Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.71 n.4 Johannesburg May. 2016
RESEARCH
Parental perspectives on self-care practices and dental sealants as preventive measures for dental caries
Brenton G NairI; Shenuka SinghII
IB Dental Therapy (UDW), M.MED (Dental Therapy) (UKZN). Masters graduate: Discipline of Dentistry, School of Health Sciences, University of KwaZulu-Natal
IIB. OH. (UDW), MSc [DENT], PhD (UWC), PG Dip Heal Res Ethics (Stell). Academic Leader (Head) - Discipline of Dentistry and Acting College Dean: Teaching and Learning - College of Health Sciences, University of KwaZulu-Natal
ABSTRACT
The oral health behaviour of children is increasingly seen to be driven and shaped by parental influences.
AIM AND OBJECTIVES: The study set out to explore parental understanding of dental caries, self-care practices, and dental sealants as preventive strategies for dental caries.
METHODS: This was an explorative and cross-sectional study. The participants were parents/care-givers (n=295) of grade one learners. Twelve schools were selected from the Chatsworth Circuit, KwaZulu-Natal, using a systematic sampling technique. Information was obtained through the use of a self-administered questionnaire and focus group discussions.
RESULTS: Seventy-four percent of respondents reported that unhealthy deciduous teeth can lead to problems when permanent teeth develop (p<0.001). Although the majority of respondents understood the role of diet and self-care practices, almost 80% of these respondents did not floss and 70% did not use a mouth rinse. Sixty-five percent were aware of dental sealants and these parents were twice as likely to be willing to have sealant placements performed on their children than those parents who were unaware of the procedure (OR 2.32, p<0.001).
CONCLUSION: Parental knowledge and awareness of oral health self-care practices does appear to translate into support for dental sealants as a preventive strategy for dental caries.
Keywords: parental knowledge and attitudes; oral health; dental sealants; dental caries; South Africa
INTRODUCTION
Dental caries is a preventable disease but remains poorly researched in developing countries, particularly sub-Saharan Africa.1-3 While not life-threatening, the impact of caries on the quality of life is profound, inflicting pain; impaired functional capacity and a negative influence on the child's growth rate and body weight.4 When the disease has an early onset with rampant clinical progression, dental caries becomes a serious public health problem, a challenge which is further compounded by the high cost of treatment.1,4 While the causes of dental caries are known and the disease can be prevented, its high prevalence amongst South African children suggests that the benefits of prevention are not reaching this population group.5,6
Eating and tooth-brushing behaviour are learned in early childhood and the home environment exerts substantial influence on the development of these behaviours.7,8 Maternal or caregivers' knowledge of nutrition, the impact of parental feeding practices, television viewing and peer pressure all play a role in influencing the child's eating behaviour.8 Several studies have examined the influence of parental knowledge, attitudes and perceptions (KAP) on oral health self-care practices in the family.9-11 Parental oral hygiene self-care practices such as tooth-brushing routines, knowledge of fluoride, healthy diet and perceptions of the importance of good oral health care, have been found to have an impact on the oral health behaviour of their children.9-11
LITERATURE REVIEW
Very few national surveys on dental caries rates have been conducted in South Africa. The National Children Oral Health Survey of 1999/2002 indicated that children living in urban areas have significantly higher rates of dental caries than do children in rural areas, and that oral health need varied widely from province to province.6 The survey also described the percentage of children in South Africa who required treatment for dental caries as ranging from 45%-60%, with the mean number of teeth needing care ranging between two to three per child.6 The greatest need was recorded in the Western Cape, (almost 80% in need), while the lowest need for dental caries care was recorded in Limpopo Province.6 In KwaZulu-Natal, the prevalence of dental caries in six-year-olds with primary dentition was recorded as 64.8%. Oral health unmet treatment need varied widely with the four to five and the six-year old age groups requiring more emergency relief of pain and conservative care in comparison with the older groups.6
Dental caries preventive strategies include educational and oral health awareness programmes; additional fluoride uptake and sealant placement programmes.7,12-15 A critical review of current dental public health preventive strategies at national, provincial and local levels in South Africa reveals that oral health promotion programmes are poorly implemented, inconsistent, fragmented and not evaluated at design, implementation, and post-implementation levels.12
Dental sealants
