Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.70 no.10 Johannesburg Nov. 2015
RESEARCH
Oral health and subjective psychological well-being among South African Adults: Findings from a national household survey
OA Ayo-YusufI; P MotlobaII; IJ Ayo-YusufIII
IBDS, MSc, DHSM, MPH, PhD. Professor & Director, Sefako Makgatho Health Sciences University
IIBDS, MPH, MDent, MBL. Senior Lecturer & Head, Department of Community Dentistry, Sefako Makgatho Health Sciences University
IIIBDS, MSc, PhD. Senior Lecturer, Department of Dental Management Sciences, University of Pretoria
ABSTRACT
OBJECTIVE: To determine the association between oral health and socioeconomic status with subjective psychological well-being.
METHODS: An interviewer-administered questionnaire was conducted during 2011 on a nationally representative sample of South African adults >16 years (n=2,971) who reported on socio-demographic data, past dental visit patterns, number of remaining teeth and oral and general health status. Subjective well-being was computed as the sum of scores obtained from participants' estimates of level of happiness (scale 0-6) and rating of level of satisfaction with life (scale 0-4). Analyses included t-tests and multivariable-adjusted Poisson regression.
RESULTS: The average score on a scale of 0-10 for subjective well-being was 6.31 (95%CI=6.17-6.44), which decreased with age, but increased with level of education and frequency of dental visits. Even after controlling for socioeconomic status, those who rated their oral health as good were more likely to report a higher subjective well-being (Prevalence Rate ratio (PRR) =1.14; 95% CI=1.03-1.27). Those who reported visiting a dentist at least every 6 months reported higher subjective well-being (PRR=1.10; 1.04-1.16.
CONCLUSIONS: Good oral health is independently associated with greater subjective well-being. This highlights the need to prioritise oral health promotion as an integral part of promoting general health and improving the quality of life of South Africans.
INTRODUCTION
Although chronic diseases and disability are associated with unsatisfactory health outcomes, those affected may still be leading fruitful and productive lives.1 Conversely, those with predictable normative health outcomes may indicate subjective reduction in satisfaction about life and/or an unhappi-ness.2 Accordingly, individuals' health care needs would be better managed if the subjective or self-perceived health outcomes of the patient are integrated with clinical practice.
The concept of health related quality of life (HRQoL), remains a well-established framework for assessment of subjective health outcomes.3-5 This framework is useful as it recognises health to be a multidimensional concept; thereby providing the impetus to move beyond normative domains like survival, the illness and impairment that may result from dental caries or missing teeth, and move to include functional and psychosocial domains in the planning and evaluation of health care.6
Numerous studies have demonstrated an association between physical activity7, daily intake of fruits and vegeta-bles8, and oral conditions and functional and social well-being as measured by levels of happiness.9,10 However, according to Piqueras et al8, subjective well-being which is an evaluative reaction of a person to his/her life, has two components, namely the cognitive component (i.e. cognitive evaluation of life satisfaction) and an affective component (such as happiness). Yet, the limited number of studies on the association between oral health and psychological well-being has focused mainly on the affective component - happiness.
Considering that no study to date has evaluated the association between oral health and subjective well-being among adults in South Africa in particular, and in Africa in general, this study sought to determine that association as measured by both level of happiness and perceived level of satisfaction with life. Furthermore, considering that the individual's socioeconomic position can conceivably influence oral health and subjective well-being, this study also examined the role of socioeconomic status as the mediator of the effect of oral health on subjective well-being.
METHODS
Data source
This analysis was based on the 2011 South African Social Attitude Survey (SASAS), which is a nationally representative household interviewer-administered questionnaire survey. The SASAS is conducted annually by the Human Sciences Research Council. This study is part of a larger study to investigate the effect of socioeconomic position on oral health-related quality of life by including questions additional to the questionnaire of the 2011 SASAS. The target population of SASAS includes non-institutionalised South African adults aged 16 years and older. The SASAS used a multi-stage probability sampling strategy with census enumeration areas as the primary sampling unit. Sampling involved stratification by socio-demographic domain for each province and geographical subtypes, namely tribal areas, formal rural, formal urban and informal urban. This stratification was designed to ensure sufficient geographical distribution across all nine provinces, and adequate distribution between South Africa's four ethnic/race groups as currently used in the South African population census, namely: self-identifying as Black African; Coloured; Indian or Asian; or White. The Human Sciences Research Council granted ethical clearance for this survey.
