Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.70 n.9 Johannesburg Oct. 2015
RESEARCH
Fracture behaviour patterns of cusp-replacing fibre strengthened composite restorations
HJ VisserI; PD BrandtII; FA de WetIII
IBChD (Pret) BChD Hons (Pret). MSc Odont student, Department of Odontology, School of Dentistry, University of Pretoria
IIBChD (Stell), PGDipDent (Aesthetic Dentistry, Stell), MSc Odont (Pret). Senior Lecturer, Department of Odontology, School of Dentistry, University of Pretoria
IIIBChD (Pret), BChD Hons (Pret), MDent (Pret), UED (Pret), DSc (Pret). Professor and Head, Department of Odontology, School of Dentistry, University of Pretoria
ABSTRACT
OBJECTIVES: To investigate and compare, in vitro, the fracture behaviours of three types of cusp-replacing posterior composite resin restorations.
METHODS: Standard preparations for posterior composite restoration of the mesio-lingual cusp were cut on seventy-five extracted lower left first and second molars and restorations placed. Group A (control, n =25) with a conventional posterior composite resin, Group B (n=25): resin reinforced with nano-scale electrospun glass fibres Group C (n=25) :resin reinforced with a fibre substructure. Specimens were thermocycled for 500 cycles between 5°C and 55°C with a dwell time of 30 seconds, then embedded in plastic cylinders in acrylic resin. The specimens were loaded in a universal testing machine at a 30° angle to the long axis of the tooth until fracture occurred. Fracture patterns were highlighted by staining, studied under a microscope and classified as favourable (restorable) or unfavourable (non-restorable). Sub-classification included adhesive and cohesive failures.
RESULTS: Group C exhibited significantly more "restorable" fractures. Group B displayed significantly more "non-restorable" fractures. Fracture patterns differed significantly between the two fibre-strengthening techniques. (Fisher's Exact Test p = 0.05.
CLINICAL SIGNIFICANCE: Resin restorations reinforced with glass-fibre substructures are more readily repaired after fracture, saving tooth structure, and reducing costs to the patient.
Keywords: glass-fibre reinforcement, posterior composite resin restorations, fracture patterns
INTRODUCTION
This article reports further on the research originally published in the 2014 SADJ Vol 69 p202-p207, and compares and discusses various fracture patterns in failed posterior composite restorations. Many different treatment modalities are available when restoring a tooth that has lost one or more cusps.1,2,3 Although all of these protocols have proven track records, they are mostly costly, technique sensitive and often involve the services of a dental technician.2,4,5 In rural areas these services are often not available, resulting in a large section of the population not being treated. This leads to the eventual loss of restorable teeth. This research project investigated a more affordable direct composite technique.
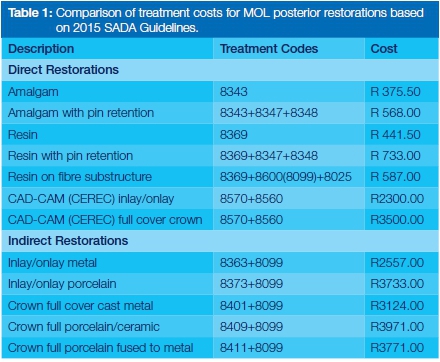
Conventional methods to restore teeth with cusp-replacing restorations include direct and indirect composite restorations, direct or indirect metal inlays/overlays, ceramic inlays/overlays and in some cases full-coverage gold/ceramic crowns.6 Based on 2015 dental tariffs and including all laboratory fees if applicable, the relative costs were calculated in ZAR (Table 1). Whilst costs are lower, fracture of the composite material in the posterior region is a common reason for failure, particularly within the first five years.6,7,8
Judging from the number of failures recorded with the use of direct composite techniques to repair posterior cavities, including restoring lost cusps, it became clear that significant improvements in the mechanical properties of dental composite resins were needed in order to extend the use of these materials to these large stress-bearing applications.6,9,10 Their use in larger posterior restorations involving cusp replacement is further severely limited by the low flexural strength of composites.10 Furthermore, a restored tooth tends to transfer stresses differently than an intact tooth. Adhesive restorations transfer and distribute functional stresses across the bonding surface and also reinforce weakened tooth structure.9 SEM analysis of dental restorations confirmed clinical observations that composite resin restorations are prone to bulk fracture with crack propagation rates higher than those of porcelain.2,11,12 Finite element analysis showed that during mastication the inner side of the restoration can be in maximum tension,13 leading to fracture initiation.14
Extensive studies have therefore been undertaken on methods of improving and reinforcing the mechanical properties of these composite resins such as adding ceramic and porous fillers,3,7,15 optimizing the filler levels3,7 and/or using micro scale-glass-fibres as fillers, as found in Aelite (BISCO, Schaumberg, Illinois, USA).16-18
