Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.71 no.5 Johannesburg Jun. 2016
RESEARCH
The psychological impact of malocclusion on patients seeking orthodontic treatment at a South African oral health training centre
DP MotlobaI; MPS SethusaII; OA Ayo-YusufIII
IBDS, MPH (Epid), MDent (Comm.Dent), MBL. Head, Department of Community Dentistry. School of Oral Health Sciences, Sefako Makgatho Health Sciences University
IIB (Diag) Rad, BDS, PDD, M Dent (Orthodontics), P G Dip (UCT). Head of the Department of Orthodontics. School of Oral Health Sciences, Sefako Makgatho Health Sciences University
IIIBDS, MSc Odont, DHSM, MPH, PhD. Professor and Director, School of Oral Health Sciences, Sefako Makgatho Health Sciences University
ABSTRACT
OBJECTIVE: The study set out to assess the psychosocial impact of dental aesthetics among a sample of patients seeking orthodontic treatment at Medunsa Oral Health Centre (MOHC), Sefako Makgatho Health Sciences University (SMU).
METHODS: One hundred and fifty patients (100 females and 50 males, aged 13-29 years) presenting for orthodontic treatment were prospectively enrolled. Following comprehensive orthodontic clinical examination, patients were requested to complete the Psychosocial Impact of Dental Aesthetics Questionnaire (PIDAQ), which was supplemented by a few additional items. The data were analysed using Chi-square, Student's t-tests and ANOVA.
RESULTS: The questionnaire demonstrated good reliability, with a Cronbach score of 0.85. Total psychological impact and particularly social impact were significantly greater among those older than 18 years (p =0.017) than amongst the younger patients (p= 0.035), and dental self-confidence was significantly higher among females than males (p = 0.045). Self-perceived malocclusion had a significant positive association with aesthetic concern (p = 0.036).
CONCLUSION: Malocclusion, particularly when self-perceived, has a significant negative impact on the psychological wellbeing of patients, especially for those older and male. Orthodontic treatment may result in improved oral health-related quality of life and thus enhance the general psychological wellbeing of patients.
INTRODUCTION
Health-related quality of life indicates the individual's perception or assessment of the impact of disease or conditions on their (i) functional, (ii) psychological, and (iii) social well-being.1 Poor oral health-related quality of life (ORHQoL) is indicative of the expressed negative impact of oral conditions on the multidimensional attributes of the individual's life. Aesthetic appearance, morphology of the facial structure, of the oral cavity and smile social interaction. Hence judgements about the attractiveness of the facial profile especially teeth and jaws, can have a huge impact on the social and psychological wellbeing of a person.2,3 The literature suggests that psychological and social effects rather than functional attributes are compelling reasons why patients seek orthodontic treatment.4
Orthodontics has been perceived as generally addressing normative clinician-based concerns with less regard for the equally important preferences and aspirations of the patient.5 Hence the recommendation that ORHQoL measures be integrated in the clinical management of patients for improved outcomes and satisfaction.
Orthodontic treatment is commonly undertaken during adolescence and young adult life. Coincidentally, patients in these age groups are acutely aware of their appearance, recognise any physical deviation from normal, and are more concerned about their social position and independence.6 Hence the expectation that adolescents and youth with untreated malocclusion will experience psychological and social impact and poor oral health-related quality of life.
Numerous instruments have been used to measure the impact of oral conditions of the quality of life. The Oral Health Impact Profile (OHIP) is the most widely used tool and is based on Locker's conceptual model.7 The Psychological Impact of Dental Aesthetics Questionnaire (PIDAQ) is gaining popularity among researchers as a tool to assess self-rated psychological impact of dental aesthetics among young patients.8 This questionnaire was developed in English-speaking countries but has since been adapted to other languages and has been found to be reliable,9-12 although only limited information is available on the reliability of this instrument in Africa. The effect of malocclusion status on subjective psychological well-being of young South Africans, particularly as it relates to normative measures used in orthodontics, has also not been widely researched.
The aim of this study is therefore to evaluate the psychological impact of malocclusion on a cohort of black South African patients seeking orthodontic treatment at a South African oral health training centre.
