Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.70 n.10 Johannesburg Nov. 2015
RESEARCH
Assessing extent of undergraduate training in maxillo-facial surgery and the related skill levels amongst public service dentists
M MabongoI; M D ThekisoII; V YengopalIII
IBDent, BDS, MChD (Maxillofacial and Oral Surgery). Department of Maxillofacial and Oral Surgery, School of Oral Health Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
IIBChd, MDent (Community Dentistry); Department of Community Dentistry, School of Oral Health Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
IIIBChD, BSc, MChD (Community Dentistry); Department of Community Dentistry, School of Oral Health Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
ABSTRACT
AIM: To assess the level of maxillofacial surgical skills amongst dentists in the Public Oral Health Services.
OBJECTIVES: To determine the level of training dentists had received in maxillofacial surgical skills during their undergraduate studies. To identify the training needs of dentists working in the public oral health sector.
METHODS: A self-administered questionnaire was designed and sent to 96 dentists who were employed in the Public Oral Health Services between 2011 and 2012. The questionnaire elicited information on demographics and on the levels of undergraduate training the dentists had received in oral surgical skills.
RESULTS: Seventy replies were received, a response rate of 73%. Respondents had received undergraduate training in the following procedures: surgical removal of impacted teeth 85.7%, closed reduction of fractured jaws 72.9%, placement of dental implants 14.3%, and incisional biopsies, 72.9%. Postgraduate training was considered required before attempting surgical removal of impacted third molars (41.4%), closed reduction of fractured jaws (67.1%), incisional (61.7%) and excisional (56.3 %) biopsies.
CONCLUSION: Dentists working in the Public Oral Health Services believed that their undergraduate training in maxillofacial surgery did not equip them to perform more complex surgical procedures with skill and confidence.
Keywords: third molars; closed reduction; dental implants; biopsy
INTRODUCTION
Public Oral Health (POH) services in Gauteng, South Africa are provided by dentists, dental therapists and oral hygienists, mainly at Primary Health Care (PHC) facilities and District hospitals (DH). These facilities are often the first contact point for patients who require a range of primary oral healthcare services. These needs include fillings, prophylaxis, extractions, emergency endodontics, denture services, oral health education and promotion, preventive interventions and extend to minor oral surgery procedures such as removal of impacted wisdom teeth and fracture stabilisation. In Gauteng there are two academic dental hospitals located in the Johannesburg Metro region [Charlotte Maxeke and Chris Hani-Baragwanath Hospital affiliated to the University of Witwatersrand (Wits). In addition, there are another two academic hospitals located in the Tshwane region [Steve Biko and Dr George Mukhari Hospitals], affiliated to the University of Pretoria (UP) and to the Sefako Makgatho University respectively. These tertiary hospitals each have a maxillofacial department staffed by qualified maxillofacial surgeons and by registrars.
Although South African qualified dentists are expected to have received formal training in minor oral surgery during their undergraduate program; patients presenting at PHC facilities and DH in Gauteng are often referred by the attending dentist to tertiary dental hospitals, especially when the problem is impacted wisdom teeth.1 However, patients have difficulty in accessing these services because of transport problems, physical immobility and long waiting lists.2 Furthermore, the provision of such services in tertiary care settings places considerable financial constraints on the budgets of academic dental hospitals.
Oral health services (OHS) are classified into primary, secondary and tertiary health services. Competencies for primary OHS are clearly stated in the norms and standard documents,3 and include oral health promotive and preventive services, basic treatment services, emergency relief of pain and sepsis and minor oral surgery procedures. Secondary health services are mainly curative and are rendered in District hospitals. Unfortunately, these hospitals do not include Public Oral Health Services in their budgets. Almost inevitably, patients from the district primary OHS are referred directly to the academic hospitals.
Hobdell et al4and Myburg et al5identified that Africa suffers a very high prevalence of orofacial trauma, and of noma, oral cancer and oral manifestations of HIV. According to the Primary Oral Health Care Package3 some of the orofacial pain should be managed in level 1 District hospitals. The norms and standards for District hospitals6,7 highlight the expectation that competencies for oral health staff should include the ability to recognise and deal with the following procedures: trauma to the teeth and oral cavity; inhaled or swallowed foreign body including performing a Heimlich manoeuvre; lacerations of the tongue and face; swallowing problems and dislocated or fractured jaws. The staff should be able to perform airway maintaining procedures like draining abscesses that may cause airway obstruction e.g. Ludwig's angina.
