Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.71 n.10 Johannesburg Nov. 2016
RESEARCH
The role of socio-economic position on satisfaction with oral health services among South African adults: a structural equation model
OA Ayo-YusufI; IJ Ayo-YusufII; SA Matjila.III
IBDS, MSc, MPH, PhD. Professor & Director, School of Oral Health Sciences, Sefako Makgatho Health Sciences University, Medunsa, South Africa
IIImade J Ayo-Yusuf: BDS, MSc, PhD, Senior Lecturer, Department of Dental Management Sciences, School of Dentistry, Faculty of Health Sciences, University of Pretoria, South Africa
IIISello A Matjila: BDS, Dip Odont, MBL, Senior Lecturer & Clinical Manager, School of Oral Health Sciences, Sefako Makgatho Health Sciences University, Medunsa, South Africa
ABSTRACT
OBJECTIVE: To investigate how differences in socio-economic position (SEP) influence satisfaction with dental services among South Africans.
METHODS: Data collected from a nationally representative sample of the South African population ≥16 years old (n=3,112) included socio-demographics, health insurance enrolment, past-year dental visit and facility type (public or private), satisfaction and reason(s) for dissatisfaction with the dental services received. Using structural equation modelling, a pathway to satisfaction with dental services was tested using a number of model fit statistics.
RESULT: Of the 15.1% (n=540) who had visited a dentist in the past-year, 54.1% (n=312) were satisfied with the services received. Reasons for dissatisfaction included long waiting time (33.1%), painful procedure (13%) and rude staff (10.4%). Being of higher SEP was associated with reporting using private facility. Those who visited public facilities were more likely to have encountered a long waiting time, which in turn was associated with being more likely to report treatment as having been painful and reporting dissatisfaction. Long waiting times had the greatest direct effect on dental service dissatisfaction (β = -0.31).
CONCLUSION: Improving waiting time is likely to be the major factor to help reduce socio-economic disparities in the quality of dental services experienced by South Africans.
INTRODUCTION
Oral health status follows a socio-economic gradient.1-5 One of the possible ways in which oral health is influenced by socio-economic position, is the dental attendance patterns.6 Richard and Ameen (2002) suggested that regular dental attendance, defined as a visit to the dental clinic within a two year period, is associated with better oral health.7
Regular dental attendance is associated with several factors, one of which is the satisfaction with the dental services.8 Furthermore, socio-economic position has been shown to predict satisfaction with healthcare in South Africa.9 The symptomatic use of dental services, particularly due to having a pain-related oral problem, has been associated with significantly less satisfaction with the services received.10
The satisfaction of clients is a concern for all organisations. The subject of satisfaction and its associated factors for dental patients has not been studied extensively in South Africa. The most dominant theory of customer (patient) satisfaction is the disconfirmation theory, which holds that the customers evaluate service satisfaction by comparing their perceptions about services experienced based on their pre-experience expectations to those of the actual services received.11 The service quality model, which is widely adopted in the marketing literature, proposes a similar view that perceptions about the expected service influence how a consumer will evaluate the outcome of the service experience.12 For example, the consumer who thinks that the dental services in the public sector are bad, may have his or her evaluation of the outcome of his or her service experience clouded by his or her preconceived judgement.
