Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.70 no.8 Johannesburg 2015
RESEARCH
Oral complications of HIV disease in children in the post 1998 era of HAART: A descriptive cross sectional study of prevalences, retrospective and clinical
SR MthethwaI; MI MmutlanaII; A BooysenIII; N ChabikuliIV
IBDS, MPH, PhD. Sefako Makgatho Health Sciences University
IIBChD, MDS. University of Witwatersrand
IIIDip OH, H Dip OH, MBA. Smile of Joy
IVMBChB, MFamMed, MCFP, MSc. Regional Director Southern Africa, FHI 360. Honorary Lecturer Sefako Makgatho Health Sciences University, Department of Family Medicine, Honorary lecturer Pretoria University, Department of Family Medicine
SUMMARY
INTRODUCTION: The administration of HAART has changed the frequency and character of the oral complications of HIV disease.
AIMS AND OBJECTIVES: This study describes and compares the incidence and status of dental caries and the number and type of oral mucosal lesions in hospital outpatients with these data in institutionalized children who had accepted a dedicated oral and dental management programme for HIV-infected patients.
DESIGN: This was a retrospective, descriptive cross-sectional study in which existing medical records were reviewed and a clinical examination performed.
METHODS: The oral cavity of each patient was examined by two calibrated clinicians who used mouth mirrors under artificial light. The presence and status of dental caries and the presence of oral soft tissue lesions were recorded using, respectively, the WHO Oral Health Surveys Basic Methods and the diagnostic classification and criteria for oral soft tissue lesions associated with HIV of the EC-Clearinghouse.
RESULTS: Oral lesions and dental caries were significantly higher (p<0.001) in hospital outpatients than in institutionalized children. Caries prevalence (p = 0.002) and severity p<0.0001) were significantly higher in hospital outpatient children receiving HAART than in those not on HAART.
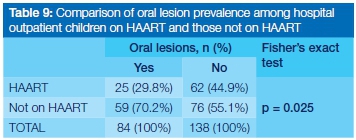
CONCLUSIONS: The prevalence of oral lesions was significantly reduced (p = 0.025) in children receiving HAART. Caries prevalence was significantly higher in children receiving HAART than in those not on HAART.
*HAART involves the simultaneous administration of three main classes of drugs together with a fourth subclass. Examples are:
- Nucleoside analogue reverse transcriptase inhibitors (nRTI 's)
- Protease inhibitors (PI's)
- Non-nucleoside reverse transcriptase inhibitors (NNTRI's)
- Nucleotide transcriptase inhibitors( NTI's) Subclass.
INTRODUCTION AND BACKGROUND
Whilst there are very few published studies of oral manifestations of HIV in children in Africa, Naidoo and Chikte did investigate the status in children not receiving HAART in South Africa.1-3 The frequency and character of the oral complications of HIV disease has changed with the introduction of HAART.4 Research on the extent of these changes in children is important in the context of developing countries where efforts are being made to scale up the provision of HAART to eligible patients.5
This study describes and compares the frequency and status of dental caries and the number and type of oral mucosal lesions in HIV-infected children who accepted a dedicated oral and dental programme. The occurrence of oral lesions was related to levels of CD4 cell counts.
OBJECTIVES OF THE STUDY
1. To describe the demographic characteristics of HIV positive children attending a hospital outpatient department and of those in an institutionalized setting.
2. To describe and compare (a) the dental caries status and (b) the number and type of oral mucosal lesions in HIV positive children between those attending a hospital outpatient department with those of children residing in an institutionalized setting.
3. To assess the association between the presence of oral mucosal lesions and the levels of CD4 cell counts among children in the hospital outpatient department.
4. To compare the prevalence of oral mucosal lesions among the hospital outpatient department children between those on HAART and those not receiving HAART.
MATERIALS AND METHODS Study design
This was a descriptive cross-sectional study with data gathered from medical records, a questionnaire and clinical examinations.