The draft South African Oral Health Strategic document8 prescribes competencies as minimum requirements for employment of Dentists in level 1 District hospitals. These include the ability to carry out the following procedures: closed reduction of fractured jaws (IMF), removal of class I dental impactions, surgical removal of teeth, biopsies, immobilisation of loose, avulsed or inflexed teeth and multiple exodontia under General Anaesthesia (GA). The regional (Level 2) hospital service package for South Africa does not cover oral health, but recognises maxillofacial and oral surgery as a sub-specialty of surgery and recommends that a maxillofacial surgeon be appointed either on a permanent or sessional basis.6,7
There is evidence that the large number of referrals for minor oral surgical procedures such as impacted wisdom teeth are causing bottlenecks at the tertiary centres as the specialists cannot cope with the volume of patients.1 Many could be handled at PHC facilities but dentists continue to refer patients with these minor conditions to specialist centres even though they are expected themselves to have the skills to manage such problems.
This survey reports on an audit of surgical skills of dentists in the Public Oral Health Services in Gauteng. The objectives were (1) to determine the level of training dentists had received in maxillofacial minor oral surgery during their undergraduate study, and, (2) to identify the deficiencies in surgical skills and the surgical needs of dentists working in the public sector in Gauteng.
MATERIALS AND METHODS
This was a cross-sectional study, conducted between 2011-12 with the permission of the Director of Specialised Services, Gauteng Department of Health, and the approval of the University of Witwatersrand Human Research Ethics Committee [M130528]. A self-administered questionnaire was designed and sent to dentists employed in the POH services in Gauteng. The questionnaire elicited information on demographics and on specifics of the undergraduate training in the surgical skills required by the draft South African Oral Health Strategic document. Participants were further asked whether they practised these surgical skills in their district clinics and whether they required further training. Data were collected and analysed using Microsoft Excel and STATA 11 software version 15, and associations were tested using a chi-square test at a level of significance of p<0.05.
RESULTS
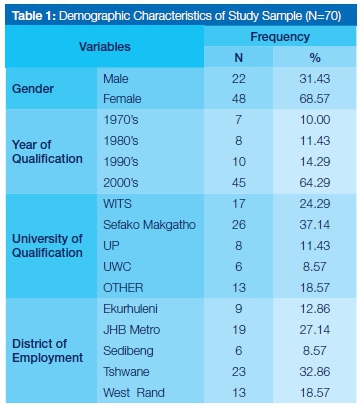
Questionnaires were sent to ninety-six dentists employed in the public sector and seventy responses were received (response rate 72.91%). A total of 48 (68.57%) were female and 22 (31.43%) were male. The majority (64.29%) of the participants had qualified during and post the year 2000, with only 10% having qualified in the 1970's. The Sefako Makgatho University provided the highest number of dental graduates (37.14%) followed by the University of Wit-watersrand (Wits) with 24.29%, the University of Pretoria (11.43%) and the University of Western Cape (UWC) with the lowest percentage at 8.57%. Graduates from universities outside of South Africa accounted for 18.57%. The Tshwane and Johannesburg Metro had the highest number of dentists employed in the various clinics (Table 1).
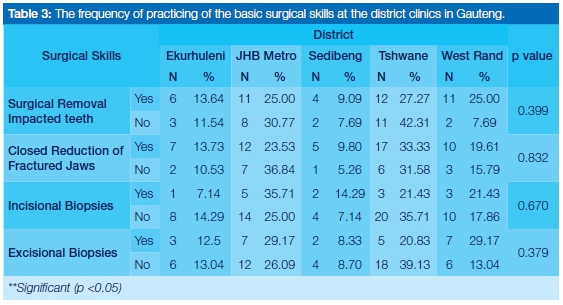
Eighty-five percent of the participants indicated having received undergraduate training in the surgical removal of impacted wisdom teeth. A small group (15%) reported not having received adequate undergraduate training in this procedure, of whom 70% were from Wits. This was significantly more than from the other dental schools. However, this should be interpreted with caution due to the small sample size. Other relevant findings were that 100% of graduates from UP reported that they had received training on the closed reduction of fractured jaws; whilst fewer than 8% of graduates from UWC had received training in biopsy procedures (Table 2). Analysis of the relationship between the practice of the basic surgical skills at the district clinics indicated that approximately 63% of dentists had removed impacted wisdom teeth surgically, 73% had performed closed reduction of fractured jaws and only 20% had performed incisional biopsy procedures at these institutions (Table 3).
