Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.70 n.8 Johannesburg 2015
RESEARCH
Percutaneous Exposure Incidents - prevalence, knowledge and perceptions of dental personnel and students at a dental training site in KwaZulu-Natal
I MoodleyI; S NaidooII
IBDTh (UDW), MSc (Dent) (UWC). Department of Community Oral Health, University of the Western Cape, Tygerberg
IIBDS(Lon), LDS.RCS (Eng), MDPH (Lon), DDPH.RCS (Eng), MChD (Comm Dent), PhD (US), Dip lInt Research Ethics (UCT). Senior Professor and Principal Specialist, Department of Community Oral Health, University of the Western Cape, Tygerberg
ABSTRACT
Healthcare workers, including dental practitioners and dental students, are at risk of occupational exposure to blood-borne pathogens such as hepatitis B, C and HIV. The present study set out to determine the prevalence, knowledge, management and perceptions of percutaneous injuries among staff and students at a dental training institute in Durban, KwaZulu-Natal with a view to identifying policies aimed at reducing the incidence. The prevalence of percutaneous injuries experienced by dental staff and students from 2001 to 2011 was determined. The levels of knowledge and their management of percutaneous injuries were determined among current dental staff and students. The dental department sustained 40% of total Hospital injuries, and of these 76% were suffered by students and 24% by staff. 22% of the sample had sustained a percutaneous injury, and of these, 57% had endured more than one and 24%, three or more injuries. Most current respondents had reported the incident (81%) and had taken the initial dose of post exposure prophylaxis; however, only 22% had taken the medication for the recommended period of four weeks. Avoiding percutaneous injuries by adopting safe work practices is probably the best practice to prevent transmission of blood-borne infections such as Hepatitis and HIV.
INTRODUCTION
Healthcare workers (HCW) are on a daily basis at risk of exposure to blood-borne pathogens through percutaneous exposure incidents (PEI). "Percutaneous exposure incident" is a broad descriptive term that includes needlestick and injury with a sharp object, as well as cutaneous and mucosal exposures to blood, saliva, tissue and other bodily fluids that are potentially infectious.1 Nurses, physicians, surgeons, laboratory workers, dental and medical personnel, and students in clinical training are considered high risk categories.
Oral health care workers are particularly vulnerable as the dental environment is unique when compared with other health care settings due to the oral cavity being a small operating field, the close contact that is required between dental personnel and the patient during procedures, the possibility of sudden movements of the patient, the use of sharp dental instruments and the likelihood of direct or indirect contact with traumatized tissues, saliva and blood, all on a daily basis.2 Furthermore, collisions with sharp objects can occur due to the close positioning of the instrument delivery system which houses the handpieces, most probably fitted with pointed burs, and handily placed to effect injury when the operators themselves move without care.
The literature has shown that the common site of injury is one of the fingers on the non-working hand which plays a supportive role in dental procedures.4,5 Other areas include the arm, palm, thigh, leg and foot. The nature of the injury can be superficial (scratch without bleeding), moderate (broken skin with bleeding) or deep (needle stick or deep cut with or without bleeding).
Mucous membrane exposure is another risk wherein blood, body fluid or tissue comes into contact with the eye, nose or mouth. Aerosols created during dental procedures with the use of high-speed handpieces and ultrasonic scalers as well as flying chips of calculus during scaling, or of amalgam during restorative procedures, or of fragments of tooth and bone during surgical procedures, can easily penetrate the eye, nose and mouth if there is no proper protection. Non-intact exposed skin that is chapped, abraded or previously injured is also susceptible to percutaneous exposure injuries.
Most injuries occur during oral surgery procedures (35%), 19% during restorative work, 13% in hygiene procedures and 9% are associated with periodontal surgery.6 Research indicates that the majority occur as a result of an accident with the dental syringe during the administration of a local anaesthetic.4,6
The reported prevalence of percutaneous injuries among dental students ranges from 20%-80%.4,7-10 Students are at a higher risk due to their inexperience in handling clinical instruments and infection control procedures5 and by the pressure occasioned by the need to complete a set number of clinical case requirements to the satisfaction of the supervisor.
