OHF classification are shown in Table 1. The number of dental emergency procedures associated with each variable was expressed as a percentage of the total procedures delivered. In general, males, soldiers between 41 and 50 years, non-commissioned officers, Whites and OHF II received more dental emergency services compared with their counterparts. Soldiers between 40 and 51 years old, Blacks, non-commissioned officers and those classified as OHF II received significantly more extractions compared with the other groups.
In terms of restorations, soldiers between 41and 50 years old and non-commissioned officers received significantly more services compared with the rest of the sample.
With respect to endodontics and crown and bridge work, the generals and senior officers, soldiers and Whites were the majority recipients of these services.
DISCUSSION
Of the total of 6352 soldiers who had received an OHF classification of I or II, 70% were male. This was consistent with other international studies which reported more males being recruited into the military services than females.7,8
The demographics of South Africa, with a population having 80% Blacks, were reflected in the sample of the soldiers who had been screened, which included 72% Black candidates.9 The mean age of the soldiers was 40 years, possibly showing that the military has a distribution of both young and older soldiers. The older, more senior soldiers were more often in management positions, while the younger soldiers were more likely to be involved in deployment exercises.
It was unexpected to find that almost a third (31%) of those soldiers who had been classified as OHF I and II, who should have been dentally fit and ready to be deployed, experienced a dental emergency within 12 months. According to the literature, the dental emergency rate of 307/1000 per year (31%) is regarded as high as this implies that for every ten soldiers certified dentally fit, three will nevertheless experience a dental emergency.10 This could be due to many factors including the possibilities that the screening tool was not sensitive enough to detect impending dental emergencies or that the staff members were not adequately trained and calibrated to carry out the screening effectively. It could also imply that many soldiers are exposed to traumatic conditions which could result in oral trauma such as teeth being broken, prostheses being knocked out or restorations fractured.
These data expose a problem of some relevance. A possible solution could be to select one or two dentists from each facility, tasking them exclusively with the screening procedure. These staff members should be trained and made aware of the guidelines related to the OHF classification system. They also need to be calibrated in order that a uniform classification system may be applied across the country. This would reduce possible variations with the screening and assist in the detection and diagnosis of dental conditions which have the potential to become emergencies within a one year period. Another possible solution is to reduce the duration of validity of the classification from one year to six months. The year-long period between screenings may be too long and as a result many potential emergency dental conditions were missed. However, this has severe implications as it would consume a large amount of time and resources which would probably make the sequence unsustainable.
Another concern is the fact that those who did present with dental emergencies required, statistically, almost two treatments (1.7) per year. This further emphasizes the need for calibration among the dentists who are performing the screening as it appears they are not consistently successful in diagnosing those who are at high risk of developing dental emergencies.
If the current situation persists, it could have dire consequences as it implies that three out of every ten soldiers who were classified as dentally fit actually developed a dental emergency. This would impact on deployment and conceivably on the ultimate success or failure of South African military missions.
Dental restorations were the most commonly required service (59%), followed by extractions (13%) and crown and bridge related treatment (12%). The trend in the type of services that were carried out, mostly restorations and extractions, compared favorably with other international studies.2,9 However, the quantity of services carried out in the current study was much higher in relation to other similar studies.11,2
Many of the soldiers who had been deemed dentally fit, returned within 12 months of their screening having a decayed or broken tooth that required a restoration. This could imply that soldiers had presented with initial or secondary caries at the time of screening but the attending dentist either did not diagnose the condition appropriately or underestimated the potential for it becoming an emergency within 12 months.
Just over 10% of the soldiers required extractions, possibly because severe carious lesions and/or poor endodontic and/or periodontic conditions had not been identified as potentially emergency conditions.
The difference between the types of dental emergency procedures performed between the two OHF categories was significant. In general, the soldiers who were classified as OHF II required more dental emergency procedures than those classified as OHF I. The OHF II classification is defined as "dental treatment is required but the condition is not expected to cause a problem within the next year", but nevertheless, the group was more susceptible to experiencing an emergency. These results were confirmed by other studies.2,10-12
Soldiers who were classified as Whites required mostly restorative services while Blacks required mostly extractions. In South Africa, before 1994, dental services and health care were rationed according to racial lines with Blacks being offered fewer services compared with Whites.13 The situation with regard to distribution of health services is improving but there are still arears with no immediate access to health services. The fact that more extractions were required by Black military personnel is perplexing considering that everybody in the military has access to the services. There may be several possible reasons why this is so, but certainly there is a need for continuous oral hygiene instruction and enhanced dental awareness amongst all the soldiers.
Non-Commissioned officers required more services than other ranks. These were the young soldiers who perhaps had the highest burden of dental decay and periodontal treatment compared with more senior soldiers who had been in the military for a longer period and may previously have received initial treatment. This result is consistent with a similar study which reported that enlisted submariners (equivalent to non-commissioned offices) were around two times more likely than senior officers to have a dental emergency.12 The concern with non-commissioned officers requiring more dental emergency procedures are that these are the soldiers who are tasked to carry out the majority of the work and are most likely to be deployed. These officers carry weapons and are more in the front lines as compared with other ranks. Their enforced removal with dental problems from deployment could result in mission failure.
Generals and senior officers as a group received more crown and bridge related treatments (45%) than the other ranks. This was expected as most of them are older soldiers and as a result may have more prostheses compared with their younger counterparts.
