Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.71 no.9 Johannesburg Out. 2016
CASE REPORT
Submandibular calcification: A report on two cases and a review
B BuchI; M MachakaII; M MabongoIII
IBSc Hons (Natal); SED (UCT); BDS (Wits); MSc Dent (Wits). Emeritus Professor-University of Pretoria, Visiting Professor and Part-time Consultant: Division of Maxillo-Facial and Oral Radiology, Department of General Dental Practice, School of Oral Health Sciences, University of the Witwatersrand, Johannesburg
IIBDS (Medunsa); Dip Odont (UP). Registrar, Department of Maxillo-Facial and Oral Surgery, School of Oral Health Sciences, University of the Witwatersrand, Johannesburg
IIIBDS (Wits); MChD (UWC); Head: Clinical Unit, Department of Maxillo-Facial Surgery, School of Oral Health Sciences, University of the Witwatersrand, Johannesburg
ABSTRACT
Two cases of sialoliths. a.) A 32 year-old female, referred to the Wits Oral Health Centre by a private periodontist who suspected a stone in the submandibular duct. The patient experienced a sharp stabbing pain beneath the right side of her chin, exacerbated on eating. Intraoral palpation of the duct revealed nothing. Panoramic and scanning radiography confirmed a small radiopaque sialolith near the angle of the mandible, measuring 6.43mm in diameter. Sialography determined it was wedged within the genu of the duct. Surgical access was difficult, possibly leading to removal of the entire gland. As the pain had subsided, the patient will be monitored over the following few months. b.) A fifty two year-old male patient with a three year history of pain and swelling on the right side of his face. Previous medical consultations failed to diagnose the cause. Intraorally a creamy-white, bony-hard lesion was visible, perforating through the sublingual mucosa. Various radiographs confirmed the presence of a giant sialolith, measured on cone-beam scan at 25 x 26mm. Excisional biopsy easily shelled out the stone The resultant cavity was marsupialized and the defect sutured. Possible causes of Sialolithiasis, the various imaging modalities and alternative treatment options are discussed.
CASE REPORTS
Case 1
A thirty two year-old female patient presented at the Wits Oral Health Centre complaining of a sharp stabbing pain beneath the right side of her chin. Her pain was much exacerbated during meals and had been of about two months' duration. She had previously consulted a private periodontist who, on the basis of her symptoms, had diagnosed a possible submandibular sialolith. He had referred her to the Wits Oral Health Centre for confirmation and possible treatment.
A slight swelling was visible beneath the right side of the patient's chin although nothing distinctive was palpable intraorally along the superficial course of the submandibular duct.
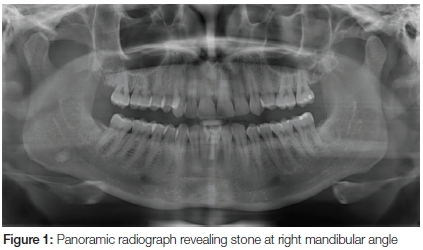
A panoramic radiograph revealed a small radiopacity surrounded by a radiolucent periphery near the angle of the mandible beneath the inferior alveolar canal (Figure 1). The radiographic appearance together with the patient's symptoms confirmed the presence of a sialolith.
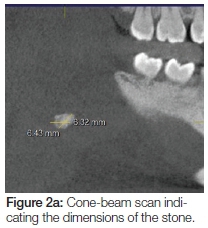
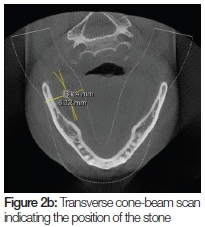
A cone-beam scan was undertaken in order to establish the size of the stone and its relative position with respect to the medial border of the mandible (Figure 2 A and B). The stone was found to measure 6.43mm in greatest diameter.
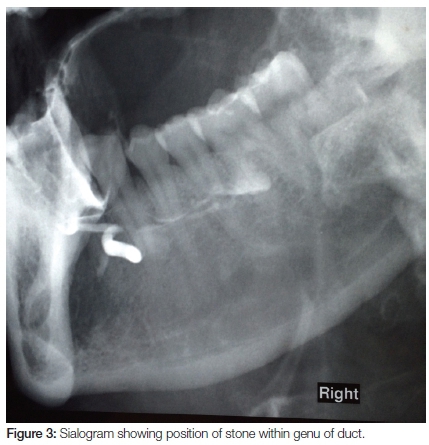
A sialogram was performed in order to determine the exact location of the stone within the submandibular duct. This revealed that the sialolith was wedged within the genu of the duct, causing a blockage, thereby preventing filling of the parenchyma of the gland by the contrast medium (Figure 3).