A percutaneous exposure incident places a healthcare worker at a significant risk of blood- borne infections that can be transmitted from the patient. Hepatitis B virus (HBV), hepatitis C virus (HCV) and human immunodeficiency virus (HIV) are the blood-borne pathogens of concern. Other infections that can be transmitted through PEI include syphilis, malaria and herpes.11 HBV is more readily transmitted in the dental setting. The World Health Organization estimates that of the global burden of disease among HCW's, 40% of the hepatitis B and C infections and 2.5% of the HIV infections are attributable to exposures at work.
The risk of contracting disease from a single percutaneous exposure to HBV-infected blood can range from 6% to 30%12 depending on the presence of hepatitis B e antigen (HBeAg) in the source individual. A safe and effective vaccine against HBV has been available since 1982 resulting in a dramatic reduction of the prevalence of HBV.11
The estimated risk for infection after a percutaneous injury and exposure to HCV-infected blood is 0%-7%.10 The risk from a blood splash is believed to be very small; however HCV infection from such an exposure has been reported.13
Symptoms of HCV often do not emerge for 20-30 years after viral transmission occurs and the disease may be undiag-nosed for protracted periods. Moreover, there is still no effective vaccine or post-exposure prophylaxis against HCV.11
The risk of transmission of HIV from a sharps injury is less than 0.3% (stated in another way, 99.7 percent of exposures do not lead to infection) and the risk after exposure to the eyes, nose or mouth is 0.09%.14 Several factors, though, can influence the risk of transmission. These include a deep injury, a hollow-bore blood-filled needle, the quantity of blood, visible blood on the device, high viral ti-tre status of a newly infected patient or those in a terminal state, and prolonged exposure to the blood of a patient as well as high susceptibility of the exposed person.15 Taken together, these factors can increase the risk of HIV infection to 5 %.11 As the prevalence of HIV in sub-Saharan Africa is the highest in the world (22.4 million people living with HIV),16 the potential for local health care workers to be exposed is high.17
During the last few decades, strategies such as hepatitis B vaccination, adoption of standard precautions, improved instrument design such as safety needle devices, worker education and training and the utilization of personal protective equipment have been implemented in the endeavour to reduce percutaneous injuries.11 Despite these attempts the problem still persists among health care workers, placing a significant emotional and psychological toll on the occupationally exposed.
The KZN Oral and Dental Training Centre (ODTC) is located within a provincial hospital and is the site for the clinical training of dental therapy and oral hygiene students at the University of KwaZulu-Natal (UKZN). The province has the highest burden of HIV/AIDS infected and TB patients in South Africa and students and staff are in contact on a daily basis with patients who are carriers of potentially infectious diseases such as HIV, tuberculosis (TB) and hepatitis.
The aim of the present study was to determine the prevalence, knowledge, management and perceptions of percutaneous injuries among dental staff and students at the KZN Oral and Dental Training Centre by
1. recording the frequency of occurrence of needlestick and sharps injuries experienced at the Oral and Dental Training Centre through a retrospective analysis over a period of time (2001-2011), and further to:
2. determining the knowledge of current dental staff and students on the clinical management of such injuries and their perceptions through a cross-sectional study and by comparing current Departmental policies and clinical protocols with the recommended universal/ standard precautions on the management of percutaneous exposure injuries.
METHODOLOGY
Information for the retrospective study pertaining to percutaneous injuries at the Oral and Dental Training Centre from 2001 to 2011 was accessed from entries made in a log book kept at the staff clinic in the main hospital in which details of all such incidences were recorded. Statistics of all health care workers were therefore available. Data specific to the dental department was captured on a structured collection sheet.
