Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Dental Journal
versión On-line ISSN 0375-1562
versión impresa ISSN 0011-8516
S. Afr. dent. j. vol.71 no.2 Johannesburg mar. 2016
CASE BOOK
Oral medicine case book 72: A rare case of Nodular Fasciitis affecting the mandibular gingiva
NH WoodI; A MoodleyII
IBChD, DipOdont(MFP), MDent(OMP). Department of Periodontology and Oral Medicine, School of Oral Health Sciences, Sefako Makgatho Health Sciences University, Pretoria, South Africa
IIBDT, BDS, MDS. Department of Periodontology and Oral Medicine, School of Oral Health Sciences, Sefako Makgatho Health Sciences University, Pretoria, South Africa
ABSTRACT
Nodular fasciitis (NF) is a rapidly growing, myofibroblastic lesion with a challenging diagnosis. The deceptive clinical and histologic features of NF often lead to misdiagnoses that include malignancies. Nodular Fasciitis is benign and has a low recurrence rate after complete excision, which is the treatment of choice. Intra-oral lesions are especially rare. We describe the case of a 27 year old female who presented with localized, lobular-exophytic nodular fasciitis of the mandibular gingiva. To our knowledge, this is the ninth case to be reported occurring in this anatomic site and the forty-fifth intra-oral case.
Key words: Nodular Fasciitis, fibro-reactive lesion, gingival lesion, spindle-cell lesions
INTRODUCTION
Nodular fasciitis (NF), also known as pseudosarcomatous fasciitis or proliferative fasciitis, was first described by Konwaler in 1955.1,2 These benign, proliferative spindle cell lesions, comprised of fibroblasts and myofibroblasts, originate in subcutaneous tissue.1,2,3 Lesions are typically solitary, well-defined but unencapsulated, and undergo rapid enlargement.4,5,6 The rapid growth and lack of encapsulation often lead to a misdirected differential diagnosis in favour of malignancy, especially of the sarcomatous type.7,8
In adults, the upper extremities are the most commonly affected site.9 The head and neck region is the second most frequently affected area (7-20%), and in paediatric patients, tends to be the most commonly affected.6,8,9 Nodular fasciitis is rarely found intraorally8,9 because of the relative lack of fascia compared with other affected sites.3 The self-limiting nature of NF resulted in the description of a 'transient-neoplasia'.6,7,8
CASE REPORT
A 27 year old female patient presented with a main complaint of a lump in her mouth which became painful when eating. She sought treatment from a local clinic four months after noticing the lesion and was subsequently referred to Oral Medicine for management. She reported having a recent incident-free pregnancy. Her medical history was otherwise not remarkable.
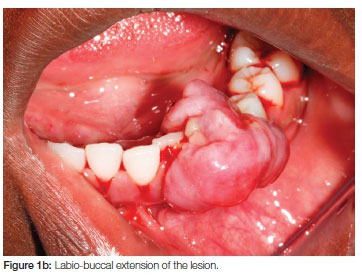
Extra-oral examination revealed palpable submandibular lymph nodes that were moveable and painless. Intra-orally the patient presented with poor plaque control evidenced by gross amounts of calculus. In the third quadrant, a large erythematous lobular lesion was found, originating from the interdental papilla between the 32 and 33 (Figures 1a and b). The exophytic lesion extended from the lingual to buccal aspects of the gingiva. Besides displacement of the 32 and the 33, nothing of significance was noted radiographically.
A differential diagnosis included pyogenic granuloma, pregnancy epulis, fibrous epulis and peripheral giant cell granuloma. Subsequent to the examination, cause-related periodontal therapy was performed, chlorhexidene 0,2% mouthwash was prescribed for use three times a day and plaque control instruction was given. An excisional biopsy was performed without complication. The lesion was sectioned and removed in two fragments measuring 2cm x 1,6cm and 1,3cm x 1cm, and the remaining gingivae was contoured to recreate the interdental tissue. The tissue segments were sent for histopathological investigation.
The patient was reviewed a week later and sutures were removed. At the two-week follow-up appointment the biopsy-site was seen to be healing uneventfully (Figure 2).

The biopsy report confirmed a diagnosis of nodular fasciitis, with the specimen showing polypoid proliferations composed of spindle- shaped cells with a feather-like appearance. The cells grew in bundles and fascicles and focal collections of lymphocytes were present (Figure 3a). Special staining techniques revealed positivity of SMA and negative staining for S100 (Figure 3b).
The patient was seen again at one and four months after the review when no signs of recurrence were discerned and the submandibular lymphnodes were no longer palpable.
