Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.71 n.3 Johannesburg Apr. 2016
CASE BOOK
Oral pathology case book: Metastatic colorectal carcinoma to the mandible
BK BunnI; H KloppersII; WFP van HeerdenIII
IBDS, MDent, FC Path(SA)Oral Path. Department of Oral Pathology and Oral Biology, School of Dentistry, Faculty of Health Sciences, University of Pretoria
IIBChD, DipOdont, MChD (MFOS). Department of Maxillofacial and Oral Surgery, School of Dentistry, Faculty of Health Sciences, University of Pretoria
IIIBChD, MChD, FC Path (SA) Oral Path, PhD, DSc. Department of Oral Pathology and Oral Biology, School of Dentistry, Faculty of Health Sciences, University of Pretoria
CASE REPORT
A 75-year old male patient presented to the Department of Maxillofacial and Oral Surgery complaining of a four-month history of a painless, ulcerative lesion which involved the posterior mandibular alveolar ridge in the region of tooth 38 with extension into the base of tongue. The patient reported that the lesion initially presented as a "pimple". A dome-shaped area of mucosal swelling was clinically noted which subsequently ulcerated and had since failed to heal. The patient had sought treatment at three different hospitals before being referred to our institution.
Intra-oral examination confirmed the presence of an ulcer in the third quadrant. Tooth 37 and tooth 38 were missing while teeth 33, 34 and 35 were mobile. Radiological examination revealed two areas of bone destruction within the left mandible. The posterior area of bone destruction was located distal to tooth 36 extending posteriorly up to the anterior margin of the ramus while the anterior osteolytic defect extended from the distal aspect of tooth 32 to the mesial root of tooth 36. Numerous teeth showed associated periapical radiolucencies (Figure 1). In addition, the patient had suboptimal oral hygiene and appeared to be in a poor general medical state although he did not complain of any other signs or symptoms and was not on any chronic medication at the time of presentation. An incisional biopsy from the ulcerated intra-oral lesion was submitted for histology.

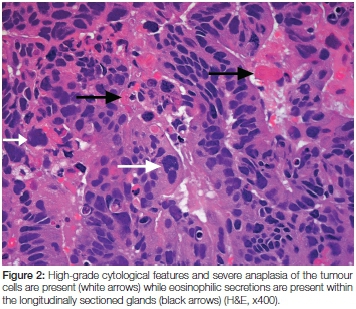
Histological examination of the tissue sections confirmed the presence of a high-grade malignant adenocarcinoma, the morphology of which was highly suggestive of a metastatic neoplasm. The malignant infiltrate comprised a well-formed glandular component with several glands cut in cross section to reveal interspersed lumina containing eosinophilic secretions. The tumour cells were markedly pleomorphic with conspicuous nuclear hyperchromasia, increased nuclear to cytoplasmic ratios and brisk mitotic activity (Figure 2). Central areas of comedo-type necrosis were observed. A panel of immunohistochemical stains was performed on sections of tissue in the presence of adequate positive and negative controls. Strong, diffuse immunoreactivity was noted for cytokeratin 20 (CK20) whilst cytokeratin 7 (CK7) immunostaining was negative. Furthermore, immunopositivity for carcino-embryonic antigen (CEA) was diffuse in its distribution (Figure 3). The histomorphological features and immunoprofile in this case were most suggestive of an adenocarcinoma of colorectal origin. Further clinicopathological correlation, systemic investigation and work up were therefore advised.

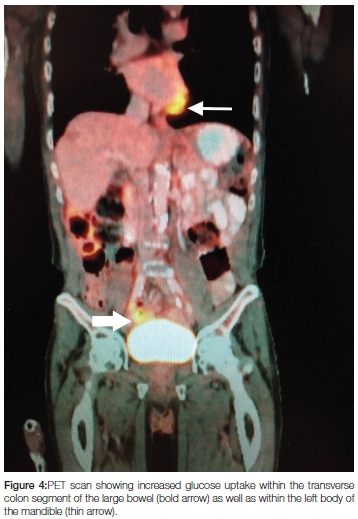
A full body examination together with positron emission topographic (PET) scanning was performed. Glucose uptake highlighted "hotspots" of activity within the transverse colon and left mandible which served to confirm the histological assertion of a primary colorectal adenocarcinoma (Figure 4). The patient was referred for palliative therapy.