A cross-sectional study used a self-administered questionnaire to determine the knowledge, management and perceptions of percutaneous exposure incidents among current dental staff and students. Information was collected regarding the understanding of percutaneous injuries, infection control practices, the reporting of the incident and the use of post-exposure prophylaxis. The sample was drawn from the dental clinical staff at ODTC (dentists, dental therapists, oral hygienists and dental assistants) and dental therapy and oral hygiene students from UKZN. Each individual, staff or student, was personally approached and invited to participate, having been informed that participation was voluntary. A stratified random sampling method based on the extent of clinical experience was used to divide the student study population (n=90) into sub-groups and a random sample was taken from each sub-group. Hence, the student sample included mainly second and third year students (n= 47) with a small selection (n=13) of first year students whose clinical exposure was observation of dental procedures. The final sample comprised 40 members of staff and 60 students for a total of 100 and was viewed as representing the combined experience of those involved in the discipline. The response rate for staff was 93% and for students, 88%.
In addition, the current Hospital policy regarding percutaneous exposures was evaluated in comparison with a list of gold standard criteria as recommended by the Centre for Disease Control (CDC) for the management of percutaneous injuries.1
Ethical clearance for the research was obtained from the University of Western Cape (Ref No. 11/4/27). The data was captured in MS Excel, basic descriptive analyses completed and the files were imported into SPSS version 20.0 for further assessment.
RESULTS
Log book data
Over the study period from 2001 to 2011, 178 percutaneous injuries were recorded at the King George Hospital in which the ODTC is situated (Table 1). The personnel from ODTC sustained the most number of percutaneous injuries (n=72) followed by the nursing staff (n=61) and medical officers (n=22).
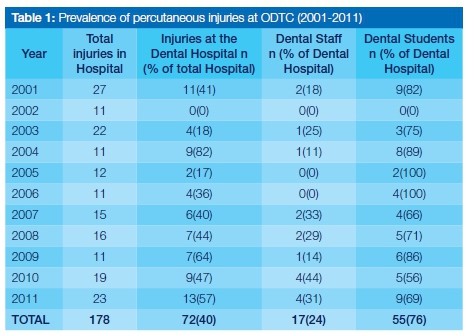
Given that every injury in fact had been reported in the logbook maintained at the staff clinic, the risk of dental staff and students suffering percutaneous injuries was 0.4 (72/178) when compared with other categories in the Hospital. This meant that out of every ten injuries recorded in the log book, four had been sustained by dental personnel who therefore had a higher probability of incurring a percutaneous injury than did other cadres of health workers in the Hospital. The risk for medical officers was 0.1 (22/178).
Over the study period, Dentistry incurred an average of 6.5 injuries per year (Table 1: 72/11 = 6.5). Dental students had a high prevalence of percutaneous injuries, constituting 76% of all Dental Hospital incidences with a mean of five injuries reported per year. The prevalence of percutaneous injuries among dental staff (dentists, dental therapists, oral hygienists and dental assistants) was 24%.
The current sample
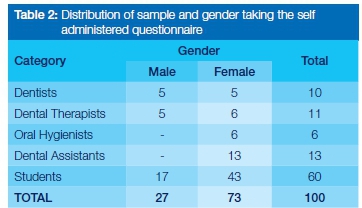
The cross-sectional study was conducted on a mixed sample which included both dental staff and students and in which the greater proportion were females (Table 2)
Analysis of the self-administered questionnaire among this sample revealed that the majority of the study population had a good understanding of percutaneous injuries with more than half (56.2%) defining this as "where a practitioner has accidentally pricked/injected themselves with a needle, scaler or other sharp, infected instrument" and almost 15% indicated that they thought it was "a visible injury when there is a breach in the epidermis, affecting underlying blood vessels resulting in bleeding." Most of the respondents (83%) recorded that they adhered to the practice of standard precautions when treating patients. Almost three quarters (74%) of those having had a PEI had previously completed three doses of the Hepatitis B vaccine, but only 41% had checked whether they had any immunity after taking the vaccine. More encouragingly, 44% reported having had a booster vaccine.
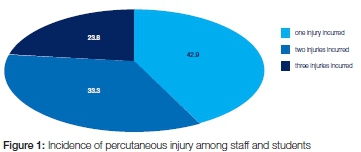
Amongst the current staff and student cohort, 22% reported having sustained a percutaneous injury. Of these, 43% had experienced at least one, more than half (57%) had suffered more than one injury and almost a quarter (24%) had experienced three or more PEIs (Figure 1).
