Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.71 no.4 Johannesburg Mai. 2016
CLINICAL COMMUNICATION
Vesna KaricI; Geoffrey MelmanII; Riaan MulderIII
IBDS(Bgd, EU), MSc(Dent)(Wits). Senior Lecturer, Division of Operative Dentistry, School of Oral Health Sciences, University of the Witwatersrand, Johannesburg
IIBDS(Wits), MSc(Dent)(Wits), Specialist in Paediatric Dentistry (UK). Department of Orthodontics and Paediatric Dentistry, School of Oral Health Sciences, University of the Witwatersrand, Johannesburg
IIIBChD (UWC), MSc(Dent)(UWC). Lecturer, Department of Orthodontics and Paediatric Dentistry. University of the Western Cape, Tygerberg, Cape Town
It was Albert Einstein who in 1917 defined the theory of the Stimulated Emission of Radiation, developing and expanding on the work of Niels Bohr, who in 1913 had formulated the Spontaneous Emission theory. Einstein described the electrons of molecules being excited by a source of energy, usually heat, and directed in a specific way.1 The excited electron releases a spontaneously emitted photon which interacts with a molecule of the active medium, causing those electrons to move to a less stable, higher energy state and producing further photons. This process exponentially increases the number of identical photons which are focused by mirrors at either end of the laser tube and emitted into the delivery system.2 The acronym "LASER" represents "light amplification by stimulated emission of radiation".
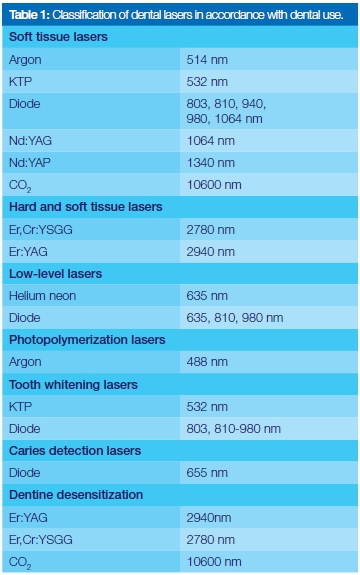
Theodore Maiman (1960) developed the first working laser.3 The active mediums contain a homogeneous population of atoms that characterize each type of laser, allowing photons to be produced and absorb energy of certain wavelengths. The active mediums can be a gas such as carbon dioxide (CO2), or solid crystal such as yttrium-aluminium garnet (YAG) or a neodymium-doped yttrium aluminium garnet (Nd) YAG. Diode lasers are solid state semi-conductors. In dentistry lasers can be classified according to their active mediums which determine the wavelengths of the laser and which in turn dictate the tissue interaction, intra-oral uses and the scope of practice (Table 1).4
A synopsis of lasers in use in Dentistry
The Carbon Dioxide Laser (CO2) provides rapid soft tissue removal and haemostasis with a very shallow depth of penetration. It provides a very dry operating field with reduced swelling of soft tissue. The main chromophore target for this wavelength (10,600nm) is water. The exposed tissue undergoes a rapid evaporation of both intracellular and extracellular fluids and the photo-destruction of the rest of the cell.
The Neodymium (Nd) Yttrium Aluminum Garnet Laser: YAG wavelength (1,064nm) is highly absorbed by haemoglobin and melanin. The energy emitted from this laser is predominantly diffused in the targeted tissues in the form of heat, making it a very effective surgical laser for cutting and coagulating dental soft tissues, with good haemostasis. In addition to its surgical applications, there has been research on using the Nd:YAG laser and various diode lasers for non-surgical sulcular debridement in periodontal disease control and the Laser Assisted New Attachment Procedure (LANAP).
Erbium Laser: There are two distinct wavelengths, namely the Er,Cr:YSGG lasers (2780nm) and Er:YAG lasers (2940nm). The erbium wavelengths have a high affinity for hydroxyapatite and the highest absorption of water of any laser wavelengths. Consequently, it is the laser of choice for treatment of dental hard tissues in operative dentistry. It has been shown that there is a 3°C rise in pulpal temperatures during cavity preparation on extracted teeth with the Er:YAG laser, well below the 5.5°C that is deemed safe to prevent an acute pulpitis.4 In addition to hard tissue procedures, an erbium laser can also be used for soft tissue ablation due to its high affinity for water.
Diode Laser: The diode laser is a solid state semiconductor that can be made of aluminum, gallium, arsenide and occasionally indium. All diode laser wavelengths (803 to 1,064nm) are absorbed primarily by tissue pigment (melanin) and haemoglobin. The emitted laser energy is scattered in the target tissues and later converted to heat. Conversely, the energy is poorly absorbed by the hydroxyapatite and by water present in the enamel. Specific procedures appropriate to their use include aesthetic gingival re-contouring, soft tissue crown lengthening, and removal of inflamed and hypertrophic tissue. The diode laser has become popular for use in frenectomies and for photostimulation of apthous / herpetic lesions.
Lasers offer a wide application in Dentistry with considerable benefits and advantages. However, there is a basic requirement that clinicians and associated staff ensure that laser use is carried out in a safe environment and with consent from the patient. Lasers can damage oral tissue, the skin, and eyes. Safety considerations are proportional to established and recognized risk. Safety glasses must be worn by the dental team and the patient at all times. The operator must have a thorough understanding of laser physics and of the device being used. Strict adherence to national and international regulations for dental lasers is essential.
ACRONYMS
KTP: potassium titanyl phosphate
Nd:YAG: neodinium-doped yttrium aluminium garnet
Nd:YAP: neodinium-doped yttrium aluminum perovskite
CO2: carbon dioxide
Er,Cr:YSGG: erbium-chromium-doped yttrium scandium gallium garnet
LANAP: Laser Assisted New Attachment Procedure
References
1. Einstein A. Zur Quantentheorie der Strahlung. Physikalische Zeitschrift. 1917; (18):121 -8. [ Links ]
2. Convissar R(ed). Lasers and light amplification in dentistry. Dent Clin N Am 2000;44(4). [ Links ]
3. Maiman TH. Stimulated optical radiation in ruby masers. Nature 1960;187:493-4 [ Links ]
4. Giovanni O, Margolis FS, Genovese MD. Paediatric Laser Dentistry: A User's Guide. 2011. Quintessence Publishing. 4350 Chandler Drive, Hanover Park, 60133, IL. ISBN: 978-0-86715-494-8. [ Links ]
5. Cozean C, Arcoria, CJ, Pelagalli J, Powell GL. Dentistry for the 21st century? Arch Oral Biol. 1997; 42(12):845-54. [ Links ]
6. Sweeney et al. Laser safety in Dentistry; A position paper, J Laser Dent 2009; 17(1):39-49. [ Links ]
 Correspondence:
Correspondence:
Vesna Karic
Division of Operative Dentistry
School of Oral Health Sciences, University of the Witwatersrand
Johannesburg
E-mail: Vesna.Karic@wits.ac.za