Study population
The study population consisted of HIV infected paediatric patients referred to George Mukhari and Kalafong outpatient HIV clinics between May 2005 and April 2006 and of HIV infected children institutionalized in twenty orphanages in Johannesburg, Pretoria and Bronkhorstspruit. During the observation period 486 children visited the outpatient clinics and 291 were examined at the orphanages.
Ethical considerations
Parents/caregivers gave permission for children to participate in this routine health service at the outpatient HIV clinics of Kalafong and George Mukhari Hospitals and at orphanages caring for children diagnosed as having HIV in Johannesburg, Pretoria and Bronkhorstspruit. Permission to use HIV/ AIDS programme records was granted by the Programme Director and the CEO's of the participating hospitals. The study protocol was approved by the Ethics Committee of the University of Limpopo (Medunsa Campus).
Study sample
The sample size was calculated based on two sets of prevalence data:
I. The prevalence of oral lesions in hospital outpatient children in Cape Town, South Africa was found by Naidoo and Chikte to be 63%.1
II. The prevalence of oral lesions in institutionalized children in Cape Town, South Africa was found by Naidoo and Chikte to be 45%.1
The sample size for hospital outpatient children was estimated at 206 in Epi Info Version 3.3.2 software,8 at the confidence interval of 95% and absolute precision of 5% assuming 63% oral lesions prevalence. In the event, a sample of 222 was drawn. The sample size for institutionalized children was estimated at 165 in Epi Info Version 3.3.2 software8 at the confidence interval of 95% and absolute precision of 5% assuming 45% oral lesions prevalence. However, a sample of only 152 was drawn.
Sampling method
Random samples were selected. The lottery method of random sampling9 was used, i.e. patient files were assigned numbers, and coupons with serial numbers ranging from 1 to 486 were then thoroughly mixed in a bowl and a sufficient number were drawn at random (without replacement) to provide the desired sample size. Files corresponding to drawn numbers were separated for analysis and the remainder (non-selected files) were returned to the archives.
The research was conducted at outpatient HIV clinics of academic hospitals (Kalafong and George Mukhari) in townships on the outskirts of Pretoria, and at orphanages caring for children diagnosed with HIV in Johannesburg, Pretoria and Bronkhorstspruit.
Parents/guardians were interviewed using a structured questionnaire to obtain information regarding medical history, current medications and demographic details. Data relating to CD4 cell counts were extracted from the patients' clinic medical records. The oral cavity of each sitting patient was examined under artificial light by two calibrated clinicians using mouth mirrors. The status and frequency of dental caries and the presence of oral soft tissue lesions were assessed. The Oral Health Surveys Basic Methods of WHO were used to record dental status.6 The diagnostic classification and criteria for oral soft tissue lesions associated with HIV of the EC-Clearinghouse were applied.7 The collected data were captured in custom-made Monitoring and Evaluation data capture sheets. After completion these documents were filed in the office of the Programme Director.
MEASUREMENTS
Medical records
The data from the medical records, the completed questionnaires and from the clinical examinations were assembled in custom-designed computer monitoring and evaluation records and were coded and cleaned in Microsoft Excel software before statistical analysis.
Variables
The recording of current medication was limited to categories which were used to treat HIV and associated opportunistic infections (antiretrovirals, antifungals and antibiotics).
Dental caries were recorded using the Oral Health Surveys Basic Methods of WHO.7
Oral soft tissue lesions were evaluated using the diagnostic classification and criteria for oral soft tissue lesions associated with HIV of the EC-Clearinghouse.6
CD4 cell counts were sourced from laboratory reports.