More than a third of the injuries (33.3%) were due to mishaps with the dental syringe and needles (Table 3). Injuries associated with the use of the dental elevator and eye splashes were also common (16.7% each).

Most percutaneous injuries (63%) were caused during a minor oral surgery procedure (Table 4). Nearly two-thirds (63%) of the injuries occurred to the finger, especially when a minor oral surgery procedure was being performed (40.7%).

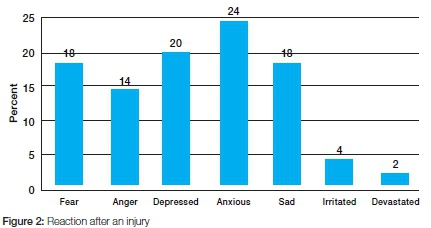
Two out of every three incidents (66.7%) occurred during, and a quarter (25%) occurred after, the dental procedure, during the cleaning up process. Oral health care workers reported considerable emotional distress, displaying reactions of anxiety, fear, sadness and anger and some were totally devastated. Anxiety was the most common emotion reported by nearly quarter of the sample (Figure 2).
Most respondents had reported the incident (81%) and those that had not had considered the injury too small to be of any significance, or that the source patient had been shown to be HIV negative whilst some thought there was no risk of infection or were unaware that they had to report the incident. Almost all the respondents who sustained and reported percutaneous injuries (94%) took the post exposure prophylaxis (PEP), however only 22.2% had taken the medication for the recommended period of four weeks.
More than half of the respondents (55.6%) had taken the PEP for between two to four weeks. Only 13.6% of those that incurred a percutaneous injury had the recommended full series follow-up blood tests and 18% did not have any follow-up blood tests at all.
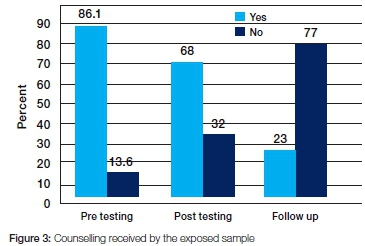
Most of the respondents (86%) had received pre-test counselling, 68% received post-test counselling but only 23% had any follow-up counselling after an injury (Figure 3).
A structured data capture sheet was used in the evaluation of the ODTC policy for the management of percutaneous injuries (Department of Health Guidelines on Standard Precautions, Chapter 15). The policy adopted by the ODTC is in keeping with recommended international guidelines for the management of percutaneous injuries (CDC, 2005) with a clearly defined aim, a designated occupational health officer and good referral systems in place. Post exposure prophylaxis is made available. Students are made aware of this policy during orientation at the beginning of each academic year.
Although the ODTC policy is in keeping with international guidelines, the following shortfalls were noted:
- The protocol is not clearly displayed on notice boards for staff and students to follow.
- There is very little in-service training offered.
- There is no induction training for new staff.
- Follow-up of student and staff after an injury is not ensured or monitored.
- There is no process for follow-up counselling.
- There is no monitoring or regular review of the policy.
DISCUSSION
By analyzing and investigating the causes of injuries, useful information may be gleaned. Information regarding the circumstances surrounding the reported injury may be valuable in preventing further injuries by modifying work practices. The needle was the most common source of injury among dental students and staff (33.3%). This finding concurs with previous studies which reported the syringe needle to be associated with 30-36% of all percutaneous injuries at a dental training institute.3,4,816,19-21
Most injuries occurred when the needle was being withdrawn from the patient's mouth, while recapping the needle and when removing the used needle from the syringe.