The small size of the stone together with its awkward position in the duct would make surgical removal difficult without damaging the duct. This might necessitate the removal of the entire gland.
Since the patient's pain had by then somewhat subsided, it was decided to monitor the patient over the following few months in order to determine whether the duct might adapt over the course of time or otherwise the stone may possibly move to a more accessible position, enabling easier surgical access.
Case 2
A fifty two year-old male patient presented at the Wits Oral Health Centre complaining of a painful swelling on the right side of his face (Figure 4). His symptoms were of three years' duration. He had previously consulted a medical practitioner who informed him that his skin had reacted to shaving. The patient was treated with numerous courses of analgesics and antibiotics to no avail. The patient then sought treatment at the Wits Oral Health Centre.

On intra-oral examination a creamy-white, bony hard lesion was visible lingual to the 47/48 region which was beginning to perforate through the sublingual mucosa (Figure 5). A preliminary diagnosis of a salivary sialolith was made.

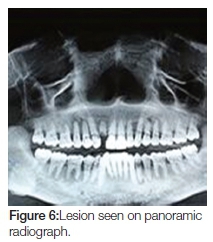
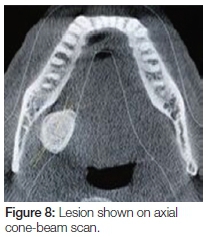
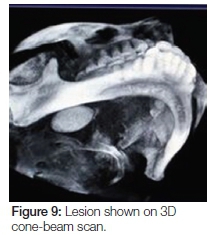
Panoramic, lateral oblique and cone-beam radiographs were taken, all of which revealed a large radiopaque lesion apical to the 48. This confirmed the presence of a sialolith (Figures 6, 7, 8, 9).

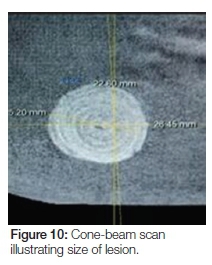
The lesion on cone-beam was seen to measure 25 x 26 mm in diameter (Figure 10). This, according to modern literature, would be considered a giant sialolith.
An excisional biopsy was performed under local anaesthetic and a creamy-white chalk-like substance was easily shelled out. Marsupialization of the resultant cavity was carried out and the defect sutured with 3/0 chromium catgut.
The patient recovered well and uneventfully from the procedure and was followed up for two months. At the final visit the saliva was seen to be draining well through the residual opening at the surgical site.
DISCUSSION
Before the advent of modern imaging modalities which today are somewhat taken for granted, radiological diagnosis of salivary gland pathoses was carried out by means of sialography.
Sialography is the process of demonstrating the duct system of salivary glands radiographically by injection of radiopaque media, the medium of choice being iodized oil.1,2 Calculi, the most common cause of duct obstruction, may be seen on plain x-ray films (termed scout films in sialography) provided that the calculus is radiopaque. Despite this fact, however, the use of a sialogram would pinpoint its exact position in the duct, aiding surgical planning. However, an estimated 20% of calculi are radiolucent and could therefore only be detected on a sialogram. Furthermore, sialography was indicated in cases of suspected strictures of the duct. Sialography, though, is contraindicated in all acute inflammatory diseases since injection of foreign material and insertion of instruments into the duct system is highly deleterious.2
With the advent of CT, Ultrasound, MRI and Cone-Beam imaging, routine sialography using plain x-rays has become almost obsolete with the exception of the occasional sialogram performed on a CT scan for a particular purpose. In the first reported case above, in view of the fact that the stone was not palpable in the mouth, the decision was taken to resort to sialography to determine its exact position in the duct.