To further explain the pathway of satisfaction, Zeithaml, Berry and Parasuraman presented a model that represents customer satisfaction as a product of three concepts.13 These are firstly, the desired (ideal) service, reflecting the level of service the customer wants to receive; secondly, adequate service, which is the standard of service that the customer is willing to accept; and thirdly, the predicted (expected) service, i.e. the level of service the customer believes is likely to be received.13 The quality of service received between the desired service and the adequate service represents the 'zone of tolerance'. This determines the level of satisfaction with the actual service received (i.e. if the level of the actual service received falls within the 'zone of tolerance' the person is satisfied, but if the level of service received falls below the level of 'zone of tolerance' the person is dissatisfied). Two major documented factors affecting the rating level of patient satisfaction with dental services received are the interpersonal relationship/communication and the technical skills.14
It is conceivable that the patient's socio-economic position could influence the zone of tolerance and thus the level of satisfaction with the quality of health services received. An individual's socio-economic position has an influence on the type of dental facility used, which in turn could influence the levels of both the desired service and the acceptable adequate service for that individual. Most people in possession of a Medical Aid (Private health insurance) in South Africa are likely to be of a higher socio-economic position and are likely to visit private dental facilities which are perceived to offer a higher standard of care. On the other hand, the majority of those of lower socio-economic position use the public/government dental clinics, which are characterised by long queues, overcrowding and are often understaffed. Thus, people may have to wait for long periods of time to receive the necessary attention.
The question therefore is whether merely using a private or public facility is directly or indirectly associated with the level of patient satisfaction with the services received? If there is an indirect effect, how is this mediated? Could it be by the restrictions seen to be associated with the use of public facilities?
Considering that satisfaction with past dental services may be significantly associated with future regular dental attendance, understanding the pathway that leads to patient satisfaction with dental services received may contribute to an improved oral health status by promoting regular dental visits. In particular, the use of the structural equation model would allow us to determine the pivotal pathway to dental patient satisfaction. If the pathway is so identified, application of the information could contribute to an improvement in dental patient satisfaction, especially among those of lower socio-economic position. The aim of this study was therefore to investigate how differences in socio-economic position influence patient satisfaction with dental services received among South African adults.
METHODS
Study design and sample population
This cross-sectional study used a representative sample of South African adults aged 16 years and older who participated in the Human Sciences Research Council's (HSRC) annual South African Social Attitude Survey (SASAS) during 2010 (n=3,112). The detailed sampling procedure for the SASAS, which was a household survey, has been published previously.15 Briefly, the SASAS used a multi-stage cluster sampling method to obtain a representative sample of adult South Africans, based on census enumeration areas. The survey procedure was approved by the HSRC's Research Ethics Committee (No. 6/22/09/10 6).
MEASURES
Comprehensive demographic information obtained through the survey included: participants' age, gender and current smoking status; a self-rated subjective socio-economic position on a scale of 1 to 10, with 1 representing those who see themselves as being at the bottom of the societal Manoux hierarchy;16 the area of residence categorised as rural, informal urban, and formal urban; the highest level of education attained categorised as <Grade 12, Grade 12 and >Grade 12 and medical aid (private health insurance) enrolment. The question items used were either adapted from the published literature or as used previously in past South African population surveys. The oral health-related questions included past 12-months dental visits, the type of dental facility attended (public/government or private dental clinic); the satisfaction with the dental services received and, for those who indicated being dissatisfied, the reason(s) for not being satisfied.
DATA ANALYSIS
Using structural equation modelling (SEM), an a prior model tested among past dental attendees hypothesized that a higher social position will be associated with having a medical aid. In turn that would result in a greater likelihood of using a private dental facility and having less waiting time for dental treatment which consequently leads to a higher level of satisfaction with the dental services received. The model was adjusted by removing non-significant pathways (bootstrap standardized estimates) and modified further based on inspection of modification indices. Adequacy of model fit was accessed using chi-square statistics (>0.05), Normed Fit Index (NFI) and Comparative Fit Index (CFI) of >0.9 and Root Mean Square Error of Approximation (RMSEA) ≤ 0.08.
RESULTS
Of the study participants, only 15.1% (n=540) reported a visit to a dentist in the past 12-month period. Of those who had made such a visit, 54.1% (n=312) reported being satisfied with the dental services received. Satisfaction with the past dental visit was associated with a visit to a private dental facility, being in possession of a medical aid, education levels above Grade 12 and non-smoking (Table 1). Females tended to have a more positive but not statistically significant level of satisfaction whilst age and residence bore no significant relationship to levels of satisfaction (Table 1).