Current safety measures recommended are the use of the "one-handed scoop technique" to recap used needles, placing a sharps container in each cubicle in the clinic to avoid staff walking around with contaminated needles and not removing needles using the hands but rather using an instrument such as artery forceps.... which may advantageously be attached to each sharps container. In addition to these measures, a device can be placed on the work surface that holds the needle sheath and allows for recapping without touching the sheath, or adopting the use of a safety syringe that has a sliding protective sheath over the needle. Another method of reducing accidents due to needles is the use of an incinerator in which the needle is completely incinerated after use leaving only the plastic hub which can then be harmlessly removed. These work practices are in keeping with the current CDC guidelines which recommend that used needles should never be recapped, purposely bent or otherwise manipulated.22
The surgical elevator was the instrument most often associated with injuries (16.7%) and it was also that most frequently contaminated with blood when the injury occurred. Mucosal eye splashes accounted for nearly a fifth of all percutaneous exposures (16.7%) which is suggestive of inadequate eye protection during dental procedures. These results are slightly higher than those found in the study by Siddiqi in 2008 (Coupland elevator 14%, mucosal eye splashes, 15%).4
Most of the injuries occurred while the operator was performing minor oral surgical procedures, followed in frequency by scaling and polishing and restorative procedures. Cleveland et al.6also found that while most percutaneous injuries occurred in oral surgical procedures, whilst the findings for other procedures differed: 19% of injuries were related to restorative procedures and 13% to oral hygiene procedures. Injuries occurring during minor oral surgical procedures can be reduced by strictly adhering to the latest standard precautions of double gloving and the use of blunt-tip suture needles as an alternative to the sharp product currently used. Blunt-tip suture needles have been shown to reduce needlestick injuries by 69%.22
The present study, in agreement with similar studies conducted in South Africa,4 showed that the finger of the non-dominant hand that plays a supportive role was the most common site of percutaneous injuries, followed by the eye.
Management of PEI
Percutaneous injuries were found to be appropriately managed at the ODTC. Eighty percent of the respondents who had sustained such an injury had reported the incident. This observation is commendable as previous studies have documented under-reporting as a universal problem.24,25 In addition, 70% of those who had sustained a percutaneous injury had sought medical attention at once. The transmission of HIV infection does not occur immediately on exposure, therefore the timeous initiation of post-exposure prophylaxis creates an opportunity for the antiretroviral drugs to modify or prevent viral replication thereby preventing systemic infection. Treatment should commence promptly, preferably 1-2 hours after the exposure and not later than 72 hours.1
Post-exposure prophylaxis is made available to both staff and students at the staff clinic in the hospital. A basic regime of two nucleoside reverse transcriptase inhibitors (NRTIs) is prescribed and a protease inhibitor (PI) is given if the risk for transmission of HIV is considered high. The CDC recommendations state that a combination of Zidovudine (AZT 200mg every 8 hours) and Lamivudine (3TC 150mg b.d.) for 28 days should be considered for treatment of all exposures involving HIV-infected blood, fluid containing visible blood or other potentially infectious fluid or tissue. Indinavir should be added to this regime for high risk exposures. It was of concern, though, that there was poor final compliance as only 22% of those incurring a percutaneous injury had completed the recommended regime. Siddiqi et al.4also reported a low compliance to post exposure prophylaxis (7%). An important aspect of post exposure prophylaxis is the completion of a four week course of anti-retrovirals when indicated.1 One of the reasons given for not completing the post exposure regime was not being able to cope with the side effects of the medication, about 46% of which included gastrointestinal problems, the medication making them feel sick, tired and nauseous.
It was also of concern that very few participants in the present study had follow-up testing. Occupational health and safety is an important issue in the work environment. Staff and students who are in the pre-employment phase should be educated about the importance of follow-up blood tests to check for sero-conversion. It is advisable for all staff and students who suffer a percutaneous injury to diarise their test dates and ensure that the follow-up tests are carried out timeously. At least the six month follow-up test should be done. It is also good practice for all health care workers working with blood to have an annual blood test.
In the present study, only a small cohort of the exposed population had received follow-up counselling. A percutaneous injury can impact negatively on a health care worker's personal life causing anxiety, fear and depression. The emotional distress can be severe and long lasting even though the risk of transmission is very low or there may be no transmission of serious disease. Therefore postexposure counselling is needed. However, this is not yet available at the Hospital as a routine option. An important lesson learnt from the current study is that a supportive environment and careful monitoring of the dental personnel after a percutaneous injury are important for total rehabilitation and readjustment to the work environment.