There was a significant difference between perceived postgraduate training needs in the surgical removal of impacted teeth (55.7%) and the performance of excisional biopsies (60%) [p<0.05]. The majority of dentists from the Tshwane district (70%) reported that they required post-graduate training in surgical removal of impacted wisdom teeth while most dentists from the West Rand (77%) reporting that they did not require training on performing excisional biopsies (Table 4).
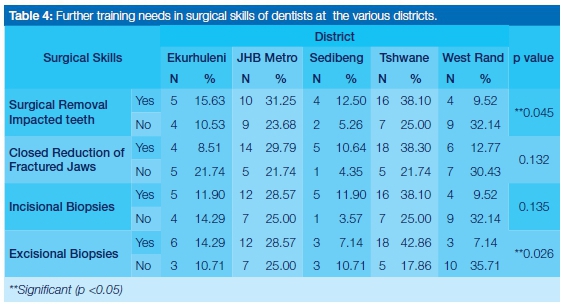
A further analysis was done to determine the postgraduate needs of the dentists and these data were related according to the University from which the respondents had graduated. Fewer than 30% of graduates from three of the four Universities indicated that they did not need further postgraduate training in the surgical removal of impacted teeth, incisional biopsy, excisional biopsy and closed reduction of fractured jaws. Approximately 45% of graduates from Sefako Mak-gatho University felt that they needed more post-graduate training on these interventions and this was significantly higher than the percentages reported for the other three universities (p<0.05). Sixty percent of dentists who had qualified in the 1980's and 1990's indicated the need for further training in closed reduction of fractured jaws, with a significant correlation (p< 0.05) between year of qualification and the acknowledgment of that need.
DISCUSSION
The study found that although approximately 86% of dentists reported they had received undergraduate training in the surgical removal of impacted third molars, only 63% had actually undertaken this procedure in their district clinics.1 These findings are comparable with those of Yiu et al9who surveyed newly qualified dentists in Hong Kong and reported that more than 52% felt comfortable in the area of oral and maxillofacial surgery, 98% felt competent to perform simple extractions, 62% felt confident to remove impacted third molars and 58% were able to manage complications of oral surgery. However, 64% of dentists felt inadequately prepared to identify and manage oral pathology with 82% not comfortable to perform soft-tissue biopsies, and only 54% of dentists undertaking such biopsies. In Mangalore, Taluk, India, Simon et al.10reported that no oral health center provided for the removal of impacted teeth and oral biopsies; all complicated dental treatments were referred to the nearest Dental College or to the Dental Wing of the nearby Government Hospital, due to lack of equipment and staff.
Although the present study did not investigate the reasons for referral of patients to the Academic hospitals, Coulthard et al11reported that generally 69% of dentists made referrals because of the anticipated difficulty of surgery and 49% because of the complex nature of the patient's medical history. In the South African context it is possible that the lack of equipment and high workloads are the reasons driving a high rate of referrals of patients for these procedures. Anecdotal evidence also suggests that lengthy procedures are not performed by the dentists at the lower level facilities as assessment of their performance is based on the number of procedures/patients treated rather than the nature of the procedure performed.
There was no significant difference between the females and males in relation to their undertaking extraction of impacted wisdom teeth. Our findings differ from Coulthard et al.11who reported that in the United Kingdom female practitioners were less confident than male practitioners in relation to surgical skills. The study also showed that twenty seven percent of females and 13% of males performed incisional biopsies, approximately 43% females and 28% males did excisional biopsies; and 55% of females and 72% of males treated fractured jaws by closed reduction. In a study conducted in Manchester, United Kingdom, Diamanti et al.12reported that 15% of dentists surveyed had performed oral biopsies but 60% felt that they lacked the skills to perform a biopsy even on benign lesions. Their main reasons for this were inadequate training and experience, and the fear of diagnostic error. In a developing country such as South Africa, the provision of these basic surgical services would improve the level of services to patients by not requiring them to attend a tertiary facility. This would also reduce the workload at the tertiary institutions and be more cost effective.