STATISTICAL ANALYSIS / HYPOTHESIS TESTING
Frequencies, means and proportions were calculated and the data were subjected to univariate, bivariate and multivariate analysis in Statistical Analysis Software (SAS) software. Fisher's exact test was performed to test the statistical significance of differences observed in the incidence of caries, and in the presentations of oral lesions between children examined at outpatient clinics and orphanages. The chosen significance level of the tests was a p-value of less than 0.05. Statistical tests were performed: the Mann-Whitney U test to compare DMFT or dmft components between the groups; Student's t-test to compare CD4 means between children on HAART and those not on HAART; a Chi-squared test to identify any statistical significances in the differences observed in the prevalence of oral lesions in children with a CD4 count <200 cell/mm3 and those with a CD4 count >200.
RESULTS
The data of randomly selected samples of 222 hospital outpatient clinic and 152 institutionalized children were analyzed.
Objective 1: Demographic characteristics
The average age of hospital outpatient children was four years (range: one to 14 years) .Half the children were aged between two and seven years.
The average age of institutionalized children was six years with a range between one and 22 years. Half of the children were aged between four and nine years.
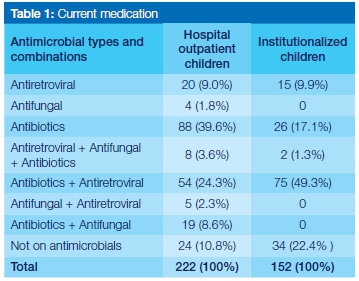
Just less than forty percent (39.1%) of hospital outpatient children were taking antiretrovirals, either alone or in combination with other medication. Antimicrobial polyphar-macy was high at 38.8% with a total of 76.1% of children taking antibiotics. Antifungal use was limited to 11.1%. A tenth (24) of the patients were not on antimicrobials.
Sixty percent of institutionalized children were taking antiretrovirals. Half of the children were on antimicrobial polypharmacy. Two-thirds were taking antibiotics. Just under a quarter (22.4%) were not on antimicrobials (Table 1).
Objective 2a: Description and comparison of dental caries status
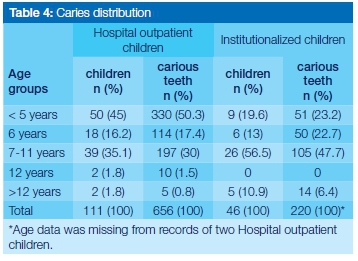
Dental caries was recorded in a considerably greater proportion of the hospital outpatient children compared with the incidence amongst institutionalized children (50% vs. 30%) Hospital outpatient children six years and under accounted for two thirds of the carious teeth occurring in this group (Table 4). Thirty percent of the carious teeth were recorded in the 7-11 years age range. Half the children (111) were caries free.
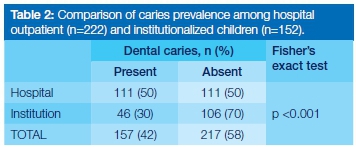
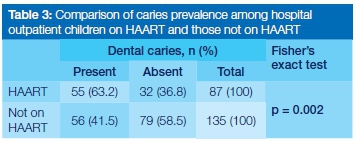
Just over two-thirds of the latter group (106) were caries free (Table 2). One and a half times as many hospital outpatient children on HAART as compared with those not on HAART (63.2% vs.41.5%) presented with caries, a statistically significant difference (Table 3).
Amongst the institutionalized children, those 7 years and older accounted for 54% of the carious teeth observed in the group.
The mean DMFT and D components were higher in hospital outpatient children on HAART than in those not on HAART (0.28 vs.0.21 and 0.26 vs.0.21). The differences were not, however, statistically significant. (Table 5).
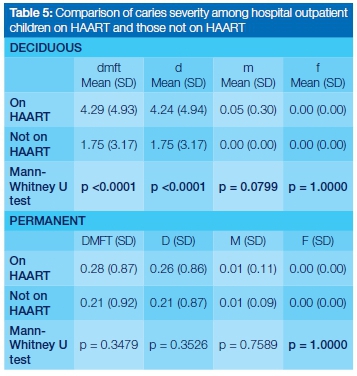
The mean dmft and d components in hospital outpatient children on HAART were more than double (4.29 vs. 1.75 and 4.24 vs. 1.75) those in children not on HAART. There is strong evidence (p <0.0001) that there is statistical significance in this difference. (Table 5).