Sialolithiasis is one of the most common diseases of salivary glands accounting for about 50% of salivary gland pathoses.3,4 It refers to the formation of calcifications within the ducts or parenchyma of the gland.4 The greater majority of stones (80-90%) are found in the submandibular gland.5-7 The reasons for this as often quoted are that the submandibular duct is very tortuous with a marked genu together with the increased viscosity of its secretions.6 There appears to be an indication that patients with salivary stones may be prone to develop nephrolithiasis.7
The exact cause of calculus formation is not fully known but a number of factors have been cited as contributory. These include altered calcium metabolism, altered pH, dehydration, poor eating, and the use of certain drugs such as antihistamines, anti-hypertensives, psychiatric and bladder- control drugs. Tobacco chewing has also been cited as a factor. There also appears to be an association between salivary calculi and certain other conditions like gout, nephrolithiasis and liver disease.8 In the UK it was postulated that residents of hard water areas were at risk of developing Sialolithiasis. However, a study by Sherman and McGurk based on statistics for the years 1991 to 1994 showed that water hardness was not significantly associated with the development of salivary calculi.9
Since not all stones are radiopaque, plain x-rays are not always able to detect such stones which may be in the duct or in the parenchyma of the gland.6 Ultrasound appears to be well-established in cases where Sialolithiasis is clinically suspected but not evident on plain x-rays.10 MRI scans have been utilized for visualising stones as well as for mapping the ductal anatomy of the gland. CT may also be used for this purpose but is not as effective as MRI.4,5 These modalities, however, are somewhat costly and are not routinely used.
Sialoliths measuring 25mm or more are termed giant sialoliths. Krishnan et al3 have reported on two cases and maintain that giant sialoliths have rarely been reported in the literature. However, a very superficial search of the literature has revealed a further five cases,8,11-14 and our second reported case would also fall into this category. The occurrence of giant sialoliths may therefore not be as rare as was stated.
The treatment of choice for most salivary stones, particularly very large ones, has for decades been surgery. However, non-surgical options are now being used to treat symptomatic stones. These include extracorporeal shock wave sialolithotripsy, balloon dilatation, endoscopic removal and laser therapy.4,8
Conflict of Interest: None declared.
References
1. Ollerenshaw RGW, Rose SS. Radiological diagnosis of salivary gland disease. Brit J Radiol. 1951; 24: 538-48 [ Links ]
2. Blatt IM, Rubin P, French AJ, Maxwell JH, Holt JF. Secretory sialography in diseases of the major salivary glands. Annals of Otorhinolaryngology. 1956; 56(2): 295-316 [ Links ]
3. Krishnan B, EL Gehani R, Il Shehumi M. Submandibular giant sialoliths-two case reports and review of the literature. Indian J Otolaryngol Head Neck Surg. 2009; 61: 55-8 [ Links ]
4. Becker M, Marchal F, Becker CD et al. Sialoliths and salivary ductal stenosis: diagnostic accuracy of MR sialography with a three-dimensional extended-phase conjugate-symmetry rapid spin-echo sequence. Radiology. 2000; 217(2): 347-58 [ Links ]
5. Jager L, Menauer F, Holzknecht N et al. Sialolithiasis: MR sialography of the submandibular duct-an alternative to conventional sialography. Radiology. 2000; 216(3): 665-71 [ Links ]
6. Kraaij S, Karagozoglu KH, Forouzanfar T et al. Salivary stones: symptoms, aetiology, biochemical composition and treatment. Br Dent J. 2014; 217(11): 1038-54 [ Links ]
7. Lustmann J, Regev E, Melamed Y. Sialolithiasis. A survey on 245 patients and a review of the literature. Int J Maxillofac Surg. 1990; 19(3): 135-8 [ Links ]
8. Fefar AD, Jivani PS, Mehta MR et al. A huge salivary calculus of the submandibular gland: a case report with a review of the literature. J Med Res. 2015; 1(1): 5-7 [ Links ]
9. Sherman JA, McGurk M. Lack of correlation between water hardness and salivary calculi in England. Br J Maxillofac Surg. 2000; 38(1): 50-3 [ Links ]
10. Gritzman N. Sonography of the salivary glands. Am J Roentgenol. 1989; 153(1): 161-6 [ Links ]
11. Carr SJ. Sialolith of unusual size and configuration. Oral Surg Oral Med Oral Path Oral Radiol Endod. 1965; 7: 709-12 [ Links ]
12. Bodner L. Giant salivary gland calculi: diagnostic imaging and surgical management. Oral Surg Oral Med Oral Path Oral Radiol Endod. 2002; 94: 320-3 [ Links ]
13. Leung AK, Choi MC, Wagner GA. Multiple sialoliths and a sialolith of unusual size in the submandibular duct. Oral Surg Oral Med Oral Path Oral Radiol Endod. 1999; 87: 331-3 [ Links ]
14. Siddiqui SJ. Sialolithiasis: An unusually large submandibular salivary stone. Br J Oral Surg. 1981; 19: 230-3 [ Links ]
 Correspondence:
Correspondence:
Brian Buch
Tel: 011 488 4854
E-mail: Brian.Buch@wits.ac.za