An analysis of the relationships between year of qualification and the practice of the different basic surgical skills found that the majority of dentists (70%) who had qualified during the 1980's and 1990's extracted impacted teeth surgically in their respective districts compared with those who qualified in the 2000's (10%). This was not statistically significant. However there was a significant difference between year of qualification and the performing of closed reduction of fractured jaws (p>0.05), with approximately 71% of dentists who qualified in the 1970's indicating that they did not require further training in closed reduction of fractured jaws compared with those who qualified in the 1980-2000's who were not confident in the treatment. The older clinicians may have accumulated experience in their facilities due to the high prevalence of injuries requiring closed reduction of the jaws, related to the elevated levels of inter-personal violence in the country.13
This study had limitations in that the participants were required to provide retrospective opinions on undergraduate training, which could have resulted in acquiescence or information bias. Clinical practice in the public sector has particular features, with patient volumes, treatment demands and opportunities distinguishing it from private sector practice.
CONCLUSION
The study showed that dentists working in the Public Oral Health Services of Gauteng reported a limited experience of surgical skills in maxillofacial surgery learned at undergraduate level. Oral Health Services provided by dentists in the Public sector could be improved if there was enhanced co-ordination amongst the different Dental Schools in South Africa in the training of dental undergraduates in specific surgical skills. There is also a need to offer postgraduate courses to improve clinical competency in minor oral surgery.
ACRONYMS
DH: District hospitals
GA: general anaesthesia
IMF: intermaxillary fixation -reduction of fractured jaws
OHS: Oral Health Services
POH: Public Oral Health
PHC : Primary Health Care
References
1. Bhayat A. Maxillofacial referral patterns from Primary Oral Health Care facilities to tertiary institutions in Gauteng (January 2009- July 2009); Unpublished Report. 2010. [ Links ]
2. Pau A, Nanjappa S, Diu S. Evaluation of dental practitioners with special interest in minor oral surgery. British Dental Journal. 2010; 208(3):103-7. [ Links ]
3. Norms, Standards and Practice Guidelines for Primary Oral Health Care. 2005. Available on: http://www0.sun.ac.za/rural-health/ukwandahome/rudasaresources2009/DOH/part1.pdf [Accessed: 10/11/14] [ Links ]
4. Myburgh N, Hobdell M, Lalloo R. African countries propose a regional oral health strategy: The Dakar Report from 1998. Oral Disease. 2004; 10:129-37. [ Links ]
5. Hobdell M, Myburgh N, Lalloo R, Chikte U, Owen P. Oral disease in Africa: a challenge to change oral health priorities. Oral Disease. 1997; 3: 216-22. [ Links ]
6. A District Hospital Package for South Africa: A set of norms and standards. 2002. http://www.kznhealth.gov.za/norms.pdf [Accessed: 10/11/14] [ Links ]
7. A Regional Hospital Service Package for South Africa: A draft proposal. 2002. Available on: http://www0.sun.ac.za/ruralhealth/ukwandahome/rudasaresources2009/DOH/DRAFT%20DIS-TRICT%20HOSPITAL%20PACKAGE.pdf [Accessed: 15/11/14] [ Links ]
8. Department of Health (2004). Revised South African National Oral Health Strategy Draft (2010). Available on: www.doh.gov.za. [ Links ][Accessed: 27/11/14]
9. Yiu CKY, McGrath C, Bridges S, Corbet EF, Botelho MG, Dyson JE and Chan LK. Self-perceived preparedness for dental practice amongst graduates of The University of Hong Kong's integrated PBL dental curriculum. Eur J Dent Educ. 2012; 16: e96-e105. [ Links ]
10. Simon AK, Rao A, Rajesh G, Shenoy R, and Pai MB. Oral health care availability in Health Centers of Mangalore Taluk, India. Indian J Community Med. 2014; 39(4): 218-22. [ Links ]
11. Coulthard P, Bailey E, Esposito M, Furness S, Renton TF, Wor-thington HV. Surgical techniques for the removal of mandibular wisdom teeth. Cochrane Database Syst Rev. 2014; 29. [ Links ]
12. Diamanti N, Duxbury AJ, Ariyaratnam S, Macfarlane TV. Attitudes to biopsy procedures in general dental practice. British Dental Journal. 2002; 192: 588 - 92. [ Links ]
13. Naidoo S, Van A. Vulnerability of children to gunshot trauma in violence-prone environment: the case of South Africa. 2011; 8(1): 101-4. [ Links ]
 Correspondence:
Correspondence:
M Mabongo
Specialist in Maxillofacial and Oral Surgery, Department of Maxillofacial and Oral Surgery
School of Oral Health Sciences, Faculty of Health Sciences, University of Witwatersrand
7 York Road, Parktown, 2193
Tel: 011 717 2243
E-mail:mzubanzi.mabongo@wits.ac.za