Epidemiological studies have found strong evidence of the effectiveness of dental sealants on sound posterior teeth in children and adolescents.1,16-18 The occurrence of dental caries in the pits and fissures of posterior teeth may be reduced by 60% in the period of two to five years after placement with a reduction of 78% in the first year and of 59% over four years or more.1,17 A study by Weintraub et al. (2001) assessed the dental experience of 15438 children over a seven-year period and concluded that dental sealant placement was associated with savings in expenditure.19
These studies generally agree that dental sealants should be part of an overall prevention strategy which should include caries risk assessment. The delivery platforms could include clinics, mobile units or school settings.12 One limitation of this caries preventive strategy is the need for skilled oral health personnel, hence increasing the potential cost of the programme.16,17,20 A second limitation is that the application and the successful retention of dental sealants are technique-sensitive, dependent on a number of factors including clinical competency and the type of material used.16,17,20
This study set out to explore parental understanding of dental caries, oral health self-care practices, and the use of dental sealants as caries-preventive strategies for children residing in the Chatsworth Circuit of the uMlazi District, KwaZulu-Natal. This province accounts for approximately 7.6% of South Africa's land surface with a population of 10 449 300.21 The study null-hypothesis was that parents of Grade 1 learners in the identified region will not have a basic understanding of dental caries, of oral health self-care practices, and of the role of dental sealants in caries prevention.
METHODS
The study design was explorative and cross-sectional using a combination of probability and non-probability sampling, and quantitative and qualitative data. From a total sample of 50 schools (representing 5832 Grade 1 learners) in the district, twelve were selected using a systematic sampling technique (with a confidence level of 95%). The names of schools were placed into an alphabetically ordered list. The total sample of 50 was divided by the desired sample number, 12, leading to the outcome of 4,2. Hence every fourth school was selected from the ordered list. If a selected school declined participation in the study, a substitute school was selected using the same sampling technique.
Information was obtained in two phases. Phase One made use of a self-administered questionnaire that sought information on demographic data, oral health behaviour and knowledge patterns, income and education status, and knowledge of oral health prevention practices. Questionnaires were sent out to about 800 parents via the learners. The inclusion criteria were that the potential participant should be 18 years or older, be a biological parent, care-giver, grand-parent or guardian and be residing in the geographical region of the uMlazi school district. Three hundred and thirteen (313) questionnaires were returned, representing a response rate of 40%. From these were excluded 18 returned questionnaires that had incomplete responses. The final study sample therefore had 295 participants (n=295).
The questionnaire was a modified version of the Child Oral-Health-Related Quality of Life (COHQoL) questionnaire.22 The scales for measurement comprised of the Child Perceptions Questionnaire (CPQ); the Parental-Caregiver Perceptions Questionnaire (P-CPQ) and the Family Impact Scale (FIS). The reliability, validity and responsiveness in longitudinal research of the P-CPQ component and the FIS have been confirmed by Thomson et al. (2013) and by Kramer et al. (2013).22,23 The questionnaire was organised into four sections: Section A focused on parental biographical data such as age, gender and education, income, number of people in each household and medical insurance ownership. Section B included information on knowledge of dental caries. Sections C, D and E had questions related to perceptions and attitudes of dental caries and preventive care, for example, "Problems with baby/milk teeth could affect adult teeth" and "Have you heard about dental sealants?" The questionnaire comprised of both open ended and closed ended responses. The questionnaire was pre-tested in a pilot study conducted among ten parents whose children attended a primary school that was not on the identified sample list.
Data for Phase Two was obtained through focus group semi-structured interviews with parents who had completed the questionnaire, at five conveniently selected schools with 10 participants in each group. The purpose of the focus group discussion was to explore parental understanding of dental sealants as a component of preventive care. The focus group discussion consisted of open-ended statements and questions, and a visual aid (a photograph of a dental sealant being placed onto a tooth) to elicit the understanding of participants of dental sealants. The focus group discussion was audio-recorded. Consent was obtained for each phase of data collection. Ethical approval was obtained from the Humanities and Social Sciences Research Ethics Committee at the University of KwaZulu-Natal (Reference: HSS/0327/013M) and gatekeeper permission was obtained from the Department of Education and the Department of Health in the eThekwini District, KwaZulu-Natal.
