Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.71 n.3 Johannesburg Apr. 2016
CASE BOOK
Oral medicine case book 73: HIV associated oral ulcerations differential diagnosis
Τ KungoaneI; JC MarnewickII; WFP van HeerdenIII
IB Dent Ther, BDS, MSc Dent (Oral Path), FC Path (SA) Oral Path MDENT (Oral Path). Department of Oral Pathology and Oral Biology, School of Dentistry, Faculty of Health Sciences, University of Pretoria
IIBChD, MDent. Department of Periodontics and Oral Medicine, School of Dentistry, Faculty of Health Sciences, University of Pretoria
IIIBChD, MChD, FC Path (SA) Oral Path, PhD, DSc. Department of Oral Pathology and Oral Biology, School of Dentistry, Faculty of Health Sciences, University of Pretoria
CASE REPORT
Clinical Presentation
A 36 year old female suffering from multiple oral ulcers was referred to the Department of Periodontics and Oral Medicine clinic at the University of Pretoria in February 2016. The ulcers had been present for a month, were first seen as "small sores" that had subsequently increased in size. On examination, multiple, relatively painful, large (>1cm) ulcers were seen on the palate, labial mucosa, tongue and gingiva (Figure 1). She also had gingivitis and a plunging ranula of the submandibular gland and reported recent weight loss. The patient had been diagnosed with retroviral disease in 2010; her latest CD4 count was 49 with a viral load of 111 797 copies. Her haemoglobin (Hb) was 11. 7g/dL and the estimated glomerular filtration rate (eGFR) >60mL/min. She had defaulted antiretroviral treatment (ARV) for a year and was reinstated on treatment, on ARVs regimen 2 comprising of Lamzid and Alluvia in January 2016. Empiric Dapsone treatment had been instituted for the ulcers.
Management and diagnosis
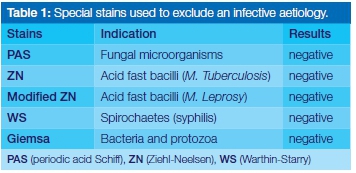
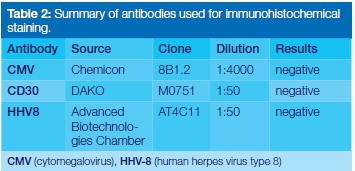
An incision biopsy was taken under local anaesthesia from the lower lip ulcer. A mucosa covered fragment measuring 8x4x4mm was received. The biopsy specimen was fixed in 10% neutral buffered formalin, processed and embedded in paraffin wax. The histological examination showed an ulcer with a necrotic floor. At the edge of the ulcer was an inflamed non-keratinizing squamous epithelium. The underlying lamina propria contained an acute-on-chronic inflammatory cell infiltrate consisting of histiocytes, plasma cells, lymphocytes, neutrophils, mast cell and occasional eosinophils. Scattered within the inflammation were large immunoblast-like cells with large nuclei, prominent nucleoli and ample cytoplasm. Viral cytopathic effects were not seen. Following routine histology examination, special stains were ordered to exclude an infectious aetiology (Table 1). Immunohistochemical stains and in-situ hybridization for EBV-encoded RNAs (EBER) were done to exclude viral and neoplastic infiltrates. The antibodies used, the source, clone and dilution together with results are summarised in Table 2. The final diagnosis was that of HIV- associated oral major aphthous ulceration. The patient was subsequently given chlorhexidine gluconate mouthwash and metronidazole. The patient was seen a month post-biopsy for follow-up with some resolution of some but not all lesions (Figure 2). At two months follow-up all lesions were healed.
DISCUSSION
Oral ulceration may be due to a number of factors including trauma, infection, immune mediated disorders, systemic disease and neoplasia. In patients with HIV the most likely causes are infections and neoplasia, both linked to a decrease in immune surveillance. Infections are prevalent in HIV patients therefore need to be considered in the possible pathogenesis of ulcers. Major oral aphthous ulcers in HIV are associated with a low CD4 count and increased inversion of the CD4+/ CD8+ ratio.1,2 The current patient had a low CD4 count (CD4 = 49).
Oral ulceration in HIV have been traditionally divided as ulcerations, not otherwise specified (NOS) (group 2) and recurrent aphthous stomatitis (group 3).3 The clinical significance of this delineation is arbitrary. Aphthous ulcers in HIV are similar to those occurring in seronegative patients, presenting as minor (less than 5mm diameter), major (>10mm) and herpetiform (multiple ulcers of 1-3mm). The diagnostic criteria of major aphthous ulcers in HIV as set out by Phelan et al4includes the following: large painful ulcers >1cm present for over >10 days, a negative viral culture and no infectious aetiology; with improvement on topical tetracycline application and resolution with topical or systemic steroids. The current case fits these criteria.
The clinical differential diagnosis of oral ulcers in HIV in a South African setting included histoplasmosis and tuberculosis ulcers. Histoplasmosis is a deep fungal infection caused by inhalation of soil and dust particles contaminated with spores of the fungus Histoplasma capsulatum. In an immune deficient host, the histoplasma infection disseminates into the blood stream leading to, amongst other manifestations, oral involvement.5,6 Oral histoplasmosis presents mostly as ulcerations that range from shallow to deep lesions with concomitant systemic symptoms such as weight loss, fever and malaise. South Africa has the highest worldwide HIV infection rate with the TB/ HIV co-infection rate of over 50% making TB a likely causative agent in our setting.7Mycobacterium tuberculosis primarily affects the respiratory system, however in disseminated cases oral involvement is possible. A few reports of primary oral tuberculosis have also been documented in the literature.8,9 Primary oral tuberculosis is postulated to result from direct mucosa inoculation by Mycobacterium tuberculosis and, rarely, by M. bovine. These infections present with long standing ulcers.
