Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.71 n.2 Johannesburg Mar. 2016
RESEARCH
Penetration of hydrogen peroxide into the pulp chamber after conventional and laser-assisted bleaching
LR OmraniI; A TaherII; A AlbujeerIII; M ParvinIV; G DaryakenariV; S Gorgani-FiruzjaeeVI; Η KermanshahVII; V ChiniforushVIII
IDDS, MSc. Assistant Professor, Department of Restorative and Esthetic Dentistry, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran
IIMSc, MBA, MFDRCPSG, FACOMS, FCS, FCIM. Department of OMF Surgery, Faculty of Dentistry, University of Kufa
IIIDDS. School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran
IVDDS. School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran
VDDS. School of Dentistry, Tehran University of Medical sciences, Tehran, Iran
VIDDS. Department of medical Laboratory Sciences, School of Allied Health Medicine, Aja university of medical sciences, Tehran, Iran
VIIDDS. Associate Professor, Department of Restorative and Esthetic Dentistry, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran
VIIIDDS, PhD. Laser research Center of Dentistry, Dental Research Institute, Tehran University of Medical Sciences, Tehran, Iran
ABSTRACT
BACKGROUND: Bleaching is a conservative approach to improve tooth colour. Laser irradiation accelerates the process by activating the hydrogen peroxide (HP) bleaching agent. However, there is little data examining whether this might result in pulp injury by enhancing HP penetration and diffusion. This study measured HP penetration into the pulp chamber with different bleaching techniques.
METHODS: Fifty extracted central maxillary incisors were collected, disinfected, root treated and stored in sterile saline solution. The pulp chambers were filled with an acetate buffer solution. Bleaching was performed with one of four methods: 1. Conventional in-office bleaching; and accelerated bleaching using 2. :yttrium-aluminium-garnet (Nd:YAG), 3. 1w Diode, and 4. 1.5w Diode lasers. A fifth control Group received no treatment. The buffer solution was drained and stained by colourimetric spectrophotometry to determine optical densities, which were analyzed by one-way ANOVA followed by Tukey honest significant difference (HSD) test.
RESULTS: The greatest penetration occurred with the conventional in-office bleaching procedure (2.232 ± 0.39μg), while the least was seen with Diode (1w) laser-assisted bleaching (0.31 ± 0.28μg). : Provided the manufacturer's recommendations are followed, laser acceleration does not exacerbate penetration of HP into the pulp chamber.
Key words: hydrogen peroxide, tooth bleaching, Nd:YAG laser, Diode laser
INTRODUCTION
Bleaching is a simple, conservative, non-invasive, and inexpensive way of lightening tooth colour, and is a popular way of enhancing beauty and youthfulness.1-4 New methods and materials are currently being developed and introduced.
Bleaching may either be done in-office or at home by the patient.1 Hydrogen peroxide (HP) at a concentration in the range of 10%-40% or other chemicals capable of producing HP (e.g., carbamide peroxide, sodium perborate) are most commonly used to oxidize organic materials, inducing tooth colour change.5,6 Perhydroxyl radicals can break down large compounds into simpler molecules, with weaker light reflecting properties, thus giving a brighter appearance to the teeth.4 About 30%-35% HP application for up to 30min is considered standard in order to minimize any surface changes to the enamel. Bleaching gels should have a ph of 9.8-10.5, which enhances perhydroxyl radical production while reducing reactive oxygen radicals.7
Power bleaching is one approach that contributes to the efficacy of bleaching procedures.8 This method was pioneered by Abbot, who used high-intensity light to accelerate the whitening process.9 This was later followed by other acceloratory methods.10-12 The application of laser light, specifically 810 or 980nm Diode laser, and Nd:YAG with 1064nm wavelength, has been found to possess photochemical whitening effects.13
Two theories are proposed to explain the action of light on bleaching efficacy: (1) light and heat might accelerate HP breakdown14,15 and (2) light and heat might facilitate HP penetration into tooth structure.16
According to these theories, the laser-accelerated bleaching methods may encourage more HP penetration into pulp, which would induce oxidative stress,17 inhibition of pulpal enzymes,18 inflammatory pulp reaction,19 and subsequently postoperative dental hypersensitivity.20
The present study aimed to quantify the penetration of HP into the pulp chamber during different in-office bleaching methods, including laser-accelerated approaches.