A significant positive correlation between self-rated subjective socio-economic position and educational level (r=0.43; p<0.001) was observed. Those who were dissatisfied with services received were more likely to rate themselves as being of lower socio-economic position (the socio-economic ranking of those satisfied compared with those dissatisfied was 5.64 vs. 4.87; p-value < 0.001).
The most common reasons for dissatisfaction were long waiting time (33.1%), painful procedure (13%) and rude staff (10.4%) (Table 2). The fourth most common reason for dissatisfaction with dental services received was that the service was too expensive or that there was no value for money (8%), which exclusively applied to those who had visited a private dental facility.
The fit statistics suggest that the final SEM model (Figure 1) obtained fitted the data well [x2(df10)=9.3; p=0.50; NFI=0.99; CFI=1.00; RMSEA=0.00; 0.00-0.04].
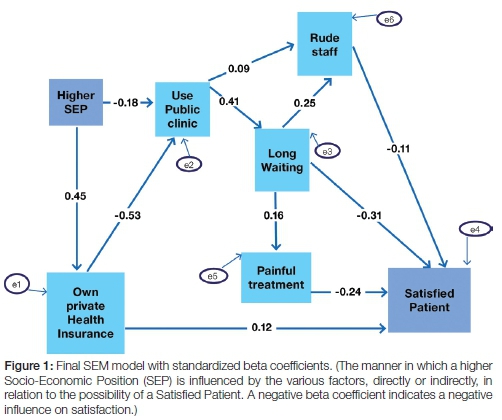
The path analysis from the structural equation model in Figure 1 demonstrates that there was no direct effect (pathway) of socio-economic position or of the use of private or public facility on the level of satisfaction with dental services. However, a long waiting time before treatment had the greatest direct effect on dental service satisfaction (β = -0.31). In addition, the long waiting time also imposed an indirect effect which was mediated through a greater likelihood of having experienced rude staff and/or painful treatment.
DISCUSSION
This study demonstrated that only about half of South African adults who had received dental service in the preceding 12 months were satisfied. Furthermore, those dissatisfied with dental services received were more likely to be of a lower socio-economic position. The three most commonly reported reasons for dissatisfaction were long waiting time (systems level), having had a painful procedure (technical skills) and experience of rude staff (interpersonal/communication). Those who were dissatisfied with dental services due to long waiting times were significantly more likely to have visited a public dental facility (Table 2). Those who were dissatisfied due to the service being too expensive and having no value for money were exclusively and significantly those who had visited a private dental facility (Table 2). This is explicable as public dental facilities are mostly free in South Africa, so expense is unlikely to be an issue.
The path analysis indicated that the pathway to satisfaction with dental services was not directly related to the type of dental facility visited (i.e. private or public) or to socio-economic position. Rather the pathway was mediated positively through possession of medical aid and negatively by long waiting times, rude staff and having had a painful dental treatment. This suggests that the disparities in perceived quality of dental services received can be addressed by attending to the mediating factors identified in this study.
Being enrolled in a Medical Aid had a direct effect on the level of satisfaction with dental services received. Medical Aid membership, found in this study to be associated with being more affluent, may contribute directly to satisfaction with dental services irrespective of the type of dental facility in which the service was delivered. Hall and Dornan (1990), had indeed previously reported that more affluent patients simply receive better treatment from health staff than do less privileged patients, even within the same health care facility. However, being a member of a Medical Aid also had an indirect effect on satisfaction for it is then more likely that the member used a private facility rather than a public facility.17 Furthermore, being in possession of medical aid may have removed the financial burden of having to pay for the visit, reducing the perception of the treatment being too expensive and hence, also diminishing the likelihood of dissatisfaction.