DISCUSSION
The reported prevalence of NF in the head and neck ranges between 7-20%.4,9 Intraoral NF is rarely encountered and the most common intraoral site is the buccal mucosa.8,9 The lip, tongue, floor of the mouth and gingivae are also intraoral sites with documented involvement.6,8 The actual prevalence of intraoral NF is unknown and only 44 reports were found in the literature.
Previously NF was thought to be reactive in nature. Infection and hormonal influences have also been suggested as initiating factors.1,6,8 However, genetic research proves that NF undergoes a clonal expansion process.7 The recent discovery of a fusion gene shows that there are rearrangements of the USP6 locus with the formation of an MYH9-USP6 fusion gene.7
Although gender predilection is not demonstrated, our review shows that intraoral NF appears to be more prevalent in female patients and the significance of this is not yet apparent.1,2,4 Affected patients are usually in their 3rd to 5th decades of life.2,8,9
Diagnostic techniques vary when dealing with NF mainly because it may mimic malignancies. Clinicians have used incisional biopsies when the diagnosis was uncertain and excisional biopsies when the lesions were smaller and appeared well localized which is often the case when dealing with intraoral NF.9,10
The histological appearance of nodular fasciitis can be described as deceptive, due to its non- specific and, even though well demarcated, infiltrative nature.6 The lesion also has a rich vascularity and is mitotically active.4,6 This rapid growth and histological features make nodular fasciitis a mimicker of malignancies such as sarcomas.1,4 However, NF is a benign lesion and does not metastisize.4,9
Histological examination including immunohistochemistry is essential for accurate diagnosis.2 Lesional tissue often presents with loosely arranged fascicles of spindle cells in a fibrous or myxoid stroma, which is scattered with chronic inflammatory cells.1,6,9 It has been described as feathery looking.7 It is also non-encapsulated but described as being well delimited.9 Immunohistochemical assessments reveal a positive expression for smooth muscle actin, vimentin, HHF-35 and muscle specific actin1,3,5,8 and negative reaction for S100, desmin and cytokeratin.4,8
Nodular fasciitis can be histologically subtyped or classified using two methods, firstly according to the plane of tissue involved1 and secondly according to cellularity of the lesion.11 (Table 1) Sub-typing based on cellularity comprises three NF types: Myxomatous, Intermediate and Fibromatous. The histological appearance of Price's classification correlates with the duration of the lesion, with the lesions becoming more fibrous with longer duration.7 The classification using different tissue planes include: subcutaneous, intramuscular and fascial. The subcutaneous type is most prevalent and the intramuscular subtype is the least defined and is most commonly mistaken for a malignancy.8,9

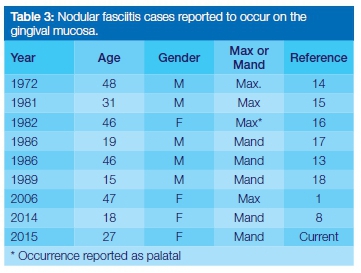
To our knowledge 45 cases of intraoral NF have been reported in the English literature. Searches spanning 1966 to 2015 have been conducted1,8,12 and the results for the prevalence of orofacial NF are summarized in Table 2, according to the anatomic location of the lesions. The buccal mucosa is the most commonly affected intraoral site, with 53,3% of intraoral NF lesions found at this location.1,12,13 Including our case report, nine NF lesions have been found on the gingiva (Table 3), making this the second most common site for the lesion to occur, followed by the lip, tongue and floor of the mouth.

Treatment of choice remains conservative total excision. Recurrence is rare,2,8,9,19 a rate of 1-2% having been reported.4 This could be due to incomplete removal of the primary lesion.4 However one report suggests that in cases where incomplete removal is not possible, the remaining lesional tissue may resolve spontaneously.20 This may be supported as a documented case of NF regression has been reported, the theory being that the regression was due to a shift in the lesion from a myxoid to a more fibrous stroma.21 The rare intraoral presentation of nodular fasciitis, especially on the gingiva, results in clinicians advising a close follow- up for patients.6
CONCLUSION
A rare case of intra-oral, lobular and exophytic gingival nodular fasciitis was presented. This is the ninth case report of this condition affecting the gingiva, and the 45th documented intra-oral case, to our knowledge. The differential diagnosis of exophytic gingival lesions should include NF. Appropriate stains should be applied to avoid the possibility of misdiagnosis as a malignancy. Recurrence is rare following surgical excision.
Acknowledgement:
Prof EJ Raubenheimer for providing the photomicrographs.