MATERIALS AND METHODS
Fifty central maxillary human incisors were collected during a three-month period. They had been extracted due to periodontal problems, and all patients had provided informed consent to their use. Teeth were cleansed of soft tissues and calculus; and the absence of cracks, abrasion, or defects was verified by stereomicroscope (Nikon, SMZ800, Japan). The specimens were soaked in 0.5% chloramine-T for one week, after which they were stored in saline solution until required.
Using a separating disk (Shofu, Japan), the root of each specimen was truncated 2mm apical to the cemento enamel junction (CEJ). Pulp chambers were cleaned using headstrom files (Maillefer, MI, USA), irrigated with saline, and then widened using a round bur to allow micro-pipette access.
A standard size (4 χ 6mm) area was marked on each tooth surface by applying two coats of nail varnish to the surrounding surface.
After drying the pulp chambers with paper cones, the specimens were fixed vertically on a wax plate. A micro-pipette was used to place 50μ! of acetate buffer solution 2M (pH 4.5) into each pulp chamber. This solution served to stabilize any HP penetration into the pulp chamber.21-25
The 50 specimens were subdivided at random into five Groups of 10 teeth each.
Group A: Conventional in-office bleaching
The bleaching gel Opalescence Boost PF (40% - Ultradent Products Inc., South Jordan, UT, USA) was applied as a 2mm layer on the marked-out area. After twenty minutes, the acetate buffer was extracted from the pulp chamber by micro-syringe for examination/analysis.
Group B: Nd:YAG laser-assisted bleaching
The bleaching gel was applied as a 2mm layer on the marked-out area. Two minutes after application of the gel, Nd:YAG laser (Fotona, Slovenia, Fidelis - 1064nm, 2.5w, 25Hz) irradiation was administered using a 320μm fiber, for three exposures of 30 seconds each, with 1min between each laser application. Three minutes after the last laser treatment, the acetate buffer was extracted. Hence the total time of bleaching was 8min and 30sec which was in accord with the manufacturer's instruction.
Group c: Diode (1w) laser-assisted bleaching
The bleaching gel was applied as a 2mm layer on the marked-out area. Two minutes after application of the bleaching gel, Diode laser (Wuhan, gigga model: DEN7A, China- 810nm, 1w, continuous wave) irradiation was administered using a 4mm fibre, in the same way as for Group B. resulting in a total time of bleaching of 8min and 30sec.
Group D: Diode (1.5w) laser-assisted bleaching
The same procedure was followed for Group D, but using a 1.5w power Diode laser. Again the total time of bleaching was 8min and 30sec.
Control Group: No bleaching treatment
Specimens underwent no treatment; the buffer solution was extracted for testing after 20min.
For each tooth, the extracted solution was transferred into a micro-tube. The pulp chamber was then irrigated twice with 50μl distilled water, and that 100μl was also transferred to the tube. One hundred micro litres of 0.5mg/ml leuco-crystal violet (Aldrich: Sigma-Aldrich Chemie GmbH, Steinheim, Germany) and 50μ! of 1mg/ml horseradish peroxidase enzyme (Sigma; Sigma Chemical Co., St Louis, MO, USA) were added to the micro-tube, which was then filled with 2700μ! distilled water, bringing the contents to 3ml volume. The process was followed for every specimen. The resulting blue solutions were examined with an UV-visible spectrophotometer (Novaspec 2, Pharmacia) at a wavelength of 596 m at room temperature, to measure the optical density (OD).26 The ODs which were obtained were then converted to micrograms using the spectrophotometer calibration curve, which was drawn up from the values resulting from spectrophotometer evaluation of different HP concentrations. The results were analyzed with one-way ANOVA, followed by Tukey's HSD test for pairwise comparison between Groups.
RESULTS
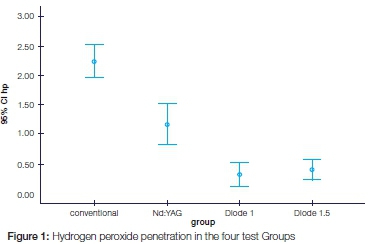
The deepest HP penetration was observed in Group A (2.232 ± 0.39pg) while the lowest values were observed in Group C (0.31± 0.28pg) (Table 1).
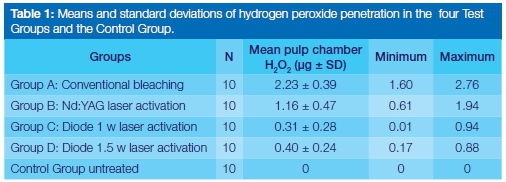
The amount of HP that had entered the buffer solution of the control Group was negligible (0.001μg) on the spectrophotometer absorption curve; this was deemed to be due to mild contamination in procedural errors and was considered as zero.