Those who visited a private facility were significantly more likely to have reported being satisfied with the dental services received compared with those who visited a public/government facility (Table 1). However, the path analysis demonstrates that the effect of dental facility type on reporting satisfaction with dental services received is mainly indirect, through not having experienced a long waiting time (β=-0.31) and, to a lesser extent, not having encountered rude staff (β=-0.11) nor undergone painful treatment (β=-0.24). These observations suggest that long waiting times may be the pivotal factor associated with dissatisfaction with dental services received irrespective of the type of dental facility attended, considering that such long delays influence the other two factors in the path analysis.
The use of a public dental facility as opposed to the use of a private dental facility was associated with a greater likelihood of reporting complaints about rude staff. This might be related to the fact that most of the public dental facilities are over-burdened with large numbers of patients, all trying to seek care from a limited number of clinical operators who themselves are overworked and could conceivably become frustrated. Those who reported waiting for long periods were also more likely to have reported experiencing rude staff and, interestingly, were also more likely to have reported having had a painful procedure, both factors associated with dissatisfaction with dental services. It could be that the long waiting time might have actually reduced the 'zone of tolerance' or level of tolerance to pain. However, the experience of having had painful treatment may also be dependent on the procedure that the person underwent. This factor was not significantly different between those who visited a private, or those who visited a public, facility (Table 2).
Similarly, the long wait may have made the people less tolerant to the attitude of the dental staff and consequently may have perceived the harassed staff as rude. Alternatively, the agitated patients may, in their bid to secure more immediate attention, have in fact provoked the staff who reacted in a manner that may be considered rude.
The National Department of Health18 recently introduced National Core Standards to improve the quality of care received. The successful enhancement of value and attitudes; and the reduction of waiting times, two of the six standards,19 hopefully should reduce dissatisfaction with dental care. There will nevertheless be a need for further studies to assess whether the implementation of these National Core Standards actually improve satisfaction with services as may be inferred from the results of this study.
LIMITATIONS OF THE STUDY
The cross-sectional study design limits possible inferences on causality. The use of structural equation modelling, however, did provide some possible causal pathways that can be tested in future longitudinal studies.
The respondents were not asked what procedure they had received and how they paid for the procedure, and whether they paid the Board of Health Funders (BHF) rates or not. The recall bias may have influenced the responses of the respondents. Furthermore, there may be other reasons for dissatisfaction which were not captured/included in this study. A large number of study participants indeed selected 'other' reasons without specifying what those reasons were, even though they were provided with that option. Although the data were collected in 2010, it is unlikely that the structural elements of the relationship described in this study would have changed to any extent.
CONCLUSIONS AND RECOMMENDATIONS
The SEM analysis confirms that there is a relationship between SEP and patient satisfaction with dental services and identifies some of the factors influencing that relationship. Although there is need for further studies on the influence of more service quality attributes, it appears that waiting time influences the 'zone of tolerance'. Therefore, interventions aimed at improving dental attendance, particularly for people of low-income, should include among other things a reduction in waiting time or perhaps prior information to patients on expected waiting time which can be regularly updated by staff, and in a polite manner. Other interventions could include the use of positive distractions for the people waiting for dental treatment to reduce the boredom of a long wait, and also the training of staff in the dental facility on customer care. Nevertheless, every effort should be put in place to reduce the waiting time for dental treatment such that it remains within the 'zone of tolerance'.
The findings of this study may also be seen to highlight the potential for the introduction of the National Health Insurance (NHI) to directly improve satisfaction with service received and thus to encourage more regular use of dental services and the promotion of prevention of dental disease. In particular, the findings suggest the need to focus on waiting time as an important performance standard when service agreements are signed with potential National Health Insurance (NHI) service providers, irrespective of whether they are located in a public or a private facility.