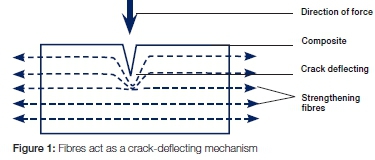
It has been proven in various research projects1,315 that fibre reinforcement of composite resin strengthens the composite resin material.6,18-20 Recent research studies found that using fibre-reinforced composite as a substructure under composite restorations can improve the load-bearing capacity and may offer one alternative in overcoming some potential problems of composite restorations in high stress-bearing areas.7,16-20 (Figure 1)
The location of the strengthening fibres is very important in the performance of the fibre-composite combination. It was found that tension side reinforcement was most effective in increasing the flexural strength as well as the static load-bearing capacity of dental restorations.3,20
However, some studies suggest that the incorporation of fibres not only increases the static load-bearing capacity of cusp-replacing restorations, but also has a beneficial effect on the failure mode and thereby on the restorability after fracture.15,21-23
The fibres may act as a crack-deflecting mechanism (Figure 1), changing the fracture behaviour of the composite resin material to that of a material with quasi-ductile fracture behaviour.6,19,22,24
AIM
The aim of this in vitro blind study was to examine and compare the fracture behaviour (fracture patterns) of a conventional posterior composite (QuiXfill, Dentsply, Kon-stantz, Germany) used as the Control Group, a posterior composite resin incorporating micro-scale glass-fibres as fillers (Aelite, BISCO, Schaumberg, Illinois, USA) (Group B) and a conventional posterior composite (QuiXfill) placed on a fibre sub-structure (everStick Crown and Bridge, Stick Tech Ltd, Turku, Finland) (Group C).
MATERIALS AND METHODS
Specimen selection and preparation
Seventy-five intact, human lower left first and second molars were collected and stored in an aqueous solution of 5% chlorhexidine (C22H30Cl2N10) at +8°C in a refrigera-tor.25-27 Informed consent for the use of the teeth for research purposes was obtained from all donors during the registration of the patient at the Oral and Dental Hospital, University of Pretoria. The specimens were selected to ensure anatomical consistency (i.e. tooth size, occlu-sal area, configuration of the fissures, etc.) in order that a standardized mesio-occlusal-lingual (MOL) cavity could be prepared. The teeth were all sound and had been extracted for reasons of periodontal disease. The donors were all aged between 50 and 70.
The preparation was standardized as follows: The cemen-to-enamel junction (CEJ) was located by visual examination. The mesio-lingual cusp was removed to a level one mm occlusal of the CEJ. A standardized MOL cavity was prepared using a number 142, size 018, dome-shaped diamond fissure bur in an air-rotor handpiece and under continuous water spray. All internal line angles were rounded. A proximal step of a depth of one mm was prepared, respecting the position of the CEJ. The width of the proximal box was determined by the occlusal anatomy of the specific tooth - the mesio-occlusal fissure was incorporated into the preparation as well as the mesio-lingual cusp. Each preparation was performed by one operator and examined for the correct dimensions by a second operator. If the preparation did not conform to the specified dimensions, the preparation was corrected (if possible); otherwise the tooth was removed from the experiment and replaced by another. The dimensions of each preparation were recorded.
The specimens were now randomly divided into three groups:
Group A: Conventional Posterior Composite - Control (n=25)
All enamel margins were bevelled. The specimens were etched with 37% phosphoric acid as follows: all enamel margins for 15 seconds, then all the exposed dentine (together with the enamel) for 10 seconds (selective etching technique). The acid was washed off with water. Care was taken to ensure that all acid was removed. The specimens were then lightly air-dried, ensuring that all dentine surfaces remained slightly moist. A bonding agent (XP Bond, Dentsply, Konstanz, Germany) was applied and light-cured, according to the manufacturer's instructions. A Tofflemire matrix band was placed according to the manufacturer's instructions.28-30
Specimens in group A received a conventionally-filled composite resin (QuiXfill, Dentsply, Konstanz, Germany) restoration, placed according to the manufacturer's instructions and using an oblique layering technique with incremental layers not exceeding 2mm. After the restoration was placed, it was polished using Shofu 411 diamond burs (Shofu Inc., Kyoto. Japan) and Enhance Polishing System (Dentsply, Konstanz, Germany).