Outcome measures
Subjective well-being (SW) was measured using two items. Considering that previous studies have demonstrated the validity of a single-item life satisfaction measure and found this to be comparable with multiple-item measures11, life satisfaction in this study was measured with the single-item : 'How satisfied are you with your life as a whole these days?'. Responses were coded on a scale from 0 to 4, ranging from 'very dissatisfied' to 'very satisfied'. The other measure for SW was based on the question: 'If you were to consider your life in general these days, how happy or unhappy would you say you are, on the whole?' Responses were coded on a scale from 0 to 6, ranging from 'completely unhappy' to 'completely happy'. Subjective well-being was computed as a sum of the scores on both items with the possible score ranging between 0 and 10.
Independent variables
Self-reported oral health and general health status were considered the main predictor variables. Self-reported health is considered the individual's personal evaluation of their (oral) health, integrating all aspects of (oral) health, including physical, social and functional aspects. The validity of these constructs has been demonstrated in previous studies.11 Self-reported general health was determined by the response of the study participants to a five scale question, 'In general, would you say your health is.... [This refers to both physical and mental health]. Would you say it is poor (coded 0), fair (1), good (3), very good (4) or excellent (5)'? The response options we collapsed into three categories of self-rated general health, namely 0 for poor, 1 for fair and 2 for good, very good or excellent. Similarly, self-rated oral health was determined by a response to a five scale question, 'How would you rate your oral health? Response options included 'very poor' (0), 'poor' (1), 'neither nor' (3), 'good' (4), 'very good' (5). We also collapsed these options to form three outcomes of self-rated oral health: 0 for very poor or poor, 1 for neither nor and 2 for good or very good.
We further considered key individual demographic markers (age, sex, race, marital status) as predictors in our analysis. Information on the participants' province and place of residence (rural, urban formal or urban informal area) as well as socioeconomic position was obtained using the questionnaire. Two different measures of socioeconomic position were used, namely the respondents' highest level of educational attainment (<grade 12; grade 12; >grade 12) and subjective socioeconomic position. The latter was measured using a ten scale question: 'In our society, there are groups which tend to be towards the top and groups which tend to be towards the bottom. Below is a scale that runs from top to the bottom. Where would you put yourself on this scale?' Responses were coded from 1 to 10, ranging from the 'Top' to the 'Bottom' of the scale.
In order to measure pain experience from common oral conditions, the respondents answered 'Yes or No' to the question asking if in the last six months they had experienced pain from the teeth or gums. Furthermore, dental care behaviour was measure by the question: 'How often do you visit a dentist or dental clinic?' Responses were categorised as 0 for never, 1 for only when in pain or whenever needed, 2 for once every 2 years, 3 for once a year and 4 for once every 6 months.
Data analysis
Factor analysis using the principal component analysis was applied to develop the subjective well-being measure and Cronbach's alpha was used to determine the reliability of the two-item subjective well-being scale. Construct validity of the subjective well-being scale was determined by exploring the association between self-reported general health and subjective well-being, as it was expected that self-reported general health would to be associated with subjective well-being.
Descriptive (median, mean and 95% confidence intervals) and bivariate statistics were employed to study the distribution of subjective well-being according to sociodemo-graphic and self-reported oral health behaviour and condition. The conceptual framework introduced by Baron and Kenny12 was used for testing the mediation effect of socioeconomic variables. True mediation occurs when both the predictor and mediator are associated with the outcome, the predictor is associated with the mediator, and the association between the predictor and the outcome is attenuated by the mediator.