The following recommendations are suggested to prevent PEIs in dental training institutions:
- Protocols to be followed in the event of a percutaneous injury should be clearly displayed in the clinical areas;
- Percutaneous injuries should be carefully recorded and those records should be reviewed annually as an effective tool to determine the aetiology and to make the relevant changes to work practices to prevent further injuries;
- The use of personal protective equipment (double gloves, mask and eye-shields) for every procedure should be reiterated;
- Adherence to safe work practices such as using the one-handed scoop technique to recap needles or a mechanical device that holds the needle cap should be encouraged;
- In addition to the adoption of safe work practices, institutions should identify, evaluate and select safety devices such as needle incinerators, needle guards and safety syringes for routine use.
- In-service training of safe work practices should be provided upon initial employment and when students first enter the clinical area and should be followed by continuous education on an annual basis to keep updated with current safe work practices and work modifications, and in the promotion of safety and prevention awareness to reduce or prevent percutaneous injuries.
CONCLUSION
A percutaneous exposure incident is a serious occupational health hazard that places dental staff and students at risk of transmission of blood-borne pathogens. The current study shows that percutaneous injuries are an ongoing problem at the ODTC and highlights the fact that dental personnel are at a higher risk of suffering percutaneous injuries than other health professionals working at the King George Hospital. High risk activities have been identified, enabling recommendations on modifications of work practice to reduce the incidence of percutaneous injuries at the ODTC. Accidents are sometimes unavoidable but attending to a percutaneous injury as soon as it occurs, treating it as a medical emergency and following through with the management protocol are of utmost importance to prevent the transmission of blood-borne diseases. It is of concern that the present study revealed that personnel do not comply with management protocols regarding completion of post-exposure prophylaxis and follow up tests.
Conflict of interest: None declared
ACRONYMS
CDC: Centre for Disease Control
HCW: Healthcare workers
HBeAg: Hepatitis B e antigen
HBV: Hepatitis B virus
HCV: Hepatitis C virus
HIV: human immunodeficiency virus
ODTC: KZN Oral and Dental Training Centre, KwaZulu-Natal
NRT: nucleoside reverse transcriptase inhibitors
PEI: percutaneous exposure incidents
PEP: post exposure prophylaxis
PI: protease inhibitor
References
1. Centers for Disease Control and Prevention. Updated US Public Health Service guidelines for the management of oc cupational exposures to HIV and recommendations for post-exposure prophylaxis. Morbidity and Mortality Weekly Report. 2005;54(RR09):1-17. [ Links ]
2. Porter KM, Scully C, Porter S, Theyer Y. Needlestick injuries to dental personnel. Journal of Dentistry 1990;18:258-62. [ Links ]
3. Younai FS, Murphy DC, Kotelchuck D. Occupational expo sures to blood in a teaching environment: results of a ten-year surveillance study. Journal of Dental Education. 2001; 65(5): 436-48. [ Links ]
4. Siddiqi A, Morkel JA, Stephen L. Occupational blood exposure at a dental faculty. Dental Horizons 2008; 5: 25-9. [ Links ]
5. Callan RS, Caughman F, Budd ML. Injury reports in a dental school a two year overview. Journal of Dental Education 2006; 1089-97. [ Links ]
6. Cleveland JL, Barker LK, Cuny EJ, Panlilio AL. National Surveillance System for Health Care Workers Group. Preventing percutaneous injuries among dental health care personnel. Journal of the American Dental Association. 2007; 138:169-78. [ Links ]
7. Hlongwa P. Accidental occupational injuries in a South African dental school. IADR South African Division Meeting and Skills Transfer Workshop-September 13-14, 2010. [ Links ]
8. Sofola OO, Folayan MO, Denloye OO, Okeigbemen SA. Occupational exposure to bloodborne pathogens and management of exposure incidents in Nigerian dental schools. Journal of Dental Education. 2007; 71(6):832-7. [ Links ]