Objective 2b: Description and comparison of number and type of oral mucosal lesions
Prevalence of oral lesions: Oral lesions were recorded in just less than forty percent (n=84) of hospital outpatient children and in less than a quarter (n=34) of institutionalized children (p<0.001).
Number of oral lesions in a mouth: multiple lesions were recorded in six (7.1%) hospital outpatient children and in four institutionalized children (11.8%). (Table 6).
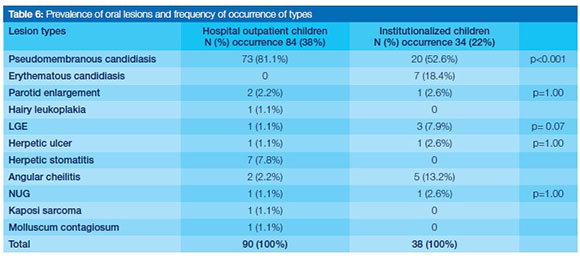
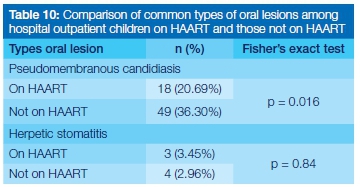
Pseudomembranous candidiasis was the most common lesion at 81.1% in hospital outpatient children. Herpetic ulcer was the second common lesion at 7.8%. Candidiasis in its two forms was the most common lesion at 71% in institutionalized children, followed by angular cheilitis at 13.2%. However, pseudomembranous candidiasis was recorded in almost three times as many hospital outpatient children as institutionalized children (30.18% vs.10.53%), a highly statistically significant finding (p<0.001). (Table 6).
Objective 3: Association between the presence of oral mucosal lesions and OD4 cell count among the hospital outpatient department children
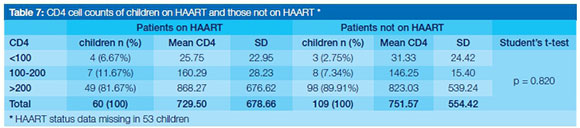
The data presented in Table 7 confirms that there is insufficient evidence (p >0.05) to demonstrate any significant difference in mean CD4 counts between patients on HAART and those not on HAART in the population.
Oral lesions were more common (54.5%) in children with a CD4 count <200 cell/mm3 but the differences were not statistically significant (p=0.21). The association between oral lesions and CD4<200 in children not on HAART was three times higher than that in children on HAART, a statistically significant difference (81.8% vs.27.3%). (Table 8.)
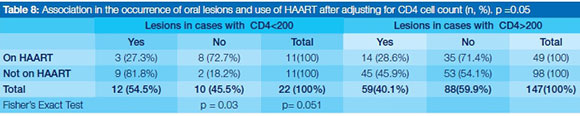
The association between the incidence of oral lesions and CD4>200 was higher in children not on HAART (45.9% vs. 28.6%), the p-value being only just greater than 0.05, suggesting that the difference in the occurrence of oral lesions between the children at CD4 >200 who are on HAART and those not on HAART is approaching statistical significance.
Objective 4: Oomparison of the prevalence of oral mucosal lesions among hospital outpatient children between those on HAART and those not on HAART
More than double the number of oral lesions were recorded in children not on HAART as in children on HAART, a statistically significant difference (70.2% vs. 29.8%).
The incidence of pseudomembranous candidiasis was statistically significantly different between children on HAART and those not receiving the drugs (36.30% vs. 20.69%, p = 0.016). (Table 10) There is insufficient evidence, however, at p >0.05, to identify statistically significant differences between the prevalences of herpetic stomatitis, angular cheilitis and parotid enlargement recorded for children on HAART and those not on HAART in the sample population.