All quantitative responses were collated and entered into a computer database using Microsoft Excel® and examined statistically using the statistical software package for social sciences IBM SPSS Statistics® version 21. Statistics were generated for biographic and demographic characteristics, and for parental knowledge, attitudes and perceptions of preventive strategies against early childhood caries. The responses to the open-ended questions were scrutinised for key concepts and themes and then thematically grouped after identifying a common link. Statements expressing similar sentiments were grouped into themes that represented the main messages conveyed by the data and then analysed using the software package NVivo® 10. Univariate descriptive statistics such as frequency and mean distribution were conducted for all variables. The Pearson chi-squared test was conducted to assess possible relationship between the independent variables (income, education and age) and the dependent variables (oral health knowledge, attitudes and behaviours). A level of p<0.05 was established as being significant. The data on' the educational levels of participants were further categorised into higher (high school level and tertiary education) and low education (no formal education and primary school education). Binary logistic regression analysis and Odds Ratios (ORs) with 95% confidence levels (CI) were also calculated.
Data collected from the focus group discussions were analysed using the open coding method of thematic analysis and the software package NVivo® 10. Each of the five focus group transcripts was scrutinised for key concepts and themes. To minimise bias all interviews were additionally scrutinised by another independent researcher and consensus was reached in the allocation of codes and themes. Member verification was conducted on the transcripts from the focus group discussions. This ensured credibility in the data collected.
RESULTS
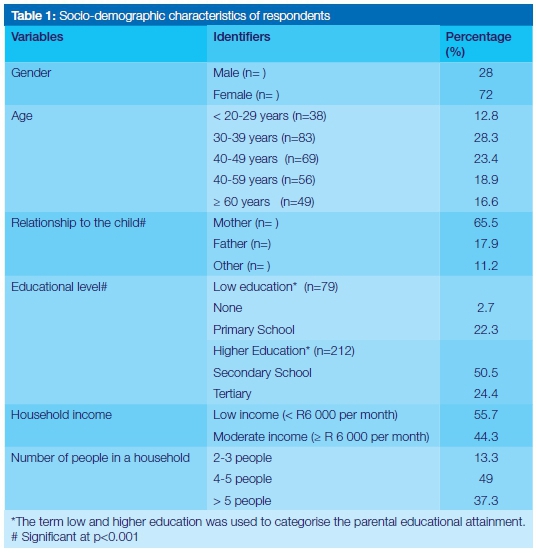
The study sample comprised of 295 participants, nearly three quarters of whom were female (72%). Half of the study population was in the 30-49 years age group (n=152, 51.7%). More than two-thirds of the participants (75%) had at least a high school or tertiary education (Table 1). Despite the majority of the participants being of higher educational level (75%), the results showed that 55.7% of the study population earned less than R6000 per month and that 42.7% received their monthly income in the form of social grants, donations or pensions. Although the results revealed that majority of the primary caregivers were female, no significant statistical association could be established between gender and any of the variables such as oral health practices or visits to the dentist.
Nearly three-quarters of the participants (73.6%) reported that unhealthy deciduous teeth could lead to problems when permanent teeth develop (p<0.001). Almost 42% of participants reported that their children had missed school because of dental caries. Additionally 25% of adults had missed work because their children had 'toothache'. Respondents indicated that they took their children to public oral health care facilities (49.6%) or to private dental practitioners (39.6%) whilst smaller numbers (10.8%) reported using home-care or traditional care when dental care was required.
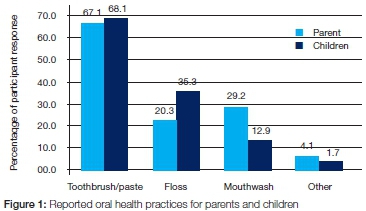
Although the majority of respondents understood the role of diet and self-care practices such as tooth-brushing, almost 80% of these respondents did not themselves floss and 70% did not use a mouthwash (Figure 1). Similar scores were reported by respondents who answered for their children's oral health care practices. Most parents (67.1%) reported that they and their children (68.1%) used toothbrushes and toothpaste. Only 20.3% of parents used dental floss themselves, whilst 35% of parents reported that their children flossed.