METHODOLOGY
All patients aged 13-29 years, screened during March to December 2015 at the Department of Orthodontics at one of the four oral health training centres in South Africa were invited to participate in this study. Using OpenEpi, Ver3, with power (1 - β) set at 0.80 and α = 05 for two-tailed tests, the recommended sample size was estimated to be n= 138, 140 and 154 respectively.13,14 It was consequently determined that a sample of 150 participants would be sufficient to detect the 10% levels of group differences in measures of psychological impact. Eligible and consenting participants underwent comprehensive orthodontic clinical assessment and completed self-administered questionnaires. In the case of minors, accompanying guardians gave permission for the children to participate in the study. Through these assessments, the following variables were measured (i) clinician assessed malocclusion or normative malocclusion (NM), (ii) self- assessed malocclusion or self-perceived malocclusion (SPM), (iii) and psychological impact of malocclusion using PIDAQ.
Assessment of normative malocclusion and self-perceived malocclusion
The clinical assessments of patients were undertaken by calibrated 3rd and 4th year orthodontic registrars/residents who were in a four-year specialist training programme. The normative assessment was done using clinical evaluation, cast models and cephalometric radiographs. Following this assessment, patients were classified as having mild, moderate or severe malocclusion, and as needing simple to complex intervention. To evaluate self-perceived malocclusion, previously tested questions from different questionnaires were incorporated into the PIDAQ which was then completed by the study participants,10,12 who graded their responses to these additional questions based on a 7 point Likert scale. Questions such as: "how do you feel about appearance of your teeth" and "do you cover your mouth because of appearance of your teeth" were applied to elicit the perception of participants of their malocclusion.15
Psychological impact of malocclusion (using PIDAQ)
The PIDAQ is a questionnaire specifically designed for assessing the psychosocial impact of dental aesthetics in young adults. This instrument was developed and tested on similar population groups and is composed of 23 items and four subscales.10,12 The Dental Self-confidence index is a positive subscale (DSC; 6 items), but Aesthetic Concern (AC; 3 items), Psychological Impact (PI; 6 items) and Social Impact (SI; 8 items) are negatively worded subscales i.e. for the latter three subscales, the higher the score the more severe the psychological impact. The response options were based on a five-point Likert scale ranging from 0 to 4 (i.e. 0 - no impact of dental aesthetics on QoL, to maximal impact - 4). For purposes of this study the English version of PIDAQ was used without translation. However the tool was tested for internal consistency and homogeneity between items using Cronbach's alpha.
Statistical data analysis
Data were analysed using SPSS version 23.0 (IBM Corp 2010). The subjects were categorised into three groups according to the estimated severity of malocclusions (mild, moderate and severe).
Additive scales and subscales for PIDAQ -23 were calculated by summing the responses to the various items. The variables in the dental self-confidence sub- scale (items 1 to 6) were reverse coded to bring the direction of the scores into line with the other three subscales. Descriptive statistics, such as mean, median and proportions were used to enumerate population characteristics. Mean differences in psychological impact of malocclusion across categories were compared using Student's t-test in the case of two group mean differences, and analysis of variance for means differences across three or more groups. Statistical differences in the proportion across groups or categories were tested using Chi-square statistics. All statistical tests were two tailed and the level of statistical significant was set at p<0.05.
RESULTS
A total of 150 participants agreed to undergo clinical examination and completed a structured questionnaire. By gender, two-thirds (100) were female, in terms of age, 55.3 %( 83) were younger than 19 years, with a mean age of 14.52 years (standard deviation 5.10). (Table 1). Based on normative evaluation of malocclusion, 75.3% (113) of participants were classified as having moderate to severe malocclusion. A similar proportion (76%; n=114) of the study participants self-perceived their malocclusion to be moderate to severe. It was however observed that participants tended to under-report the 'severe' category of malocclusion (17.3 %; n= 26) when compared with clinical findings by the orthodontic registrars (38%; n=57), who relied on normative measures (Table 1).

Cronbach's alpha of 0.85 shows an excellent degree of internal consistency or scale reliability and homogeneity between the scale items. Similarly, the subscales of PIDAQ were highly correlated, with Cronbach alpha coefficients ranging from 0.81 to 0.92.