Group B: Posterior composite resin incorporating micro-scale glass fibres (n=25)
Exactly the same technique was used as in Group A, except that the restorative material was a posterior composite resin restoration incorporating micro-scale glass-fibres as fillers (Aelite, BISCO, Schaumberg, Illinois, USA).
Group C: Posterior composite resin placed on a fibre sub-structure (n=25)
Exactly the same technique was used as for Groups A and B, including the placement of a Tofflemire matrix band. The inter-proximal step was then filled with a conventionally-filled composite resin (QuiXfill) restoration and light-cured according to the manufacturer's instructions.
A glass-fibre bundle (everStick Crown and Bridge, Stick Tech Ltd, Turku, Finland) was placed on the occlusal surface across the area of the missing cusp. The glass-fibre bundle was secured in position with a flowable composite (Esthet-Xflow, Dentsply, Konstanz, Germany). This acts as a luting cement, ensuring that no air bubbles are trapped between the fibre bundle and the bonded tooth surface and was placed according to the manufacturer's instructions (Stick Tech Ltd, Turku, Finland). Close contact between the fibre bundle and the floor of the cavity was ensured by means of a silicone refix forming aid. The glass-fibre bundle was light-cured according to the manufacturer's instructions. Specimens in Group C now received a conventionally-filled composite resin (QuiXfill) restoration, placed according to the manufacturer's instructions and using an oblique layering technique with incremental layers not exceeding 2mm. After the restoration was placed it was polished using Shofu 411 diamond burs (Shofu Inc., Kyoto. Japan) and Enhance Polishing System (Dentsply, Konstanz, Germany).
All specimens were embedded in an acrylic resin cylinder (20mm diameter, height 20mm) with the CEJ approximately 1.5mm above the acrylic, which simulated the bone level. The cylinders were marked to distinguish the groups. All specimens were stored in saline25,31,32 and subjected to thermocycling (500 cycles between 5° and 55° centigrade with a dwell time of 30 seconds).33
Testing: Specimens were then stored in saline (isotonic NaCl aqua solution, 9% by volume) for a minimum of 24hrs before testing. Each was sequentially fixed in a metal holder and positioned, using a specially made jig, in a universal testing machine (TestXpert V 11.02 Zwick 1446, Zwick Roell, Epental, Germany) with the long axis of the roots at an angle of 30 degrees to the direction of the load.34,35 The site of loading was the central fissure of the occlusal surface in the direction of the mesio-lingual cusp. A stainless steel cylindrical rod (tip diameter of 2mm)33 was used with a crosshead speed of 0.5 mm/ min32,33 to load the specimens until fracture occurred. The force needed to fracture the tooth was recorded on a PC. Testing of specimens was done randomly by an independent operator who did not know to which group each specimen belonged. Individual specimen numbers were allocated as the tests were being done. The part of the specimen that fractured off was collected, mounted on a transparent sheet and numbered for later investigation.
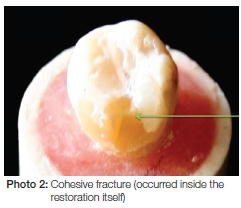
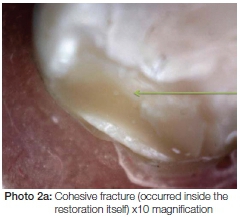
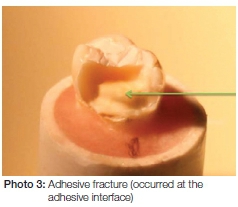
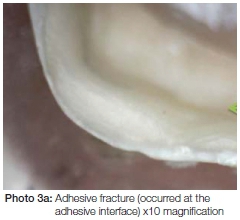
After testing, the fractured specimens were stored for 24 hours immersed in India ink35,37 according to standardized protocols38 in order to highlight the fracture lines. The failure modes were evaluated by two observers both visually and microscopically, using a stereo microscope at 10x magnification.
RESULTS
Table 2 gives the collated results on the fracture patterns. The results are explored in more detail as part of the Discussion. (Annexure 1, Table 2)
For fracture behaviour patterns, the groups were analysed in a contingency table using Fisher's exact test. All testing were evaluated at the 0.05 level of significance.