DISCUSSION
Objective 1: Demographic characteristics
Antiretroviral use was higher (60%) in institutionalized children than in hospital outpatient children (39.1%). The proportion of children on HAART at George Mukhari and Kalafong outpatient HIV clinics was significantly (20%) lower than that reported by Michaels and colleagues in a similar setting.10 This finding may be explained by the fact that the non-governmental organization (NGO) community, which founded many of these orphanages investigated by Michaels et al, offered antiretroviral medication earlier than Government hospitals. The Government had initially doubted the effectiveness of antiretrovirals.11
Antibiotic use in the two population groups was high i.e. 66.4% for institutionalized children and 76.1% for hospital outpatient children. This may have been related to prophylaxis instituted against pneumocystis carini pneumonia, which was commenced when the CD4 dropped below 200 cells/ml3 or when there were clinical signs of advanced immune deficiency.12
Objective 2a: Description and comparison of dental caries status
Caries prevalence was significantly higher (p<0.001) in hospital outpatient than in institutionalized children. The bulk of this caries was untreated and affected deciduous teeth.
This study produced results which corroborate the findings of previous work by Naidoo and Chikte in a similar cohort.1 A possible explanation for these differences may be that nutritionists planned the diets of children in the orphanages, within the limits of available resources.3
Caries prevalence (p = 0.002) and severity p<0.0001) was significantly higher in hospital outpatient children receiving HAART than in those not on HAART. The bulk of this caries was untreated and affected deciduous teeth. This result has not previously been described and is in fact difficult to explain, but may be related to the high sugar content of AZT and other HIV medications14 and the decreased salivary flow associated with HAART use.15 These results need to be interpreted with caution as the precise HAART regimen and duration of use were not studied. This finding, while preliminary, does however suggest that the use of HAART is associated with an increased risk of dental caries in children. Previous research has described the prevalence of dental caries in adults receiving HAART when a lower prevalence of dental caries in HAART patients was reported. Further studies on the topic of antiretroviral medication and dental caries risks are therefore recommended.
Objective 2b: Description and comparison of number and type of oral mucosal lesions
The prevalence of oral lesions was significantly higher (p<0.001) in hospital outpatient than in institutionalized children and was associated mainly with the occurrence of oral candidiasis. This finding is in agreement with that of Naidoo and Chikte and of a great deal of the previous work in this field which documented candidiasis as the most frequently occurring manifestation in HIV-infected children.1,17,18 A possible explanation for this might be a relatively high level of malnutrition and poor oral hygiene in hospital outpatient children, factors which have been reported to predispose to the expression of oral lesions.16No more than two lesions per child were observed in the study groups. This finding does not support the previous research which reported up to five oral lesions per child.1 This inconsistency may be due to the use of HAART in this study.
More types of oral lesions (10 vs. 7) were observed in hospital outpatient than in institutionalized children. A variable clinical spectrum of HIV associated oral lesions in children has been described in diverse settings in South Africa, 1721 but the types of oral lesions observed in this study were largely consistent with those reported by Naidoo and Chik-te1 with NUG, LGE, herpetic stomatitis and Kaposi sarcoma being additionally recorded in hospital outpatient children. In contrast to previous findings molluscum contagiosum lesions were not observed in institutionalized children. Neither NOMA nor lymphadenopathy were documented in this study, despite Naidoo and Chikte having recorded the latter in just less than half (47%) of their subjects.1
Objective 3: Association between the presence of mucosal lesions and OD 4 cell counts among the hospital outpatient department children.
There was no statistically significant difference (p = 0.82) in mean CD4 counts between children on HAART and those not on HAART. This study does however confirm that HAART does increase the CD4 cell count.22,23 Data from 82% of the children on HAART showed an increase in the mean CD4 count from <200 cell/mm3 to 868 cell/mm3. Government policy at the time of this study directed that HAART therapy be initiated at a CD4 count <200 cell/mm3.24
There was no significant difference (p = 0.2)) in the prevalence of oral lesions in patients with a CD4 count <200 cell/mm3 and those with a CD4 count >200.