The mean and 95% confidence interval for total PIDAQ score was 45.26 (95% CI=42.64 to 47.87). The mean DSC was 8.82 (7.81 - 9.83), SI score 12.54 (12.25 - 14.82), PI 15.05 (14.17 - 16.13), and AC 7.76 (7.06 - 8.45).
Our study shows no significant association between psychological impact and age except for the total PIDAQ and social impact subscale for which those older than 18 years had significantly higher scores (p =0.017 and 0.05 respectively). No significant differences were also noted by gender in the total and subscales, except for DSC for which males reported significantly worse scores than females (p =0.045). A one-way ANOVA was conducted to compare the mean scores on the PIDAQ and its subscales across the three self-perceived and normatively determined malocclusion categories. The results showed a significant association between categories of self-assessed malocclusion and reported aesthetic concern (p=0.036). Post hoc comparisons using the Fisher's least significant difference (LSD) test indicated that the aesthetic concerns were significantly lower among participants who reported they perceived their malocclusion as 'mild' as compared with that amongst those who perceived their malocclusion as 'moderate' (p=0.021) or severe (p=0.026). However, aesthetic concerns did not differ significantly between moderate and severe SPM (p=0.595) (Table 2). Furthermore, there were no significant differences in mean PIDAQ or its subscales across the categories of normative malocclusion (Table 2).
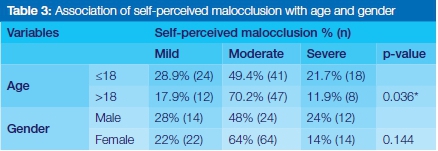
Self-perceived malocclusion was significantly associated with age but not with gender. Compared with those older than 18 years, the younger participants reported their malocclusion significantly more frequently as either mild or severe. Those older were significantly more often likely to report their malocclusion as moderate (Table 3).
DISCUSSION
This study examined the impact of malocclusion on the overall psychological wellbeing and its PIDAQ subscales among 13-29 year olds seeking dental treatment at MOHC. It was found that twice as many females than males sought orthodontic treatment at the centre. This finding is in agreement with previous studies that females have a significantly higher uptake of orthodontic treatment than males.16,17 It is postulated that this is because girls are frequently and intensely dissatisfied with their dental appearance,16,18 tend to put a higher priority on their physical appearance, and appreciate the social significance and expectation of aesthetics more than do male counterparts.17 It can also be considered that parents might be socialised to seek orthodontic treatment for their daughters rather than their sons.16
Differences in self-perception of malocclusion between genders were statistically insignificant (p=0.144). This result supports findings by Peres19 and Batool20 but contradicts others.21,22 The absence of consensus in the literature about the gender differences and perceived malocclusion, may be attributed to methodological variation, resulting in a failure to detect the presence of statistical inconsistencies.
Our study, similar to many, has evaluated the psychological impact of malocclusion on young adults9,23 compared with adolescents and teenagers.12,24 We found heightened perceptions of severe malocclusion by younger participants, similarly reported by Aikins et al,21 Peres et al,19 Klages et al,25 and refuted by Jawad et al.26
It has been found that increasingly, adolescents and the young report for orthodontic care primarily to address the aesthetic and social effects of malocclusion, and secondarily to manage functional problems.26 The impact of malocclusion in this age group can be attributed to cohort effects. Age cohorts are exposed to similar social events, common experiences, influences and demographic trends and tend to adopt and display comparable but unique behaviour patterns over time. Nowadays, appearance, beautiful smiles and acceptance have become are paramount in advancing social equity, given the proliferation of technology and information. It may thus be expected that the younger age group will seek intervention, like orthodontic treatment, to advance their social positions. In addition, this group is exposed to acceptance o a social image through social media and related technology.
The mean total PIDAQ of 45.26 in our study is comparable with the findings observed from similar population groups elsewhere of 47.9327 and 47.128. These scores are indicative of the overwhelming impact of dental aesthetics on the psychological wellbeing of patients.