In the focus group interview, a participant from group "D" highlighted the difficulties experienced in getting children to brush their teeth, stating that "they brush but I try to make it fun and it works for me but when I am not around it doesn't work out very well." Another participant from Group "E" proposed that whilst tooth brushing was important for oral hygiene, the correct brushing technique was more important than the brand of toothbrush or tooth paste. A participant from focus group "B" stated that whilst they were able to control their children's diet and oral hygiene practices at home they were unable to exert such control "at school or when children visit in-laws, at school, Diwali or at Christmas time."
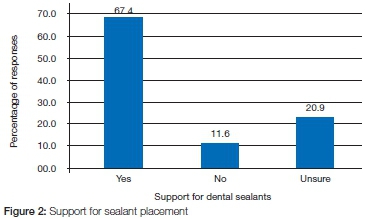
The study results also indicated that the majority of respondents (65%) were aware of dental sealants. However only 67% of participants were willing to have sealant placements performed on their children (Figure 2). Thirty-two percent (32%) of respondents were hesitant or unwilling to have this procedure done. Parents who were aware of dental sealants were twice as likely to be willing to have sealant placements performed on their children than parents who were unaware of the process (OR 2.32, p<0.001). Additionally a participant in focus group "D" stated that she was concerned about the "side effects of dental sealants".
DISCUSSION
The results of this study reveal gaps in parental knowledge, attitudes and perceptions about dental caries, oral hygiene practices, diet and nutrition, and dental sealants. Only 67.1% of respondents indicated their use of toothbrush and toothpaste for self-care practices. The respondents also recorded that only 68.1% of children brushed their teeth. The majority of respondents did not floss (79.7%) or use a mouthwash (70.8%). According to de Castilho et al (2013), the key elements shown to impact on oral health behaviour of children include parental oral health attitudes, general knowledge and oral health status.24 These authors further add that children's oral health behaviours are more closely related to parental oral health behaviours,24 an opinion similar to the findings of this study. Although knowledge and attitudes towards oral health self-care practices are important considerations, examples set by parents in their oral health behaviours are seen to have a greater influence on those of their children.
Saldūnaitė et al (2014) pointed out that parental education and socio-economic status appear to influence the implementation of dental caries prevention in children.11 Higher parental education is associated with more favourable oral health outcomes in children.25 The literature further indicates that cultural norms and social factors such as values, beliefs and customs are also seen to influence oral health.26
It is therefore imperative that oral health promotion programmes and interventions include mother and child/family involvement in addressing early childhood caries.12, 27 More research and advocacy needs to be conducted to identify strategies to improve parental involvement in oral health promotion decision making, specifically in the area of children's oral health care. The contextual influences (such as income, living conditions, nutritional intake and access to oral health care services) on a family's capacity to maintain optimal oral health status must also be considered and addressed when designing and implementing these programmes and interventions.
Two-thirds of the study participants were able to identify sealants as a mechanism to help prevent dental caries but 32% of respondents did not support this procedure. Although this issue was further explored in the focus group discussions, participants provided weak reasons for not supporting dental sealants, such as concerns about the 'side effects of fissure sealants'. Bonetti et al (2010) reported in their study that the main problem may be a lack of understanding of the mechanism by which the sealant works.28 The themes arising from qualitative analysis suggested a poor understanding of common oral diseases and oral health priorities, coupled with the perception that low oral health status could be inherited. The study results imply an acceptance that oral health status is very much beyond the individual's control and that oral health intervention should only occur when the condition becomes symptomatic. Conversely, past dental experiences, limited access to care, or impact of time away from work could also contribute to inconsistent perceptions of dental sealant uptake.
Potential bias could also have resulted in parents over-reporting their knowledge of dental sealants. Contrary to the findings in this study, the literature does however suggest that knowledge of dental sealants does not necessarily translate into a behavioural change.29 Given that 32% of respondents did not support dental sealants, more research needs to be conducted to unravel the reasons for parents not wanting to have sealant placements done on their children despite their having a knowledge of its proven benefits. Bonetti et al (2010) suggest that psychological theories such as the Theory of Planned Behaviour (TPB), the Social Cognitive Theory (SCT) and the Operant Learning Theory (OLT) could be utilised in efforts to ensure that parental knowledge, attitudes and perceptions toward dental sealants and preventive care, are increased.28 On the other hand, parents could have positive attitudes towards preventive care, including dental sealants but this is of little value if there are obstacles to accessing these inventions. Further research is also required to explore the availability and support for oral health promotion activities, specifically from a public oral health service delivery perspective.