As the outcome (subjective well-being) was a count variable, a multi-variable adjusted Poisson regression was used to test the independent association between the predictors and the outcome. Using purposeful selection, two separate models were constructed, namely one without the two socioeconomic potential mediator variables and the other with the two socioeconomic variables. The latter model allowed us to observe any attenuation in the magnitude of the association between the predictor variables and the outcome. All variables with P<0.25 were kept in the final model. All statistical tests performed using STATA version 12, took into account the complex sampling employed in SASAS and estimates provided were weighted in respect of the response pattern and the need to keep the national representation of the study sample. All statistical tests were two-tailed and the level of statistical significance was set at p<0.05.

RESULTS
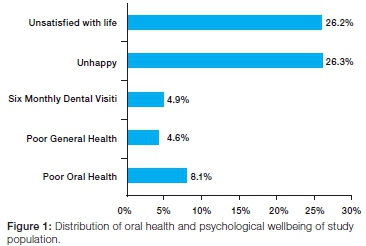
The study participants, as expected, were representative of the national socio-demographic distribution namely that respondents predominately self-identified as black Africans (76.7%), female (52.5%), resident in the formal or informal urban areas (64.7%), and having achieved lower than grade 12 level of education (55.9%). In general, 4.6% reported poor general health, 8.1% poor oral health, 5.7% reported being edentulous and only 4.9% reported 6-monthly routine preventive dental visits (Figure 1), which translates to weighted counts of 1,546,798, 2,690,509, 1,904,272 and 1,620,071 people respectively. Of the study participants, 26.3% (weighted count = 8,784,535) reported being not happy and 26.3% (weighted count=8,750,029) reported not being satisfied with their life in general. Compared with those reporting being satisfied with their life, significantly more of those who reported not being satisfied with their life reported being unhappy (16.3% vs. 54.7%; p<0.001).
The two-item measure of subjective well-being was found reliable as demonstrated by a satisfactory internal consistency (Cronbach's alpha = 0.68). Proportion of those who reported being completely/fairly happy was highest among those who reported good oral health (77.2%), good general health (78.2%), 6 monthly dental visits (90.9%), having all/most of their teeth (84.7%), residing in formal urban areas (81.7%), self-identified as white (91.9%), male (72.3%), had greater than grade 12 education (92.7%). There were significant differences in the reported levels of happiness across provinces with the highest proportion of those reporting being completely/ fairly happy being in the Western Cape (87.3%) and the lowest being in the Eastern Cape Province (59.9%) (Data not shown). Similarly, the mean scores for subjective psychological wellbeing based on a scale of 0 to 10, was highest among those reporting good oral health, good general health, 6 monthly visits, formal urban residents, self-identifying as white, being male and having greater than grade 12 (Table 2).
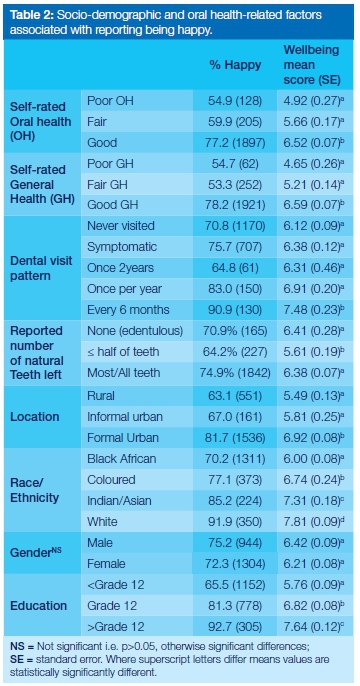
Unadjusted Poisson regression showed a significant association between higher subjective wellbeing and reported good oral health status, good general health, one year and six monthly preventive dental visits, formal urban residence, higher level of education, self-identifying as white and reporting higher subjective socioeconomic position (Table 2). Following adjustment for socioeconomic status, age and provincial variations, although the prevalence rate ratios became attenuated, reporting good oral health (PRR=1.12; 1.01-1.24) and good general health (PRR=1.19; 1.07-1.37) remained significantly associated with better psychological wellbeing as compared with reporting poor oral health and poor general health. Furthermore, as compared with having never visited a dentist, only making preventive dental visits every six months was associated with better psychological wellbeing (PRR=1.08; 1.01-1.14) (Table 3). Race/ethnicity completely lost statistical significance in an adjusted regression model, suggesting that race/ethnic differences were completely mediated by socio-economic differences among the racial groupings. The estimated number of teeth reported missing or present was also no longer significantly associated with wellbeing after controlling for socio-economic position.