The literature corroborates our results that total PIDAQ and its subscales do not differ significantly by gender, except for DSC.24,28 We observed high DSC scores in males, suggesting that males displayed lower self-confidence and self-assurance about their teeth, and consequently suffering a greater negative psychological impact of malocclusion. Our results are contradictory to the established and socialised norm, that women are more likely than men to worry about how their teeth look, and hence display a heightened impact of malocclusion.17,26
It is possible to hypothesise an emerging phenomenon specific to African subjects as represented by the participants in our study. Notably, more adults and more males are seeking orthodontic care to address primarily the aesthetic and psychological consequences of malocclusion. This occurrence could be attributed to improved socioeconomic positions, increased oral health awareness, changing perceptions about self-image especially in males, and improved access to orthodontic treatment. As a result, teaching institutions like MOHC are observing an increased demand for orthodontic treatment by previously underserved population groups, who now are finding these services to be more affordable and attainable.
CONCLUSION
There is no previously published study on the psychological impact of malocclusion in South Africa. While this study cannot be seen as representative of the whole population, it does provide a reasonable impression of the reaction to malocclusion amongst orthodontic patients in this area and facility.
This cross sectional study has validated the reliability of PIDAQ in the South African population group seeking orthodontic treatment, and provided evidence on the impact of dental aesthetics on oral health related quality of life and specifically the psychological impact. Additionally, the findings reveal that the perceptions of an individual of their malocclusion had a greater impact on their psychological and social wellbeing than did clinician assessed status of malocclusion. Malocclusion has a significant negative impact on the psychological wellbeing of patients, especially for those older and male.
Recommendations
These results imply that teaching institutions and private healthcare should incorporate adult orthodontics in the curriculum and that the available treatment modalities should be discussed, given the increasing demand for care from this population group.
More comprehensive studies should be conducted in the future. Significant moderating and intervening factors between perceived malocclusion and its impact should be explored to provide a greater understanding of this relationship. Novel approaches should incorporate a pre-post design to evaluate the definitive impact of orthodontic treatment.
ACRONYMS
AC: aesthetic concern
DSC: dental self-confidence
LSD: least significant difference
MOHC: Medunsa Oral Health Centre
NM: normative malocclusion
OHIP: Oral Health Impact Profile
PI: Psychological Impact
PIDAQ: Psychosocial Impact of Dental Aesthetics Questionnaire
SI: Social Impact
SMU: Sefako Makgatho Health Sciences University
SPM: Self- assessed Malocclusion or Self-perceived Malocclusion
References
1. Allison, PJ, Locker, D, Feine, JS. Quality of life: a dynamic construct. Soc Sci Med. 1997;45:221-30. [ Links ]
2. de Oliveira, CM, Sheiham, A. Orthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescents. J Orthod. 2004;31: 20-7; discussion 15, doi:10.1179/146531204225011364 . [ Links ]
3. Liu, Z, McGrath, C, Hagg, U. The impact of malocclusion/orthodontic treatment need on the quality of life. A systematic review. Angle Orthod. 2009;79:585-91, doi:10.2319/042108-224.1. [ Links ]
4. Marques, LS. et al. Self-perception regarding the need for orthodontic treatment among impoverished schoolchildren in Brazil. Eur J Paediatr Dent. 2009;10:125-30. [ Links ]
5. Marques, L S, Ramos-Jorge, M L, Paiva, S M., Pordeus, I A. Malocclusion: esthetic impact and quality of life among Brazilian schoolchildren. Am J Orthod Dentofacial Orthop. 2006;129:424-7, doi:10.1016/j.ajodo.2005.11.003. [ Links ]
6. Mandall, N , Wright, J, Conboy, FM, O'Brien, KD. The relationship between normative orthodontic treatment need and measures of consumer perception. Community Dent Health. 2001;18: 3-6. [ Links ]