A statistically significant difference was found between each pair of study Groups (P < 0.001) except for Groups C and D (P = 0.954) (Figure 1).
DISCUSSION
One of the common complaints after bleaching treatment is tooth sensitivity. It has been suggested that this might be the result of HP penetration through the tooth structure into the pulp chamber or due to an increased temperature of the pulp during power bleaching. HP might cause the release of inflammatory mediators and stimulate sensory nerves. It thus appears to be of importance to select a method that minimizes HP penetration into the pulp.27 Recently, many activating methods have been introduced for in-office bleaching, in order to achieve better results in shorter times. These include laser irradiation. However the safety of such methods is not clear.
The lasers used in the present study all operate in the infrared spectrum, and possess photochemical properties. It is obvious that the bleaching gel must contain pigments and therefore Opalescence Boost PF, which contains red pigments in the form of carotene, was selected. The time of gel application for each Group was the minimum time recommended by the manufacturers. Although the manufacturers declare that activation of the bleaching gel, as applied in this study, is not necessary, research has shown that the use of a Diode laser or LED light enhances the gel's whitening effect, reducing the duration of treatment.28,29
According to physical laws, the amount of diffusing substance depends directly on the surface area through which it can diffuse, and, inversely, on the diffusion distance.3 Consequently, application areas of equal surface area were outlined with nail polish, and teeth of the same size were selected for inclusion in the study.
Many different spectrophotometric methods have been used to quantify the amount of HP in micrograms. The leuco crystal violet (LCV) method is fast, simple, and sensitive.23 It is based on oxidation reaction of LCV buffer solution in the presence of HP and horseradish peroxidase as a catalyzer. The crystal violet ion forms a blue solution that absorbs at 590 nm and remains stable for several days.26
HP was detected in the pulp chambers of all bleached Groups. This is in accordance with other studies.30,31 Hard dental tissues have a high degree of permeability.32 HP penetrates dental tissues as it has a low molecular weight, in addition to the ability to denature proteins and replace ions, which amplifies the depth and amount of penetration.2,33
The highest HP penetration was observed in Group A. This might be the result of the extended bleaching gel application time, allowing more penetration into dental structures, and inducing a destructive effect on dental structure that further increases permeability.34
The present findings are in agreement with other studies.37,38 Haywood showed that 35% HP can reach the pulp tissue within 15 min,37 a finding similar to that found in this study.
Another finding was that HP penetrated to a greater extent in the Nd:YAG laser Group. This laser is reported to be capable of greater activation of the bleaching gel, due to the fact that its wavelength is higher than that of the Diode laser (1064 vs. 810-830nm), which reduces its penetration depth but allows absorption in the bleaching gel. Most of the laser energy therefore heats the gel, resulting in higher HP release. Pulpal penetration may therefore be expected. However, 1w and 1.5w Diode lasers did not significantly alter the penetration rates, showing that, at those wavelengths, altering the laser power has little significance.38
Camargo et al. reported that application of Nd:YAG or LED laser during the bleaching process increased HP penetration as compared with their control Group which received no activation protocol.3 The bleaching gel application period was the same in the three test Groups in their study, making the results clinically irrelevant, because the purpose of activating agents is to achieve better results in a shorter time.
The present in vitro study, obviously, merely offers a possible window into what might happen in vivo, which has yet to be clarified.18 There are at least two possible in vivo mechanisms that could act to stop the penetration of HP molecules, namely: positive pulp pressure and the osmotic pressure of the bleaching gel.39 In addition to these possibilities, vital pulp possesses defense systems that protect it, including the enzymes peroxidase and catalase, which would be beneficial if HP molecules succeeded in reaching the pulp tissue.40 Moreover, according to Bowles et al., for HP to have a negative impact on pulp enzymes, its concentration must reach 50000 pg.18 Among the possible negative side effects of HP penetration into the pulp, only reversible side effects, for example sensitivity, have been reported.
CONCLUSION
This study appears to show that, provided the manufacturer's recommendations are followed, using laser activation for bleaching will not result in increased HP penetration into the dental pulp system.