DISCUSSION
Results of research have to be interpreted with care, even more so when biological material is investigated.39 It is just not possible to control all variables, therefore specimens were carefully selected using anatomical criteria, age of the patient and position in the mandible. However, factors that might influence dentine bonding such as sclerotic dentine and dead dentinal tracts could not be controlled. On the other hand, sample size, tooth preparation, placement technique, specimen preparation, testing and analysis of results were easily standardized. Chlorhexidine25-27 might not have been the best liquid in which to store the extracted teeth because of risks such as staining of the specimens and the possible effect on dentine bonding. These considerations were deemed beyond the scope of this article, which has focussed on fracture patterns. Likewise, storing the specimens (after preparation, placing of the restoration and thermocycling) in saline instead of artificial saliva might be questioned by some researchers. However, the authors are of the opinion that there probably would not have influenced the fracture patterns. Saline for storage of teeth has been chosen by many researchers.25,31,32,39 It seems that, according to the literature, many researchers prefer to store the prepared specimens in distilled water prior to testing.34,40-42 Raum (2007) recommended storage in artificial saliva;43 Kitasako (2000) concluded that there is no difference between storage in distilled water and saline,44 while Jaffer (2009) observed that dry storage or storage in ethanol is not recommended because of desiccation.45
It would have been ideal to perform the loading tests during thermocycling, but this was found to be logistically impossible. Again, any effect on the fracture patterns is questionable.
Fracture Patterns
Fracture patterns are broadly classified in the literature as either restorable (fractures above the simulated bone crest) and non-restorable (fractures below the simulated bone crest).35,36,46
Fractures which were restorable occurred in 44% of cases (11 of 25 specimens) in Group A (control - QuiXfill ), in 12% (3 of 25 specimens) in Group B (Aelite and nano-scale glass fibre reinforcement) and in 84% (21 of 25 specimens) in Group C (QuiXfill placed on everStick ). (Graph 1) These data differences were statistically significant (Fishers Exact Test, p < 0.05)

Fennis et al found that composite resin restorations placed on bi-directional fibre netting fractured in a favourable (restorable) way in 62% of specimens.47 In comparison, when composite resin restorations were placed on a unidirectional fibre sub-structure 77% specimens fractured in a favourable manner (restorable). Studies by Akman et al, 2011 and by Lammi et al 2011 also showed that if a multi-directional substructure were used, 66% -80% of fractures were favourable (restorable).47-49,50
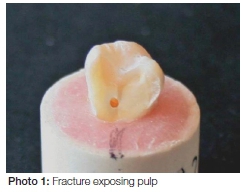
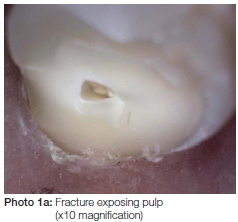
The composite resin reinforced with nano-scale glass fibre reinforcement (Group B - Aelite) fractured in 28% of cases (7 out of 25) in such a manner that pulp tissue was exposed. (Photos 1 and 1a). This was the only group in this study in which pulp-exposing fractures occurred. These catastrophic type of fractures have also been reported to occur when conventionally-filled composite resin was placed on a substructure of short multi-directional fibre composite.23
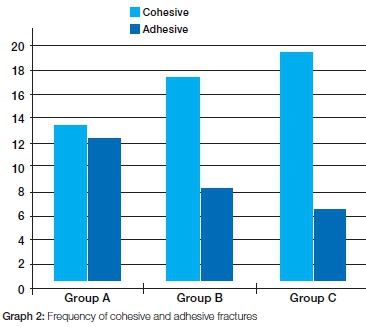
According to the literature35,36,42 some researchers also use a broad classification system based on the type of fracture, being either cohesive or adhesive. (Photos 2 and 2a). A more detailed investigation of fracture patterns in the current study (Graph 2) show that in Group A, the fractures were more or less evenly distributed between cohesive and adhesive types (Graph 2). 52% or 13 out of 25 specimens were cohesive fractures (Photo 3 and 3a). This differs from the finding of Taha (2011)51 who found mainly adhesive fractures. In Group B most of the fractures were cohesive (68%, 17 out of 25 specimens), while in Group C 76% (19 out of 25) of fractures were cohesive, and 16% (4 out of 25 specimens) of fractures were adhesive. This is similar to the finding of Tezvargil (2005).49 In all 76% of cohesive failures the fracture occurred between the fibre substructure and the composite resin as illustrated in Photo's 4 and 4 (a).