7. Locker, D. Measuring oral health: a conceptual framework. Community Dent Health. 1988; 5: 3-18. [ Links ]
8. Klages, U, Claus, N, Wehrbein, H, Zentner, A. Development of a questionnaire for assessment of the psychosocial impact of dental aesthetics in young adults. Eur J Orthod. 2006; 28: 103-11, doi:10.1093/ejo/cji083 . [ Links ]
9. Klages, U, Rost, F, Wehrbein, H, Zentner, A. Perception of occlusion, psychological impact of dental esthetics, history of orthodontic treatment and their relation to oral health in naval recruits. Angle Orthod. 2007;77:675-80, doi:10.2319/061206-237.1. [ Links ]
10. Lin, H. et. al. Translation and validation of the Chinese version of the psychosocial impact of dental aesthetics questionnaire. Eur J Orthod. 2013; 35:354-60, doi:10.1093/ejo/cjr136. [ Links ]
11. Montiel-Company, J M, Bellot-Arcis, C, Almerich-Silla, J M. Validation of the psychosocial impact of dental aesthetics questionnaire (PIDAQ) in Spanish adolescents. Med Oral Patol Oral Cir Bucal. 2013; 18:e168-73. [ Links ]
12. Sardenberg, F, Oliveira, AC, Paiva, SM. Auad, SM, Vale, M P. Validity and reliability of the Brazilian version of the psychosocial impact of dental aesthetics questionnaire. Eur J Orthod.2011;33: 270-5, doi:10.1093/ejo/cjq066. [ Links ]
13. Fleiss, JL, Levin, B, Paik, MC. Statistical Methods for Rates and Proportions. John Wiley & Sons, 2013. [ Links ]
14. Kelsey, J L. Methods in Observational Epidemiology. Vol. 26 Oxford University Press, USA, 1996. [ Links ]
15. Claudino, D, Traebert, J. Malocclusion, dental aesthetic self-perception and quality of life in a 18 to 21 year-old population: a cross section study. BMC Oral Health. 2013;13: 1 . [ Links ]
16. Badran, SA, Al Khateeb, S. Factors influencing the uptake of orthodontic treatment. Journal of Public Health Dentistry. 2013;73: 339-44. [ Links ]
17. Harris, EF, Glassell, BE. Sex differences in the uptake of orthodontic services among adolescents in the United States. Am J Orthod Dentofacial Orthop. 2011; 140:543-9. [ Links ]
18. Shaw, W. Factors influencing the desire for orthodontic treatment. Eur J Orthod.1981; 3:151-62. [ Links ]
19. Peres, S H d CS, et al. Self-perception and malocclusion and their relation to oral appearance and function. Ciência & Saúde Coletiva.2011;16:4059-66 . [ Links ]
20. Batool, I, Abbas, A, Imtiaz, A, Zulfiqar, K. Psychological effect of malocclusion. Pakistan Orthodontic Journal.2009; 1: 17-22 . [ Links ]
21. Aikins, E, Dacosta, O, Onyeaso, C, Isiekwe, M. Self-perception of malocclusion among Nigerian adolescents using the aesthetic component of the IOTN. The Open Dentistry Journal. 2012;6:61-66 [ Links ]
22. Spalj, S, et al. Mediation and moderation effect of the big five personality traits on the relationship between self-perceived malocclusion and psychosocial impact of dental esthetics. The Angle Orthodontist. (2015). 2016;6:61-6 [ Links ]
23. Ali Mahmood, TM, Kareem, FA. Psychological impact of dental aesthetics for Kurdish young adults seeking orthdontic treatment. Int J of Health and Rehabilatation Sciences. 2013;2: 28-37. [ Links ]
24. Bellot-Arcís, C, Almerich-Silla, JM. Psychosocial impact of malocclusion in Spanish adolescents. The Korean Journal of Orthodontics. 20143;43:193-200. [ Links ]
25. Klages, U, Erbe, C, Sandru, SD, Brüllman, D, Wehrbein, H. Psychosocial impact of dental aesthetics in adolescence: validity and reliability of a questionnaire across age-groups. Quality of Life Research.2015;24: 379-90 . [ Links ]
26. Jawad, Z, Bates, C, Hodge, T. Who needs orthodontic treatment? Who gets it? And who wants it? British Dental Journal. 2015;218: 99-103. [ Links ]
27. Settineri, S, Rizzo, M, Liotta, M, Mento, C. The validation of the pychological impact of dental aesthetics questionnaire (PIDAQ). Health.2014;6: 2100-8 . [ Links ]
28. Bellot-Arcís, C, Montiel-Company, JM., Pinho, T, Almerich-Silla, JM. Relationship between perception of malocclusion and the psychological impact of dental aesthetics in university students. Journal of Clinical and Experimental Dentistry. 2015; 7: e18 (2015). [ Links ]
 Correspondence:
Correspondence:
DP Motloba
Head, Department of Community Dentistry
School of Oral Health Sciences
Sefako Makgatho Health Sciences University.
E-mail: pagollang.motlaba@smu.ac.za