Conflicts of Interest: None declared
Acknowledgments: Thank you to Benedicenti Stefano and Angiero Francesca, University of Genoa, Department of Surgical Sciences and Integrated Diagnostics, Genoa, Italy for their collaboration in this reaserch.
This article was supported by grant no. 91-04-97-19814 (Laser Research Center of Dentistry, Dental Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
ACRONYMS
CEJ: cemento enamel junction
HP: hydrogen-peroxide
HSD: honest significant difference
LCV: leucocrystal violet
Nd:YAG: neodymium:yttrium-aluminium-garnet
References
1. Camargo SE, Valera MC, Camargo CH, Gasparoto Mancini MN, Menezes MM. Penetration of 38% hydrogen peroxide into the pulp chamber in bovine and human teeth submitted to office bleach technique. J Endod. 2007;33(9):1074-7. [ Links ]
2. Soares DG, Ribeiro APD, Sacono NT, Loguercio AD, Hebling J, Costa CADS. Mineral loss and morphological changes in dental enamel induced by a 16% carbamide peroxide bleaching gel. Braz Dent J. 2013;24(5):517-21. [ Links ]
3. Camargo SE, Cardoso PE, Valera MC, de Araujo MA, Kojima AN. Penetration of 35% hydrogen peroxide into the pulp chamber in bovine teeth after LED or Nd:YAG laser activation. Eur J Esthet Dent. 2009;4(1):82-8. [ Links ]
4. Gokay O, Mujdeci A, Algin E. In vitro peroxide penetration into the pulp chamber from newer bleaching products. Int Endod J. 2005;38(8):516-20. [ Links ]
5. Baik JW, Rueggeberg FA, Liewehr FR. Effect of light-enhanced bleaching on in vitro surface and intrapulpal temperature rise. J Esthet Restor Dent. 2001;13(6):370-8. [ Links ]
6. Luk K, Tam L., Hubert M. Effect of light energy on peroxide tooth bleaching. J Am Dent Assoc. 2004;135(2):194-201. [ Links ]
7. Verheyen P. Laser-assisted bleaching: smart bleach. J Oral Laser Applications 2001;1(3):207-13. [ Links ]
8. Jordan RE, Boksman L. Conservative vital bleaching treatment of discoloured dentition. Compend Contin Educ Dent. 1984;5(10):803-5, 807. [ Links ]
9. Abbot C. Bleaching discoloured teeth by means of 30% perhydrol and electric light rays. J Allied Dent Soc. 1918;13:259. [ Links ]
10. Sun G. The role of lasers in cosmetic dentistry. Dent Clin North Am. 2000;44(4):831-50. [ Links ]
11. Buchalla W, Attin T. External bleaching therapy with activation by heat, light or laser-a systematic review. Dent Mater. 2007;23(5):586-96. [ Links ]
12. Dostalova T, Jelinkova H, Housova D, Sulc J, Nemec M, Miyagi M, et al. Diode laser-activated bleaching. Braz Dent J. 2004;15 Spec No, SI3-8. [ Links ]
13. Garber DA. Dentist-monitored bleaching: a discussion of combination and laser bleaching. J Am Dent Assoc. 1997;128(Suppl):26S-30S. [ Links ]
14. Sulieman M, MacDonald E, Rees JS, Addy M. Comparison of three in-office bleaching systems based on 35% hydrogen peroxide with different light activators. Am J Dent. 2005;18(3):194-7. [ Links ]
15. Joiner A. Tooth colour: a review of the literature. J Dent. 2004;32:3-12. [ Links ]
16. Wiegand A, Vollmer D, Foitzik M, Attin R, Attin T. Efficacy of different whitening modalities on bovine enamel and dentin. Clin Oral Investig. 2005;9(2):91-7. [ Links ]
17. Anderson DG, Chiego DJ Jr, Glickman GN, McCauley LK. A clinical assessment of the effects of 10% carbamide peroxide gel on human pulp tissue. J Endod. 1999;25(4):247-50. [ Links ]
18. Bowles WH, Ugwuneri Z. Pulp chamber penetration by hydrogen peroxide following vital bleaching procedures. J Endod. 1987;13(8):375-7. [ Links ]
19. Soares DG, Ribeiro APD, da Silveira Vargas F, Hebling J, de Souza Costa CA. Efficacy and cytotoxicity of a bleaching gel after short application times on dental enamel. Clin Oral Inves-tig. 2013;17(8):1901-9. [ Links ]