DISCUSSION
One of the hallmarks of malignancy is the ability to invade and metastasise to both loco-regional and distant sites. Metastatic tumour spread to the orofacial region is rare and accounts for only 1 to 4% of all oral malignancies and is typically diagnosed in the 5th to 7th decades of life.1-7 Secondary malignancy at this site may solely involve bone or soft tissue or in some instances both.7 Metastatic orofacial malignancies are predominantly located within bone in up to 90% of all cases. The mandible is the preferred site of distant metastatic tumour spread within the orofacial region, being involved in almost 85% of cases and far more frequently than the maxilla or soft tissue.1,3,4 The posterior regions of the mandible are followed by the mandibular angle, retromolar trigone area and condyle in descending order of favoured metastatic sites.1 Isolated soft tissue involvement is less usual with cases being largely limited to the gingiva and tongue.1,3
The relative scarcity of mandibular metastases in general, is attributed to the increased bone density at this site which is accompanied by poor vascularity and an age-related loss of active haematopoietic tissue.3,5 Jaw bone involvement is almost always a late stage event characterised by multiple co-existent metastatic deposits, representing widespread disseminated disease.4 Furthermore, in approximately 67% of cases, jaw bone deposits of secondary tumour are concurrently identified at the time of primary tumour diagnosis.4 The clinical and histological diagnosis of distant metastatic disease in the absence of any known primary tumour remains challenging but should always be borne in mind for unusual soft tissue lesions and destructive bone disease at this site.3
The most common primary tumour sites in male patients with secondary orofacial tumour involvement include the lungs, adrenal glands, kidneys and bone whilst in female patients, primary tumours are usually located in the breast, adrenal glands, female genito-urinary tract and colorectum.1,3
Further confounding the accurate diagnosis of jaw metastases from distant sites is the highly varied clinical presentation of secondary disease. Metastatic tumour deposits mimic a wide range of benign, reactive and malignant disease processes. Isolated soft tissue deposits commonly involve the attached gingiva in the anterior maxilla and mandible but may also be identified within the tongue, floor of mouth, palate and buccal mucosa. They tend to present as submucosal masses which ulcerate over time.2 The clinical differential diagnosis for a soft tissue swelling of this nature would include a pyogenic granuloma, vascular malformation, peripheral giant cell granuloma and fibrous epulis. Metastatic lesions are difficult to separate from reactive benign soft tissue proliferations on the basis of clinical presentation alone.3,7,8 Features supporting the diagnosis of a malignant soft tissue neoplasm include rapid growth, excessive bleeding, extensive surface ulceration and tissue necrosis. Soft tissue lesions may infiltrate adjacent bone to result in osteolytic destruction.2,7
Tooth mobility, rapid growth, painful swelling, bleeding and paraesthesia should be clinically worrying for symptoms of malignant bone involvement.2 Bone metastases cause osteolytic defects associated with marked tenderness which may be further complicated by trismus, dysphagia and even pathological fracture.2,4 Radiological examination of metastatic tumours within bone shows irregular, ill-defined destructive radiolucent lesions which may be mistaken for infected odontogenic cysts, advanced periodontal bone loss, osteomyelitis or a primary bone or odontogenic malignancy.2 Very occasionally, tumour cells stimulate osteoblastic bone deposition resulting in a mixed radio-opaque / radiolucent radiological appearance.3
Bone involvement may be accompanied by the rapid onset of paraesthesia along the distribution of the mental branch of the inferior alveolar nerve associated with tingling, numbness and a burning sensation on the skin of the chin and lower lip.1,3 This rather peculiar neurological manifestation is termed "numb chin syndrome" (NCS) and is a fairly consistent indicator of primary or metastatic mandibular malignancy.1,2 NCS occurs due to direct tumour infiltration of nerve or as a result of perineural tumour spread. Mental nerve neuropathy consequently strongly suggests the presence of malignancy.3,4 The presence of NCS in a patient with no clinical evidence of pathology is often the only sign of a metastatic neoplasm.4