Contrary to expectations,25 this study did not find an association between the level of immunosuppression and oral lesions. The reason for this is not clear but it may be related to the fact that patients with a CD4 count <200 cell/mm3 constituted merely 13% of the study sample.
HAART use was associated with a decreased prevalence (p = 0.03) of oral lesions in patients with a CD4 count <200. The present findings seem to be consistent with other research which found that whilst a CD4 count <200 cell/mm3 predisposes towards the expression of oral lesions26,27 the administration of HAART reduces their occurrence.28
HAART use may be associated (p = 0.051) with a decreased prevalence of oral lesions in patients with a CD4 >200. These results suggest that HAART use may be associated with decreased prevalence of oral lesions in patients with a CD4 >200. This finding is consistent with the conclusions of other studies.29
Objective 4: Comparison of the prevalence of oral mucosal lesions among the hospital outpatient children between those on HAART and those not receiving Haart
The prevalence of oral lesions was significantly reduced (p= 0.025) in children receiving HAART.
The findings of the current study do not support previous research,2,21,30 which reported no change in the occurrence of oral lesions in children receiving HAART. This rather contradictory result may be due to the fact that this study used a relatively large sample size. Previous studies used small sample sizes which may have had inadequate power to detect an existing important effect. It is possible; therefore, that HAART use is indeed associated with a decreased prevalence of oral lesions. Further work is required to establish this.
This reduction was attributed to a reduction in oral candidiasis.
This finding further supports previous research which found that HAART plays an important role in controlling the occurrence of oral candidiasis.4,31
CONCLUSION
In the present study, the incidence of oral lesions and dental caries were significantly higher in hospital outpatients than in institutionalized children. Caries prevalence was significantly higher in children receiving HAART than in those not on HAART,.
Acknowledgement: The authors would like to thank the Programme Director Prof E Blignaut for her contribution and Prof H Schoeman for his assistance in analysing the data.
ACRONYMS
DMFT: decayed, missing, filled teeth (lower case dmft for deciduous dentition)
EC: European Common Market
HAART: Highly Active Anti-Retroviral Therapy
HIV: Human Immunodeficiency Virus
LGE: Linear Gingival Erythema
NUG: Necrotizing Ulcerative Gingivitis
WHO: World Health Organisation
References
1. Naidoo S, Chikte U. Orofacial manifestations in paediatric HIV: a comparative study of institutionalized and hospital outpatients. Oral Dis 2004; 10(1): 13-8. [ Links ]
2. Hamza OJM, Matee MIN, Simon ENM, Kikwilu E, Moshi MJ, Mugusi F, et al. Oral manifestations of HIV infection in children and adults receiving highly active anti-retroviral therapy[HAART] in Dar es Salaam, Tanzania. BMC Oral Health 2006; 6(1):12. Available: http://www.biomedcentral.com/472-683/6/12 [Accessed 8 June 2010]. [ Links ]
3. Blignaut E. Oral health needs of HIV/AIDS orphans in Gauteng, South Africa. AIDS Care 2007; 19(4): 532-8. [ Links ]
4. Hodgson TA, Greenspan D, Greenspan JS. Oral lesions of HIV disease and HAART in industrialized countries. Adv.Dent Res 2006; 19(1): 57-62. [ Links ]
5. World Health Organization . Scaling up antiretroviral therapy in resource-limited settings: guidelines for a public health approach. Geneva: WHO, 2002. [ Links ]
6. EC Clearinghouse. Classification and diagnostic criteria for oral lesions in HIV-infection. J Oral Pathol Med 1993; 22: 289-91. [ Links ]