DISCUSSION
The findings of this study suggest that there were almost twice as many people who reported poor oral health as there were people who reported poor general health. Furthermore, that subjective psychological wellbeing is independently influenced by self-reported oral and general health status, dental visit, place of residence, education and socioeconomic status. This study also showed that a substantial number of those who reported being unsatisfied with their life still reported being happy, confirming that these are two different constructs of subjective well-being.
The finding that good oral health is a significant predictor of better psychological wellbeing among South Africans is consistent with results from similar studies that have shown that dental pain, untreated caries, edentulism, inability to chew, malocclusion etc. impact on social interactions, influence happiness, and impact on the quality of life.8, 13-16 Operating through the psychological pathway, oral health therefore seems to have an independent influence on subjective wellbeing in various settings.14,17
Remarkably, subjective assessment of oral health as opposed to the objective assessment such as physical absence of teeth had greater impact on the psychological wellbeing of South African adults. This has also been observed in several other studies in a variety of settings and supports the call for a shift from traditionally
normative assessment of care to a patient-centered centred clinical care.5, 18, 19 Patients' global assessment of their oral health would indeed not only be related to the absence or presence of oral disease but may also include perception of dental appearance and the extent that this may influence social interaction. Those who perceive their oral health as poor, would conceivably feel less happy, less satisfied with life and thus have poor subjective wellbeing. Perceived poor oral health, particularly among those of low SES who might not be able to afford regular routine preventive dental visits or afford to have prosthetic replacements for missing teeth, may therefore impose additional psychosocial burden resulting in further decline in the wellbeing and quality of life of individuals.9, 10, 13
This study like other similar studies is prone to cross-sectional design limitations, despite being nationally representative. Hence the study findings should be interpreted cautiously, given that direction of causal relation cannot be accurately determined without evidence of the temporal order of events. For instance, it is not known if participants had been unhappy and unsatisfied with life before developing poor oral health as opposed to the other way round. Noticeably, properly designed longitudinal studies are necessary to evaluate the temporal effects on perception of oral health on subjective wellbeing. This study nevertheless draws the attention of oral health practitioners to the fact that perceived poor oral health, reduced levels of happiness, dissatisfaction with life and thus poorer psychological wellbeing may coexist within different strata of South African population, particularly among already vulnerable groups. These vulnerable subgroups include those living in the rural or informal areas, less educated (< grade 12), and having had infrequent or no dental visit in the last two years. Poor oral health therefore has the potential to worsen inequality in health and wellbeing in South Africa, thus the need for Government to prioritise interventions to improve oral health among the identified vulnerable groups in this study.
CONCLUSIONS
Good oral health status is associated with better subjective psychological wellbeing independent of socioeconomic status. This study's findings also highlight the need to consider subjective wellbeing as an important outcome in oral health interventions or oral health policy outcomes.20,21 Therefore, in planning future healthcare services such as that envisaged within the National Health Insurance (NHI) scheme, health care outcomes should go beyond clinical measures of disease but should incorporate improved subjective wellbeing. Finally, this study's findings highlight the need to incorporate oral health promotion in all interventions to improve general health and the quality of life of South Africans.