Conflict of interests: None declared
ACRONYMS
BHF: Board of Healthcare Funders
CFI: Comparative Fit Index
HSRC: Human Sciences Research Council
NFI: Normed Fit Index
NHI: National Health Insurance
RMSEA: Root Mean Square Error of Approximation
SASAS: South African Social Attitude Survey
SEM: Structural Equation Modelling
References
1. Watt R, Sheiham A. Inequalities in oral health: a review of the evidence and recommendations for action. Br Dent J 1999; 187: 6-12. [ Links ]
2. Chavers LS, Gilbert GH, Shelton BJ. Racial and socioeconomic disparity in oral disadvantage, a measure of oral health-related quality of life: 24-months incidence. J Public Health Dent 2002; 62: 140-7. [ Links ]
3. Sanders AE, Slade GD, Turrell G, Spencer AJ, Marcenes W. The shape of the socioeconomic-oral health gradient: implications for theoretical explanations. Community Dent Oral Epidemiol 2006; 34: 310-9. [ Links ]
4. Sabbah W, Tsakos G, Chandola T, Sheiham A Watt RG. Social gradient in oral and general health. J Dent Res 2007; 86: 992-6. [ Links ]
5. Jung S-H, Watt RG, Sheiham A, Tsakos G. Exploring pathways for socioeconomic inequalities in self-reported oral symptoms among Korean adolescents. Community Dent Oral Epidemiol 2011; 39: 221-9. [ Links ]
6. Donaldson AN, Everitt B, Newton T, Steele J, Sherriff M, Bower E. The effects of social class and dental attendance on oral health. J Dent Res 2008; 87(1):60-4. [ Links ]
7. Richards W, Ameen J. The impact of attendance patterns on oral health in a general dental practice. BDJ 2002; 193(12) 697-702. [ Links ]
8. Liddell A and Locker D. Dental satisfaction in a group of adults aged 50 years and over. J Behavioural Med 1992; 15: 415-27 [ Links ]
9. Myburgh NG, Solanki GC, Smith MJ and Lalloo R. Patient satisfaction with healthcare providers in South Africa: the influences of race and socioeconomic status. Int J Quality in HealthCare 2005; 17: 473-7 [ Links ]
10. Riley JL 3rd, Gilbert GH, Heft MW. Orofacial pain: patient satisfaction and delay of urgent care. Public Health Report, 2005; 120: 140-9 [ Links ]
11. Oliver R. A cognitive model of the antecedents and consequences of satisfaction decisions, J Marketing Res, 1980; 17:460-9. [ Links ]
12. Gronroos CA Service quality model and its marketing implications. European J Marketing, 1984; 18, 4:36-44. [ Links ]
13. Zeithaml VA., Berry LL, Parasuraman A., The nature and determinants of customer expectations of service. J Academy Marketing Sci, 1993;21 (1): 1-12. [ Links ]
14. Gürdal P, Çankaya H, Önem E, Dınçer S, Yílmaz T: Factors of patient satisfaction/ dissatisfaction in a dental faculty outpatient clinic in Turkey. Comm Dentist Oral Epidemiol 2000; 28: 461-9. [ Links ]
15. Olutola BG, Ayo-Yusuf OA. Socio-environmental factors associated with self-rated oral health in South Africa: a multilevel effects model. Int J Environmental Res Pub Health 2012; 9: 3465-83. [ Links ]
16. Singh-Manoux A, Marmont M, Adler NE. Does subjective social status predict health and change in health status better than objective status? Psychosomatic Medicine 2005; 67: 855-61. [ Links ]
17. Hall JA, Dornan MC. Patient socio-demographic characteristics as predictors of satisfaction with medical care: a meta-analysis. Soc Sci & Med. 1990; 30(7): 811-8. [ Links ]
18. National Department of Health. National Core Standards for Health Establishments in South Africa. Pretoria: National Department of Health; 2011. [ Links ]
19. Whittaker S, Shaw C, Spieker N, Linegar A.. Quality standards for Health Care Establishments in South Africa. SAHR 2011, pp59- 68. [ Links ]
 Correspondence:
Correspondence:
OA Ayo-Yusuf
E-mail: lekan.ayo-yusuf@smu.ac.za