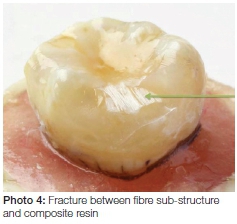
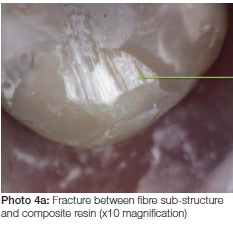
The superior performance of Group C seems to support the hypothesis that the fibre substructure acts as a crack-deflecting mechanism, enabling the composite resin restoration to endure significantly higher forces before fracture.18-20,23 It is speculated that the absence of a uni-directional fibre substructure might be the reason for the fractures that occurred in Group B in such a manner that the pulp was exposed. This speculation is supported by a recent publication by Frater et al, 2014.23
CONCLUSION
Analysis of fracture patterns in this study identify statistically significant differences between the three restoration groups studied. The conventionally-filled composite placed on a uni-directional fibre substructure showed the most favourable (restorable) fracture pattern; with the composite restoration incorporating nano-scale glass-fillers showing the least favourable fracture pattern.
It can therefore be concluded that placing a fibre substructure underneath a conventionally filled composite restoration will enhance the 'restorability' of the fracture pattern and ultimately may thereby extend the life-span of the restored tooth.
Declaration: Dr HJ Visser is the co-owner of a Dental Company (Stick Bond Dental CC) which imports one of the key products.
ACRONYM
CEJ: cemento-enamel junction
MOL: mesio-occlusal-lingual
References
1. Kim SH, Watts DC. Effect of glass-fiber reinforcement and water storage on fracture toughness (KIC) of polymer-based provisional crown and FPD materials. Int J Prosthodont 2004; 17: 318-22. [ Links ]
2. Garoushi S, Lassila LV, Tezvergil, Vallittu PK. Static and fatigue compression test for particulate filler composite resin with fiber reinforced composite substructure. Dent Mater 2007; 23(1):17-23. [ Links ]
3. Garoushi S, Mangoushi E, Vallittu PK, Lassila LV. Short fiber reinforced composite: a new alternative for direct onlay restorations. Open Dent J 2013:7:181-5 [ Links ]
4. Baran G, Boberick K, McCool J. Fatigue of restorative materials. Crit Rev Oral Biol Med 2001; 12(4): 350-60. [ Links ]
5. Fennis WM, Kuijs RH, Roeters FJ, Creugers NH, Kreulen CM. Randomized control trial of composite cuspal restorations: five-year results. J Dent Res 2013; 93(1) 36-41. [ Links ]
6. Garoushi S, Tanner J, Vallittu PK, Lassila LV. Preliminary clinical evaluation of short fiber-reinforced composite in posterior teeth: 12 month report.. Open Dent J 2012; 6:41-5. [ Links ]
7. Sarrett DC. Clinical challenges and the relevance of materials testing for posterior composite restorations. Dent Mater 2005; 21: 9-20. [ Links ]
8. Van Dijken JWV, Sunnegädh-Grönberg. Fiber reinforced packable composite resin in class II cavities. J Dent 2011; 34(10):763-9. [ Links ]
9. Belli S, Erdemir A, Ozcopur M, Eskitascioglu G. The effect of fibre insertion on fracture resistance of root-filled molar teeth with MOD preparations restored with composite. Int Endod J 2005; 38: 73-80. [ Links ]
10. Xu HHK, Schumacher GE, Eichmiller FC, Peterson RC, Antonucci JM, Mueller HJ. Continuous-fiber performs reinforcement of dental resin composite restorations. Dent Mater 2003; 19: 523-30. [ Links ]
11. Sakaguchi RL, Cross M, Douglas WH. A simple model of crack propagation in dental restoratives. Dent Mater 1992; 8: 131-6. [ Links ]
12. Manhart J, Chen H-Y, Hickel R J. Clinical evaluation of the posterior composite QuiXfil in class I and class II cavities: 4-year follow-up of a randomized controlled trail. Adhes Dent 2010; 12(3):237-43. [ Links ]
13. Lassila LV, Vallittu PK. The effect of fibre position and polymerization condition on the flexural properties of fibre-reinforced composite. J Con Dent Prac 2004; 5: 12-23. [ Links ]