9. Machado-Carvalhais HP, Martins PM, Ramos-Jorge ML, Magela-Machado D et al. Management of occupational blood- borne exposure in a dental teaching environment. Journal of Dental Education 2007; 71(10):1348-55. [ Links ]
10. Zhang Z, Moji K, Cai G, Ikemoto J, Kuroiwa C. Risks of sharps exposure among health science students in northeast China. Bio Science Trends.2008; 2: 105-11. [ Links ]
11. Wilburn SQ, Eijkemans G. Preventing needlestick injuries among healthcare workers: A WHO-ICN collaboration.International Journal of Occupational Environmental Health. 2004; 10: 451-6. [ Links ]
12. Centers for Disease Control and Prevention. Workbook for designing, implementing, and evaluating a sharps injury prevention program (2004). Available from URL: www.cdc.gov/sharpssafety/pdf/WorkbookComplete.pdf [ Links ]
13. Centers for Disease Control and Prevention. Recommendations for Prevention and Control of Hepatitis C Virus (HCV) Infection and HCV-Related Chronic Disease. Morbidity and Mortality Weekly Report.(1998b); 47(RR-19). [ Links ]
14. Sagoe-Moses C, Pearson RD, Perry J, Jagger J. Risks to health care workers in developing countries. North England Journal of Medicine. 2001; 345:538-41. [ Links ]
15. Cardo DM, Culver DH, Ciesielski CA, Srivastava PU, Marcus R, Abiteboul D, Heptonstall J, Ippolito G, Lot F, McKibben PS, Bell DM. A case control study of HIV sero-conversion in health workers after percutaneous exposure. Centres for Disease Control and Prevention of Needlestick Surveillance Group. North England Journal of Medicine1997; 337:1485-90. [ Links ]
16. UNAIDS report on the global AIDS epidemic-2010. Available fromURLhttp://www.unaids.org/en/regionscountries/countries/southafrica/ [ Links ]
17. Prüss-Üstün A, Rapiti E, Hutin, Y. Sharps injuries: Global burden of disease from sharps injuries to health-care workers. Geneva, Switzerland: World Health Organization(2003). Available at www.who.int/peh/burden/9241562463/sharptoc.htm [ Links ]
18. Cleveland JL, Barker L, Gooch BF, Beltrami EM. Use of HIV post exposure prophylaxis by dental health-care personnel. An overview and updated recommendations. Journal of the American Dental Association. 2002; 133(12):1619-26. [ Links ]
19. Panagakos FS, Silverstein J. Incidence of percutaneous injuries at a dental school: A four-year retrospective study. American Journal of Infection Control. 1997; 25:330-4. [ Links ]
20. Ramos-Gomez F, Ellison J, Greenspan JED, Bird W, Lowe S, Gerberding JL. Accidental exposures to blood and body fluids among health care workers in dental teaching clinics: a prospective study. Journal of the American Dental Association.1997; 128: 1253-61. [ Links ]
21. Gonzalez CD, Pruhs RJ, Samson E. Clinical occupational blood-borne exposures in a dental school. Journal of Dental Education. 1976; 58(3): 217-20. [ Links ]
22. Centres for Disease Control and Prevention. Guidelines for infection control in dental health- care settings. Morbidity and Mortality Weekly Report- 2003; 52(No. RR-17).available from URL: http://www.cdc.gov/mmwr/preview/mmwrhtml/r5217a1.htm [ Links ]
23. Parantainen A, Verbeek JH, Lavoie MC, Pahwa M. Blunt versus sharp suture needles for preventing percutaneous exposure incidents in surgical staff. Cochrane Database of Systematic Reviews 2011;Issue 11. Art. No.: CD009170. DOI:10.1002/14651858.CD009170.pub2. [ Links ]
24. Tarantola A, Golliot F, Astagneau P, Fleury L, Brücker G, Bouvet E. Occupational blood and body fluids exposures in health care workers: four year surveillance from the Northern France Network. American Journal of Infection Control 2003; 31(6): 357-63. [ Links ]
25. Askarian M, Malekmakan L, McLaws ML, Zare N, Patterson JMM. Prevalence of needlestick injuries among medical stu dents at a University in Iran. Infection Control and Hospital Epidemiology. 2006; 27(1): 99-101. [ Links ]
 Correspondence:
Correspondence:
S Naidoo
Faculty of Dentistry, University of the Western Cape
Private Bag X1 Tygerberg, 7505
Tel: 021 937 3095. Fax: 021-931 2287
E-mail: suenaidoo@uwc.ac.za