Other differential diagnoses in this case included cytomegalovirus (CMV) ulcer, syphilitic ulcers, Epstein-Barr virus (EBV) associated ulcer and neoplasms. CMV oral ulcers, although infrequent, are an indication of immune suppression. The virus-infected cells can be detected in tissue on routine histopathology examination, seen as large cells with large inclusion-like nuclei surrounded by a clear halo. Confirmation of virus infected cells is via a positive CMV immunohistochemistry stain. EBV associated oral ulceration has been described in immune-compromised individuals.10,11 The reported ulcers ranged from 1 to >2 cm and can involve both the keratinizing and non-keratinizing squamous mucosa. Histological examination reveals a polymorphous infiltrate of inflammatory cells within which there are scattered immunoblastic and Reed-Sternberg-like cells. These cells are EBV positive, detected using in-situ hybridization for EBV-encoded RNA.
It is important for the clinician to recognize and properly manage HIV patients with oral ulcers. The key features in the diagnosis of oral ulcers are the clinical history, size, duration of the lesions and whether they are single or multiple. Both local (trauma, chemical burn, etc.) and systemic causes of ulcers should be excluded. A single persistent firm non-healing ulcer with indurated margins may be an indication for malignancy and require further lymph node palpation. On the other hand multiple nonpersistent ulcers that heal spontaneously are commonly caused by viral infections or aphthous ulcers.12 It is not uncommon to have persistent ulcers in patient with HIV, which may take months to resolve. Systemic and autoimmune diseases such as lichen planus, lupus and pemphigoid are likely to present with multiple persistent ulcers. It should be remembered that TB is a great mimicker of malignancy and hence may present as a persistent non-healing ulcer. The management of HIV oral aphthous ulcers include pain management, chlorhexidine mouthwash and the maintenance of a good oral hygiene. A biopsy of all ulcers is mandatory to exclude infections and malignancy. The biopsy of the ulcer should include adjacent normal tissue.
CONCLUSION
Major oral aphthous ulcers result in significant patient morbidity due to pain, difficulty in eating and swallowing. The recognition of the entity is vital for proper patient management.
Declaration: No conflict of interest declared.
ACRONYMS
ARV: antiretroviral treatment
CMV: cytomegalovirus
EBV: Epstein-Barr virus
References
1. MacPhail LA, Greenspan D, Feigal DW, Lennette ET, Greenspan JS. Recurrent aphthous ulcers in association with HIV infection. Oral Surg Oral Med Oral Pathol 1991; 71: 678-83. [ Links ]
2. Miziara ID, Filho BCA, Weber R. AIDS and recurrent aphtous stomatitis. Braz J Otorhinolaryngol 2005; 71: 517-20. [ Links ]
3. Classification and diagnostic criteria for oral lesions in HIV infection. J Oral Pathol Med 1993; 22: 289-91. [ Links ]
4. Phelan JA, Eisig S, Freedman PD, Newsome N, Klein RS. Major aphthous-like ulcers in patients with AIDS. Oral Surg Oral Med Oral Pathol 1991; 71: 68-72. [ Links ]
5. Economopoulou P, Laskaris G, Kittas C. Oral histoplasmosis as an indicator of HIV infection. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 1998; 86: 203-6. [ Links ]
6. Ferreira OG, Cardoso SV, Borges AS, Ferreira MS, Loyola AM. Oral histoplasmosis in Brazil. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 2002; 93: 654-9. [ Links ]
7. Abdool Karim SS, Churchyard GJ, Abdool Karim Q, Lawn SD. HIV infection and tuberculosis in South Africa: an urgent need to escalate the public health response. Lancet 2009; 374: 921-33. [ Links ]
8. Khuzwayo ZB, Naidu TK. Head and neck tuberculosis in KwaZulu-Natal, South Africa. The Journal of Laryngology & Otology 2014; 128: 86-90. [ Links ]
9. Mignogna MD, Muzio LLO, Favia G, et al. Oral tuberculosis: a clinical evaluation of 42 cases. Oral Dis 2000; 6: 25-30. [ Links ]
10. Bunn B, van Heerden W. EBV-positive mucocutaneous ulcer of the oral cavity associated with HIV/AIDS. Oral Surg Oral Med Oral Pathol Oral Rad 2015; 120: 725-32. [ Links ]
11. Amorim Pellicioli AC, Luciano AA, Rangel ALCA, et al. Epstein-Barr virus (EBV)-associated posttransplant lymphoproliferative disorder appearing as mandibular gingival ulcers. Oral Surg Oral Med Oral Pathol Oral Rad 2016; 121: e80-e86. [ Links ]
12. Scully C, Felix D. Oral Medicine-Update for the dental practitioner. Mouth ulcers of more serious connotation. Br Dent J 2005; 199. [ Links ]
 Correspondence:
Correspondence:
Willie Fp van heerden:
Department of Oral Pathology and Oral Biology, University of Pretoria
Pretoria, South Africa.
Tel: +27 12 319 2320, Fax: +27 12 321 2225.
E-mail: willie.vanheerden@up.ac.za