Colorectal carcinoma represents a disease of lifestyle associated with a diet high in fat and protein. Although previously considered a neoplasm of "Western Society", its incidence has increased dramatically in other geographic regions. Metastatic colorectal carcinoma is most often reported in the liver, lungs, adrenal glands and kidneys followed lastly by bone deposits. The jaw is an unlikely site for metastasis of this tumour and the clinical presence of lesions is customarily regarded as incurable, disseminated disease.1 Patient survival following the diagnosis of jaw metastases is predicted to be in the order of several months to a couple of years at best. Most patients will succumb to widespread organ involvement within a year of diagnosis.1,4,5,7
The CK7 and CK20 immuno-profiling of tumour masses allows for initial categorisation based on site of origin. Colorectal carcinoma consistently displays negativity for CK7 whilst showing strong positive immunoreactivity for CK20. These two simple immune-histochemical stains are exceptionally useful for excluding and including multiple sites of primary tumour origin.3 Additional site specific tissue markers and novel molecular markers are useful confirmatory adjuncts for the determination of the tissue of origin.4
Owing to the advanced nature of disease when jaw bone metastases are clinically evident, palliative therapy is the usual therapeutic option. This typically includes chemo-radiation and very occasionally surgery with no curative intent, at both primary and metastatic tumour sites. Palliative therapy is primarily aimed at reducing symptoms of pain and discomfort while facilitating normal function and improving the overall quality of the patient's life.3-5
CONCLUSION
Metastatic malignancy to the jaws signifies advanced, disseminated, incurable terminal disease. Awareness of the clinical heterogeneity as well as the fact that metastatic tumour deposits may be the first sign of occult primary malignancy emphasises the significance of early recognition and diagnosis. Jaw metastases frequently present as loosening of teeth prompting patients to seek dental treatment first and foremost. Clinicians therefore need to be cognizant of metastatic jaw bone lesions despite their scarcity. Rapidly growing destructive necrotic bone and soft tissue lesions in a geriatric age group with no known underlying cause of disease, as well as in patients who have previously been diagnosed with malignancy, demands expeditious diagnostic and therapeutic intervention. In patients with a previously diagnosed malignancy or in those who are undergoing oncological therapy, such a clinical presentation may be the first indication of tumour recurrence or progression. The earlier metastatic malignancy is recognised, the sooner palliation may be initiated, thus improving the quality of life for the patient.
This case is intended to highlight a rare orofacial manifestation of an underlying distant primary visceral neoplasm in order to increase the clinical index of suspicion for possible occult primary malignancy. It also demonstrates the absolute necessity of acquiring a thorough medical history from each and every patient whilst having adequate knowledge of systemic malignancies.
Declaration: No conflict of interest declared.
ACRONYMS
CBCT: cone beam computerised tomographic scan
CEA: carcino-embryonic antigen
CK7: cytokeratin 7
CK20: cytokeratin 20
NCS: numb chin syndrome
PET: positron emission topographic
References
1. Amin A, Jha M, Reddy A. Lower lip numbness in a patient with colorectal cancer. BMJ Case Rep 2011; 2011. Doi:10.1136/bcr.01.2011.3682. [ Links ]
2. Lim SY, Kim SA, Ahn SG, et al. Metastatic tumours to the jaws and oral soft tissues: a retrospective analysis of 41 Korean patients. Int J Oral Maxillofac Surg 2006; 35: 412-5. [ Links ]
3. Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, Berger R. Metastatic tumours to the oral cavity - pathogenesis and analysis of 673 cases. Oral Oncol 2008; 44: 743-52. [ Links ]
4. Aksoy S, Orhan K, Kursun S, Kolsuz ME, Celikten B. Metastasis of prostate carcinoma in the mandible manifesting as numb chin syndrome. World J Surg Oncol 2014; 12: 401. [ Links ]
5. Lavanya C, Ranganathan K, Veerabahu M. Mandibular metastasis of thyroid carcinoma: a case report. J Clin Diagn Res 2014; 8: ZD15-6. [ Links ]
6. Misra SR, Shankar YU, Rastogi V, Maragathavalli G. Metastatic hepatocellular carcinoma in the maxilla and mandible, an extremely rare presentation. Contemp Clin Dent 2015; 6: S117-21. [ Links ]
7. Murillo J, Bagan JV, Hens E, Diaz JM, Leopoldo M. Tumors metastasizing to the oral cavity: a study of 16 cases. J Oral Maxillofac Surg 2013; 71: 1545-51. [ Links ]
8. Ngwenya SP, Bunn BK. Clinical pathologic conference case 1: Lesion presenting as a hemorrhagic mass of the alveolar ridge. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116: e59-63. [ Links ]
 Correspondence:
Correspondence:
Willie Fp van heerden
Department of Oral Pathology and Oral Biology, University of Pretoria
Pretoria, South Africa.
Tel: +27 12 319 2320, Fax: +27 12 321 2225
E-mail: willie.vanheerden@up.ac.za