Conflict of interest: None declared
ACRONYMS
HRQoL: Health related quality of life
PRR: Prevalence rate ratio
SASAS: South African Social Attitude Survey
SW: Subjective well-being
References
1. Fellinghauer B, Reinhardt JD, Stucki G, Bickenbach J. Explaining the disability paradox: a cross-sectional analysis of the Swiss general population. BMC Public Health. 2012; 12(1):655. [ Links ]
2. Albrecht GL, Devlieger PJ. The disability paradox: high quality of life against all odds. Social Science & Medicine. 1999; 48(8):977-88. [ Links ]
3. Locker D. Measuring oral health: a conceptual framework. Community Dental Health. 1988; 5(1):3-18. [ Links ]
4. Moons P, Budts W, De Geest S. Critique on the conceptualisation of quality of life: a review and evaluation of different conceptual approaches. International Journal of Nursing Studies. 2006; 43(7):891-901. [ Links ]
5. Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life: a conceptual model of patient outcomes. The Journal of the American Dental Association. 1995; 273(1):59-65. [ Links ]
6. Cushing A, Sheiham A, Maizels J. Developing socio-dental indicators--the social impact of dental disease. Community Dental Health. 1986(3):3-17. [ Links ]
7. Richards J, Jiang X, Kelly P, Chau J, Bauman A, Ding D. Don't worry, be happy: cross-sectional associations between physical activity and happiness in 15 European countries. BMC Public Health. 2015; 15(1):53. [ Links ]
8. Piqueras JA, Kuhne W, Vera-Villarroel P, van Straten A, Cui-jpers P. Happiness and health behaviours in Chilean college students: a cross-sectional survey. BMC Public Health. 2011;11(1):443. [ Links ]
9. Dumitrescu AL, Kawamura M, Dogaru BC, Dogaru CD. Relation of achievement motives, satisfaction with life, happiness and oral health in Romanian university students. Oral Health & Preventive Dentistry. 2009; 8(1):15-22. [ Links ]
10. Ide R, Hoshuyama T, Wilson D, Takahashi K, Higashi T. Association of psychological well-being with oral conditions in Japanese workers. Journal of Occupational Health. 2006; 48(6):487-93. [ Links ]
11. Cheung F, Lucas RE. Assessing the validity of single-item life satisfaction measures: results from three large samples. Quality of Life Research. 2014; 23(10):2809-18. [ Links ]
12. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986; 51(6):1173. [ Links ]
13. Kandelman D, Petersen PE, Ueda H. Oral health, general health, and quality of life in older people. Special Care in Dentistry. 2008; 28(6):224-36. [ Links ]
14. Scapini A, Feldens CA, Ardenghi TM, Kramer PF. Malocclu-sion impacts adolescents' oral health-related quality of life. The Angle Orthodontist. 2012; 83(3):512-8. [ Links ]
15. Yoon HS, Kim HY, Patton LL, Chun JH, Bae KH, Lee MO. Happiness, subjective and objective oral health status, and oral health behaviours among Korean elders. Community Dentistry and Oral Epidemiology. 2013; 41(5):459-65. [ Links ]
16. Strauss RP, Hunt RJ. Understanding the value of teeth to older adults: influences on the quality of life. The Journal of the American Dental Association. 1993; 124(1):105-10. [ Links ]
17. Tuchtenhagen S, Bresolin CR, Tomazoni F, et al. The influence of normative and subjective oral health status on schoolchil-dren's happiness. BMC Oral Health. 2015; 15(1):15. [ Links ]
18. Locker D, Miller Y. Evaluation of subjective oral health status indicators. Journal of Public Health Dentistry. 1994; 54(3):167-76. [ Links ]
19. Lyubomirsky S, Lepper HS. A measure of subjective happiness: Preliminary reliability and construct validation. Social Indicators Research. 1999; 46(2):137-55. [ Links ]
20. Sischo L, Broder H. Oral Health-related Quality of Life - What, Why, How, and Future Implications. Journal of Dental Research 2011; 90(11):1264-70. [ Links ]
21. Carr AJ, Higginson IJ. Measuring quality of life: Are quality of life measures patient centred? British Medical Journal. 2001; 322(7298):1357. [ Links ]
 Correspondence:
Correspondence:
OA Ayo-Yusuf
Sefako Makgatho Health Sciences University
P. O. Box D12, Medunsa 0204
E-mail: lekan.ayo-yusuf@smu.ac.za