Conflict of interest: No conflict of interest declared
ACRONYM
NF: Nodular fasciitis
References
1. Han W, Hu Q, Yang X, Wang Z, Huang X. Nodular fasciitis in the orofacial region. Int J Oral Maxillofac Surg 2006;35:924-7. [ Links ]
2. Leventis M, Vardas E, Gkouzioti A, Chrysomali E, Chatzista-mou I. J Cranio-Maxillofac Surg 2011;39:340-2. [ Links ]
3. de Carli ML, Fernandes KS, dos Santos Pinto Jr D, Witzel AL, Martins MT. Nodular fasciitis of the oral cavity with partial spontaneous regression. Head and Neck Pathol 2013;7:69-72. [ Links ]
4. Haddad AJ, Avon SL, Clokie CML, Sandor GKB. Nodular Fasciitis in the oral cavity. J Can Dent Assoc 2001;67(11):664-7. [ Links ]
5. Martinez- Blanco M, Bagán JV, Alba JR, Basterra J. Maxillofacial nodular fasciitis: a report of three Cases. J Oral Maxillofac Surg 2002;60:1211-4. [ Links ]
6. Nair P, Barrett AW, Theodossya T. Oral nodular fasciitis: case report. Br J Oral Maxillofac Surg 2004;42;360-2. [ Links ]
7. Oliveira AM. Mesenchymal Tissue Pathology: Nodular Fasciitis. Pathobiology of Human Disease: A Dynamic Encyclopedia of Disease Mechanisms. http://dx.doi.org/10.1016/B978-0-12-386456-7.04402-6 [ Links ]
8. Lima FJ, de Sousa Lopes ML, de Oliveira Nobrega FJ, da Silveira EJ. A rare case of intraoral nodular fasciitis: diagnosis and immunohistochemical profile. J Oral Maxillofac Surg 2014;72:529-36. [ Links ]
9. Hino S, Masuda I, Fukai S, Kaneko T, Horie N, Shimoyama T. A case of nodular fasciitis involving the tongue. J Oral Maxillofac Surg Med Pathol 2014, http://dx.doi.org/10.1016/j.ajoms.2014.05.007 [ Links ]
10. Ikebe T, Ogata Y, Takamune Y, Ota K, Obayashi Y, Shinohara M. Nodular fasciitis in the buccal mucosa :a case report. Oral Science Int 2004;1(2):89-92. [ Links ]
11. Price EB, Silliphant WM, Shuman R. Nodular fasciitis: A clinico-pathologic analysis of 65 cases. Am J Clin Pathol 1961;35:122-36. [ Links ]
12. Dayan D, Nasrallah V, Vered M. Clinico-pathologic correlations of myofibroblastic tumors of the oral cavity: I. Nodular fasciitis. J Oral Pathol Med 2005;34:426-35. [ Links ]
13. Mostofi RS, Soltani K, Beste L, Polak E, Benca P. Intraoral periosteal nodular fasciitis. Int J Oral Maxillofac 1987;16(4):505-9. [ Links ]
14. Rakawer W. Fasciitis, an unusual diagnosis, and the clinician's dilemma: report of a case. J Oral Surg 1972; 29:503-6. [ Links ]
15. Sato M, Yanagawa T, Yoshida H, Yura Y, Shirasuna S, Miyazaki T. Submucosal nodular fasciitis arising within the buccal area. J Oral Surg 1981; 10:210-13. [ Links ]
16. Takagi M, Ishikawa G. Fibromatosis of the oral cavity. Bull Tokyo Med Dent Univ 1982;29:113-22. [ Links ]
17. Freedman PD, Lummerman H. Intravascular fasciitis: report of two cases and review of the literature. Oral Surg 1986;62:549-54. [ Links ]
18. Davies HT, Bradley N, Bowerman JE. Oral nodular fasciitis. Br J Oral Maxillofac Surg 1989; 27:147-51. [ Links ]
19. Naidu A, Lerman MA. Clinical Pathologic Conference Case 3: Nodular fasciitis. Head and Neck Pathol 2011; 5:276-80. [ Links ]
20. Subramaniam P, Balakrishna R, Mahendra P, Gilhotra K. Nodular fasciitis of the oral region. Contempt Clin Dent 2012;3:3,Suppl S1:16-8. [ Links ]
21. Yanagisawa A and Okada H. Nodular fasciitis with degeneration and regression. J Craniofac Surg 2008;19(4):1167-70. [ Links ]
 Correspondence:
Correspondence:
Neil Hamilton Wood
Department of Periodontology and Oral Medicine, School of Oral Health Sciences
Sefako Makgatho Health Sciences University
Pretoria, South Africa 0204
Tel: 012 521 4834. Fax: 012 521 4835
E-mail: Neil.Wood@smu.ac.za