The World Health Organisation advocates that comprehensive strategies to prevent caries in children cannot be conducted in isolation but should be part of a collaborative health promotion effort between the following role-players: health care professionals, educators and health care providers; caregivers; and the child.30 A framework for any oral health promotion programme should include the following five approaches: intervention, behaviour change, education, client-centred approach and societal change.9,30 Thus an oral health promotion programme aimed at reducing the rate of dental caries and improving oral health outcomes in children should consider the multifactorial influences on this process and ensure strategic engagement with the relevant stakeholders at all levels of programme planning and implementation.
A limitation of this study is that the research findings cannot be generalised. Despite this, the results provide insight into parental practice, knowledge and perceptions towards oral health care for their children/guardians. The study provides useful data that could be used to re-orientate planning towards improved oral health promotion, especially among identified high-risk groups from lower-socio-economic groups. These data could also be integrated into programmes aimed at addressing non-communicable diseases that affect South Africa and other countries of similar economic and social development.
CONCLUSION
The study concludes that parental knowledge and awareness of oral health self-care practices does appear to translate into support for dental sealants as a preventive strategy for dental caries. The alternate hypothesis for this study is thus supported. More research needs to be conducted to further investigate strategies to improve parental involvement in oral health promotion decision-making, specifically in the area of children's oral health care.
Acknowledgement
This paper formed part of a dissertation submitted for the fulfilment of a Master's degree (M.Med).
ACRONYMS
COHQoL: Child Oral-Health-Related Quality of Life
CPQ: Child Perceptions Questionnaire
FIS: Family Impact Scale
KAP: knowledge, attitudes and perceptions
P-CPQ: Parental-Caregiver Perceptions Questionnaire
References
1.Al Agili DE, Niazy HA, Pass MA. Prevalence and socioeconomic determinants of dental sealant use among schoolchildren in Saudi Arabia. East Mediterr Heal J. 2012;18(12):1209-16. [ Links ]
2.Postma T, van Wyk P, Ayo-Yusuf O. Empirical support for a fissure sealant placement timeframe protocol for Black South Africans. South African Dent J. 2008;63:344-6. [ Links ]
3.Kiwanuka SN, Astrøm AN, Trovik TA. Dental caries experience and its relationship to social and behavioural factors among 3-5-year-old children in Uganda. Int J Paediatr Dent. 2004;14(5):336-46. [ Links ]
4.Zafar S, Yasin-Harnekar SY, Siddiqi A. Early childhood caries: aetiology, clinical considerations, consequences and management. Int Dent. 2009;11:24-36. [ Links ]
5.Postma TC, Ayo-Yusuf OA, van Wyk PJ. Socio-demographic correlates of early childhood caries prevalence and severity in a developing country - South Africa. Int Dent J. 2008;58:344-6. [ Links ]
6.Department of Health. Report: National Children's Oral Health Survey. South Africa, 2003:1-18. [ Links ]
7.Nakhjavini YB, Forutan S, Nakhjavani FB. Mothers' knowledge about fluoride therapy and fissure sealants. J Oral Heal Oral Epidemiol. 2013;2(1):1-5. [ Links ]
8.Campbell K, Crawford DA, Hesketh KD. Australian parents' views on their 5-6-year-old children's food choices. Health Promot Int. 2007;22(1):11-8. [ Links ]
9. Pine CM, Adair PM, Nicoll AD, Burnside G, Petersen PE, Beighton D, et al. International comparisons of health inequalities in childhood dental caries. Community Dent Health. 2004;21:121-30. [ Links ]
10. Blinkhorn A, Wainwright-Stringer YM, Holloway PJ. Dental health knowledge and attitudes of regularly attending mothers of high-risk, pre-school children. Int Dent J. 2001;51:435-8. [ Links ]