14. Kelly JR, Tesk JA, Sorenson JA. Failure of all-ceramic fixed partial dentures in vitro and in vivo: analysis and modelling. J Dent Res 1995; 74: 1253-8. [ Links ]
15. Deliperi S. Direct fiber reinforced composite restoration in an endodontically treated molar: a three year case report. Oper Dent 2008; 33(2):208-14. [ Links ]
16. Liu Y, Sagi S, Chandrasekar R, Zhang L, Hedin NE, Fong H. Preparation and characterization of electrospun SiO2 nanofibers. J Nanosci Nanotechnol. 2008; 8(3): 1528-36. [ Links ]
17. Xia Y, Zhang F, Xie H, Gu N. Nanoparticle-reinforced resin based dental composites. J Dent 2008; 36(6): 450-5. [ Links ]
18. Lassila LV, Garoushi S, Bijelic J, Vallitu PK. Mechanical characterization of short fiber reinforced composite Xenius. IADR 2013 Abstract 1562. [ Links ]
19. Garoushi S, Sailynoya E, Vallittu PK, Lassila LV. Physical properties and depth of cure of a new short fiber reinforced composite. J Dent Mat. 2013; 29:835-41. [ Links ]
20. Garoushi S, Lassila LV, Vallittu PK. Fiber-reinforced composite substructure: load-bearing capacity of an onlay restoration. Acta Odontol Scand 2006; 64(5): 281-5. [ Links ]
21. Dyer SR, Lassila LV, Jokinen M, Vallittu PK. Effect of fiber positioning and orientation on fracture load of fiber reinforced composite. Dent Mater 2004; 20: 947-55. [ Links ]
22. Vallittu PK. Strength and interfacial adhesion of FRC-tooth system. In: Vallittu PK (ed.) The 2nd Symposium on Fibre reinforced Plastics in Dentistry. University of Turku, Institute of Dentistry, 2001(b). [ Links ]
23. Frater M, Forster A, Kereszi'uri M, Braunitzer G, Nagy K. In vitro fracture resistance of molar teeth restored with a short fiber reinforced composite material. J Den 2014; 42(9): 1143-50. [ Links ]
24. Ellakwa AE, Shortall AC, Marquis PM. Influence of fibre position on the flexural properties and strain energy of a fibre reinforced composite. J Oral Rehabil 2003; 30: 679-82. [ Links ]
25. Lee JJ, Nettey-Marbell A, Cook A Jr, Pimenta LA, Leonard R, Ritter AV. Using extracted teeth for research: The effect of storage medium and sterilization on dentin bond strengths. J Am Dent Assoc 2007; 138(12): 1599-603. [ Links ]
26. Sachdeira K, Singla A, Mahajan V, Saini SS. Effect of storage media on sheer bond strength of orthodontic brackets: An in vitro study. JSOS 2012; 46(4): 203-9 [ Links ]
27. Carrilho MRO, Carvalho RM, de Goes MF, di Hipólito V. Chlo rhexidine preserves dentin bond in vitro. J Dent Res 2007; 86(1):90-4 [ Links ]
28. Wirsching E, Loomans BAC, Klaiber B, Dörfer CE. Influence of matrix systems on proximal contact tightness of 2- and 3-sur- face posterior composites in vivo. J Dent 2011; 39:386-95 [ Links ]
29. Naz F, Shirazi U, Kahn SR, Tariq U. Choice of matrix systems for direct posterior composites by dentists in Lahore. PODJ 2013; 33(1):141-4 [ Links ]
30. Lowe AH, Burke FJT, McHugh S, Bagg J. A survey of the use of matrix bands and their decontamination in general dental practice. BDJ 2002; 192(40):40-2 [ Links ]
31. de Melo Maranhäo K, Klautau EB, Pereira PMM, Guimarães RB, Pantoja VG. The effect of storage solutions on enamel of bovine teeth. Salusvita Bauru 2009; 28(2):129-34 [ Links ]
32. Tosun G, Sener Y, Sengun A. Effect of storage duration/solution on microshear bond strength of composite to enamel. Dent Mat 2007; 26(1): 116-21 [ Links ]
33. Stewardson DA, Shortall AC, Marquis PM. The effect of clinically relevant thermocycling on the flexural properties of endodontic post materials. J Dent 2010; 38(5): 437-42. [ Links ]
34. Naumann M, Metzdorf G, Fokkinga W, Watzke R, Sterzen bach G, Bayne S, Rosentritt M. Influence of test parameters on in vitro fracture resistance of post-endodontic restorations: a structured review. J Oral Rehab 2009; 36: 299-312. [ Links ]