The prevalence of dental emergency procedures increased with age, with the 20-30 year olds requiring the least amount of dental services. This finding is consistent with other studies which indicate that caries is an age dependent phenomenon that increases with age and hence as soldiers got older, their dental requirements, as a result of dental caries, increased as well.14-16
LIMITATIONS
The prevalence of smoking and history of any smoking habit was not included in the patient records; hence it could not be assessed as a confounder. Other studies have reported that smokers were five times more likely to have a periodontal emergency and almost two times more likely to have a dental emergency compared with non-smokers.12
The study extended for a single year and was too short to detect any changing trends over time. Other projects are currently being planned to determine the changing patterns and disease burdens presented by soldiers.
This study was carried out in Gauteng and may not be representative of the SANDF dental profile. Further studies are currently underway in different provinces to enable across the country comparisons and to identify high risk areas and soldiers.
CONCLUSION
The prevalence of dental emergency procedures among OHF I and II soldiers was relatively high and consisted predominantly of restorations, extractions and crown and bridge related issues. There were significantly more dental emergency procedures performed on OHF II, older and junior ranking soldiers than their counterparts. There were significantly more dental emergency procedures performed on Whites and Blacks compared with other races. The dental emergency profile was influenced by the OHF classification, rank, age and race.
It is recommended that studies must be carried out in different provinces and over a longer period of time to identify high risk areas and common emergency dental procedures.
Acknowledgements
The Surgeon General of the South African Military Health Service gave permission for the study. Brigadier General Derik Janse van Rensburg, director Oral Health, facilitated access to the records and offered encouragement. Military Intelligence of the South African National Defense force gave clearance for the publication. Professor PJ Van Wyk gave guidance throughout the study. All are therefore hereby acknowledged for their contributions.
ACRONYMS
OHF: Oral Health Fitness
SANDF: South African National Defence Force
References
1. Chaffin JG. Class 3 dental treatment time. Military Medicine. 2004; 169 (9): 696-9. [ Links ]
2. Chaffin J, Moss D. Review of current U.S. Army Dental Emergency Rates. Military Medicine. 2008; 173(1): 23-6. [ Links ]
3. Payne TF, Posey WR. Analysis of the dental causalities in prolonged field training exercise. Military Medicine. 1981; 146: 265-71. [ Links ]
4. Callison GM. Is a dental risk assessment predictive of dental health? Military Medicine. 2005; 170(1): 26-31. [ Links ]
5. South African Military Health Service. Oral Health Care Strategy. [Cited 2016 April 20]. Available on http://www.mhs.mil.za:800/ohcs/policies.htm. [ Links ]
6. Leiendecker T. The Department of Defence oral health and readiness. Military Medicine. 2008; 173: 1-2. [ Links ]
7. Office of the Deputy Secretary of Defense: United States Department of Defense. Profile of the military community for 2014. [Cited 2016 May 20). Available from http://www.icfi.com/workforce. [ Links ]
8. Rutherford T. Defence personnel statistics in the United Kingdom for 2014. [Cited 2016 May 20). Available from http://www.parliament.uk/briefing-papers/sn02183.pd. [ Links ]
9. Statistics South Africa. Demographics in SA in 2010. [Cited 2016 May 20). Available from http://www.statssa.gov.za/publications/P0302/P03022010.pdf . [ Links ]
10. Madiba TK, Van Wyk PJ. Evaluation of dental emergency outcomes of the Oral Health Fitness classification of the South African Military Health Service in Gauteng, South Africa. International Review of the Armed Forces Medical Services. 2014;83(3): 32-7. [ Links ]
11. Dunn WJ. Dental emergency rates at an expeditionary Medical Support Facility supporting Operation Enduring Freedom. Military Medicine. 2004; 169(5): 349-54. [ Links ]
12. Deutsch WM. Dental events during periods of isolation in the U.S. Submarine Force. Military Medicine. 2008; 173(1): 29-37. [ Links ]
13. Coovadia H, Jeukes R, Barron P, Sanders D, Mcintyre. The health and Health Systems of South Africa: Historical roots of current public health challenges. Lancet. 2009; 374: 817-34. [ Links ]
14. Nichaman M.Z, Johansen E, Rowe N, Forbes G, Garn S, Owen G.M. The effect of age, sex, race, and economic status on dental caries experience of the permanent dentition. Pediatrics. 1976; 57: 456-62. [ Links ]
15. United States, National Health and Nutrition Examination Survey, 1999-2004. Prevalence of caries in permanent teeth (DMFT) among adults 20 to 64 years of age, by selected characteristics. [Cited 2012 June 20]. Available on www.nidcr.nih.gov/DataStatistics/FindDataByTopic. [ Links ]
16. Lukas JR, Largaespadal L. Explaining sex differences in dental caries prevalence: saliva, hormones, and «life history» etiologies. American Journal of Human Biology. 2006; 18: 540-55. [ Links ]
 Correspondence:
Correspondence:
Thomas K Madiba
Department of Community Dentistry, School of Dentistry, Faculty of Health Sciences, University of Pretoria, South Africa
Tel: 012 319 2417
Cell: 084 503 6175
Fax: 086 592 4535
E-mail: thommy.madiba@gmail.com