11 .Saldūnaitė K , Bendoraitienė EA, Slabšinskienė E, Vasiliauskienė I, Andruškevičienė V, Zūbienė J. The role of parental education and socioeconomic status in dental caries prevention among Lithuanian children, Medicina. 2014;50(3):156-61. [ Links ]
12. Singh S. Dental caries rates in South Africa: implications for oral health planning. South African J Epidemiol Infect. 2011;26(4):259-61. [ Links ]
13. Kitchens D. The economics of pit and fissure sealants in preventive dentistry - A review. J Contemp Dent Pract. 2005;6(3):95-103. [ Links ]
14. Featherstone J. The continuum of dental caries - evidence for a dynamic disease process. J Dent Restor. 2004;83:C39-42. [ Links ]
15. Marinho V, Higgins J, Logan S, Sheiham A. Fluoride mouth rinses for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003;3(CD002284). [ Links ]
16. Hiiri A, Ahovuo-Saloranta A, Nordblad A, Mäkelä M. Pit and fissure sealants versus fluoride varnishes for preventing dental decay in children and adolescents. Cochrane Database Syst Rev. 2010;17(3):CD003067. doi:10.1002/14651858. [ Links ]
17. Gooch BF, Griffin SO, Gray SK, Kohn WG, Rozier RG, Siegal M, et al. Preventing dental caries through school-based sealant programs: Updated Recommendations and Reviews of Evidence. J Am Dent Assoc. 2009;140(11):1356-65. [ Links ]
18. Yengopal V, Harnekar SY, Patel N, Siegfried N. Dental fillings for the treatment of caries in the primary dentition. Cochrane Database Syst Rev. 2009;(2). CD004483. doi:10.1002/14651858 [ Links ]
19. Weintraub J, Stearns SC, Rozier RG, Huang CC. Treatment outcomes and costs of dental sealants among children enrolled in Medicaid. Am J Public Health. 2001;91(11):1877-81. [ Links ]
20. Yengopal V, Mickenautsch S, Bezerra AC, Leal SC. Caries-preventive effect of glass ionomer and resin-based fissure sealants on permanent teeth -a meta-analysis. J Oral Sci. 2009;51:373-82. [ Links ]
21. Statistics South Africa. Census 2011. Pretoria; 2012. Available from: http://www.statssa.gov.za/publications/p03014/p030142011.pdf [ Links ]
22. Thomson WM, Foster Page LA, Gaynor WN, Malden PE. Short-form versions of the Parental-Caregivers Perceptions Questionnaire and the Family Impact Scale. Community Dent Oral Epidemiol. 2013;41(5):441-50 [ Links ]
23. Kramer PF, Feldens CA, Ferreira SH, Bervian J, Rodrigues PH, Peres MA. Exploring the impact of oral diseases and disorders on quality of life of preschool children. Community Dent Oral Epidemiol. 2013;41(4):327-35. [ Links ]
24. De Castilho ARF, Mialhe FL, Barbosa T, Puppin-Rontani RM. Influence of family environment on children's oral health: a systematic review. J Pediatr (Rio J). 2013;89:116-23. [ Links ]
25. Saied-Moallemi Z, Virtanen JI, Ghofranipour F, Murtomaa H. Influence of mother's oral health knowledge and attitudes on their children's dental health. Eur Arch Paediatr Dent. 2008;9:79-83. [ Links ]
26. Hilton IV, Stephen S, Barker JC, Weintraub JA. Cultural factors and children's oral health care: a qualitative study of carers of young children. Community Dent Oral Epidemiol. 2007;35:429-38. [ Links ]
27. Agostini BA, Machry R.V, Teixeira CR, Piovesan C, Oliveira MDM, Bresolin CR, Ardenghi TM. Self-perceived oral health influences toothbrushing in preschool children. Brazilian Dental Journal. 2014; 25(3), pp.248-52. [ Links ]
28. Bonetti D, Johnston M, Clarkson JE, Grimshaw J, Pitts NB., Eccles M, et al. Applying psychological theories to evidence-based clinical practice: identifying factors predictive of placing preventive fissure sealants. Implement Sci. 2010;5(25):1-15. [ Links ]
29. Locker D. Deprivation and Oral Health: A Review. Community Dent Oral Epidemiol. 2000;28:161-9. [ Links ]
30. Petersen P. World Health Organization, The World Oral Health Report 2003. World Health Organ. 2003; Available from: http://www.who.int/oral_health/media/en/orh_report03_en.pdf [ Links ]
 Correspondence:
Correspondence:
Shenuka Singh
Discipline of Dentistry, School of Health Sciences, University of KwaZulu-Natal
Private Bag X54001, Durban, South Africa 4000
Tel: 031 242 8591
Fax: 031 260 8069
E-mail: singhshen@ukzn.ac.za