35. Michael MC, Hussein A, Baker WZW, Sulaiman E. Fracture resistance of endodontically treated teeth: an in vitro study. Arc Orofac Sci 2010; 5(2):36-41. [ Links ]
36. Hayashi M, Takahashi Y, Imazato S, Ebisu S. Fracture resistance of pulpless teeth restored with post-cores and crowns. Dent Mater 2006; 22: 477-85. [ Links ]
37. Tobón-Arroyave S I, Restrepo-Pérez M M, Arismendi-Echa varria J A, Velásquez-Restrepo Z, Marin-Botero M L, Garcia-Dorado E C. Ex vivo microscopic assessment of factors affecting the quality of apical seal created by root-end fillings. Int Endod J 2007; 40(8):590-602. [ Links ]
38. Sorrentino R, Monticelli F, Goracci C, Zarone F, Tay FR, Garcia-Godoy F, Ferrari M. Effect of post-retained composite restorations on the fracture resistance of endodontically-treated teeth related to the amount of coronal residual structure. Am J Dent 2007; 20:269-74. [ Links ]
39. Yoldas O, Akova T, Uysal H. An experimental analysis of stresses in simulated flared root canals subjected to various post-core applications. J Oral Rehabil 2005; 32: 427-32 [ Links ]
40. Secilmis A, Dilber E, Ozturk N, Yilmaz FG. The effect of storage solution on mineral content of enamel. Materials Science and Applications 2013; 4: 439-45 [ Links ]
41. Mohammadi N, Kahnamoiji MA, Yeganeh PK, Navimipour EJ. Effect of fiber post and cusp coverage on fracture resistance of endodontically treated maxillary pre- molars directly restored with composite resin. J Endod 2009; 35(10):1428-32 [ Links ]
42. Garoushi S, Vallittu PK, Lasilla LV. Fracture toughness, compressive strength and load-bearing capacity of short fibre- reinforced composite resin. Chin J Dent Res 2011; 14(1): 15-9 [ Links ]
43. Raum K, Kempf H, Hein HJ, Schubert J, Maurer P. Preservation of microelastic properties of dentine and tooth enamel in vitro - a scanning acoustic microscopy study. Dent Mat 2007; 23(10) 1221-8 [ Links ]
44. Kitasako T, Tagami Y, Burrow MF, Nikaido J. The influence of storage solution on dentine bond durability of resin cement. Dent Mat 2000; 16(1):1-6 [ Links ]
45. Jaffer S, Oesterle LJ, Neman S. Storage media effect on bond strength of orthodontic brackets. Am J Orthod Dentofacial Orthop 2009; 136(1) 83-6 [ Links ]
46. Nam S-H, Chang H-S, Min K-S, Lee Y, Cho H-W, Bae J-H. Effect of the number of residual walls on fracture resistances, failure patterns, and photoelasticity of simulated premolars restored with or without fiber-reinforced composite posts. J Endod 2010; 36(2): 291-301. [ Links ]
47. Fennis WMM, Tezvergil A, Kuijs RH, Lasilla LVJ, Kreulen CM, Creugers N, Vallittu PK. In vitro fracture of fiber reinforced cusp-replacing composite restorations. Dent Mater 2005; 21: 565-72. [ Links ]
48. Akman S, Akman M, Eskitascioglu G, Belli S. Influence of several fibre-reinforced composite restoration techniques on cusp movement and fracture strength of molar teeth. Int En-dod J 2011; 44(5):407-15. [ Links ]
49. Tezvergil A, Lassila LVJ, Vallittu PK. The shear bond strength of bidirectional and random-orientated fibre-reinforced composite to tooth structure. J Dent 2005; 33(6):509-16. [ Links ]
50. Lammi M, Tanner J, Le Bell Ronnlof A-M, Lassila LV, Vallittu PK Restoration of endodontically treated molars using fiber reinforced composite substructure. IADR 2011, Abstract 2517. [ Links ]
51. Taha NA, Palamara JE, Messer HH. Fracture strength and fracture patterns of root filled teeth restored with direct resin restorations. J Dent 2011; 39(8):527-35. [ Links ]
 Correspondence:
Correspondence:
HJ Visser
PO Box 294, Kleinmond,7195
Tel: +27 28 271 5321
E-mail: landas@lando.co.za