20. Markowitz K. Pretty painful: Why does tooth bleaching hurt? Med Hypotheses 2010;74(5):835-40. [ Links ]
21. Cooper JS, Bokmeyer TJ, Bowles WH. Penetration of the pulp chamber by carbamide peroxide bleaching agents. J Endod. 1992;18(7):315-7. [ Links ]
22. Gokay O, Tuncbilek M, Ertan R. Penetration of the pulp chamber by carbamide peroxide bleaching agents on teeth restored with a composite resin. J Oral Rehabil. 2000;27(5):428-31. [ Links ]
23. Mottola HA, Simpson BE, Gorin G. Absorptiometric determination of hydrogen peroxide in submicrogram amounts with leuco crystal violet and peroxidase as catalyst. Anal Chem. 1970;42:2. [ Links ]
24. Gokay O, Yilmaz F, Akin S, Tuncbilek M, Ertan R. Penetration of the pulp chamber by bleaching agents in teeth restored with various restorative materials. J Endod. 2000;26(2):92-4. [ Links ]
25. Adibfar A, Steele A, Torneck CD, Titley KC, Ruse D. Leaching of hydrogen peroxide from bleached bovine enamel. J Endod. 1992;18(10):488-91. [ Links ]
26. Gokay O, Mujdeci A, Algn E. Peroxide penetration into the pulp from whitening strips. J Endod. 2004;30(12):887-9. [ Links ]
27. Soares DG, Basso FG, Pontes EC, Garcia LDF, Hebling J, de Souza Costa CA. Effective tooth-bleaching protocols capable of reducing H2O2 diffusion through enamel and dentine. J Dent. 201442(3):351-8. [ Links ]
28. Yiming L. Safety controversies in tooth bleaching. Dent Clin North Am. 2011;55:9. [ Links ]
29. Gurgan S, Cakir FY, Yazici E. Different light-activated in-office bleaching systems: a clinical evaluation. Lasers Med Sci. 2010;25(6):817-22. [ Links ]
30. Bharti R, Wadhwani KK. Spectrophotometric evaluation of peroxide penetration into the pulp chamber from whitening strips and gel: an in vitro study. J Conserv Dent. 2013;16(2):131. [ Links ]
31. Patri G, Agnihotri Y, Rao SR, Lakshmi N, Das S. An in vitro spectrophotometric analysis of the penetration of bleaching agent into the pulp chamber of intact and restored teeth. J Clin Diagn Res. 2013;7(12):3057. [ Links ]
32. Lefkowitz W, Bodecker CF. Concerning the vitality of the calcified dental tissues. II The permeability of enamel. J Dent Res. 1938;17(6):453-63. [ Links ]
33. Jain RJ, Jadhav SK, Hegde VS. Effects of conventional and laser activated intracoronal bleaching agents on ultrastructure and mineral content of dentin. J Dent Lasers. 2013;7(1):2. [ Links ]
34. Marson FC, Gonçalves RS, Silva CO, Cintra LT, Pascotto RC, Santos PD, et al. Penetration of hydrogen peroxide and degradation rate of different bleaching products. Oper Dent. 2015;40(1):72-9. [ Links ]
35. Seale NS, Wilson CF. Pulpal response to bleaching of teeth in dogs. Pediatr Dent. 1985;7(3):209-14. [ Links ]
36. Costa CA, Riehl H, Kina JF, Sacono NT, Hebling J. Human pulp responses to in-office tooth bleaching. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(4):e59-64. [ Links ]
37. Haywood VB. Overview and status of mouthguard bleaching. J Esthet Dent. 1991;3(5):157-61. [ Links ]
38. He LB, Shao MY, Tan K, Xu X, Li JY. The effects of light on bleaching and tooth sensitivity during in-office vital bleaching: a systematic review and meta-analysis. J Dent. 2012;40(8):644-53. [ Links ]
39. Thitinanthapan W, Satamanont P, Vongsavan N. In vitro penetration of the pulp chamber by three brands of carbamide peroxide. J Esthet Dent. 1999;11(5):259-64. [ Links ]
40. Bowles WH, Burns H Jr. Catalase/peroxidase activity in dental pulp. J Endod. 1992;18(11):527-34. [ Links ]
 Correspondence:
Correspondence:
Kermanshah hamid
Associate Professor, Department of Restorative and Esthetic dentistry
School of Dentistry, Tehran University of Medical Sciences
Tehran, Iran
E-mail: kermanshahhamid@yahoo.com