7. World Health Organization. Oral Health Surveys. Basic Methods. 4th edn. Geneva: WHO, 1997. [ Links ]
8. Epi Info[program]. [ Links ]3.3.2 version, 2005.
9. World Health Organization. Health Research Methodology: A Guide for Training in Research Methods. Regional Office for the Western Pacific Manila, 1992. [ Links ]
10. Michaels D, Eley B, Ndhlovu L, Rutenberg N, Khan H. ''Expanding pediatric access to antiretroviral therapy in South Africa''. Horizons Research Summary. Washington DC: Population Council, 2006. [ Links ]
11. Nattrass N. Mortal combat: AIDS denialism and the struggle for antiretrovirals in South Africa. University of KwaZulu Natal Press, 2007. [ Links ]
12. Department of Health. National Antiretroviral Guidelines. 2004. [ Links ]
13. Bretz WA, Flaitz C,Moretti A, Corby P, Schneider LG, Nichols CM. Medication usage and dental caries outcome-related variables in HIV/AIDS patients. AIDS Patient Care STDS 2000; 14(10): 549-54. [ Links ]
14. Gehrke FS, Johnsen DS. Bottle caries associated with anti- HIV therapy. Pediatr Dent 1991; 13(1): 73 (letter). [ Links ]
15. Navazesh M, Mulligan R, Barron Y, Redford M, Greenspan D, Alves M, et al. A 4-year longitudinal evaluation of xerostomia and salivary gland hypofunction in the Women's Interagency HIV Study participants. Oral Surg Oral Med Oral Pathol Oral Radiol 2003; 95(6): 693-8. [ Links ]
16. Reznik DA. Oral manifestations of HIV disease. Top HIV Med 2005; 13(5): 143-8. [ Links ]
17. Moniaci D, Cavallari M, Greco D,Bruatto M, Raiteri R, Palomba E, et al. Oral lesions in children born to HIV-1 positive women. J Oral Pathol Med 1993; 22(1): 8-11. [ Links ]
18. Magalhaes MG, Bueno DF, Serra E, Goncalves R. Oral manifestations of HIV positive children. J Clin Pediatr Dent 2001; 25(2): 103-6. [ Links ]
19. dos Santos LC, Castro GF, de Souza IPR, Oliveira RHS. Oral manifestations related to immunosuppression degree in HIV- positive children. Braz Dent J 2001; 12(2): 135-8. [ Links ]
20. Leggott PJ. Oral manifestations of HIV infection in children. Oral Surg Oral Med Oral Pathol 1992; 73(2): 187-92. [ Links ]
21. Khongkunthian P, Grote M, Isaratanan W, Piyaworawong S, Reichart PA. Oral manifestions in 45 HIV positive children from Northen Thailand. J Oral Pathol Med 2001; 30(9): 549-52. [ Links ]
22. Powderly WG, Landay A, Lederman MM. Recovery of the immune system with antiretroviral therapy: the end of opportunism? JAMA 1998; 280(1): 72-7. [ Links ]
23. Patton LL, McKaig R, Strauss R, Rogers D, Eron JJ. Changing prevalence of oral manifestations of human immuno-deficiency virus in the era of protease inhibitor therapy. Oral Surg Oral Med Oral Pathol Oral Radiol 2000; 89(3): 299-304. [ Links ]
24. UNGASS. South Africa UNGASS Country Progress Report, 2010. Available: http://www.unaids.org/en/dataanalysis/monitoringcountryprogress/2010progressreportssubmittedbycountries/southafrica_2010_country_progress_report_en.pdf [Accessed 15 May 2012] . [ Links ]
25. Shiboski CH, Hilton JF, Greenspan D, Westenhouse JL, Derish P, Vranizan K, et al. HIV-related oral manifestations in two cohorts of women in San Francisco. J Acquir Immune Defic Syndr 1994; 7(9): 964-71. [ Links ]
26. Margiotta V, Campisi G, Mancuso S, Accurso V, Abbadessa V. HIV Infection: oral lesions, CD4+ cell count and viral load in an Italian study population. J Oral Pathol Med 1999; 28(4): 173-7. [ Links ]
27. Bravo IM, Correnti M, Escalona L, Perrone M, Brito A, Tovar V, et al. Prevalence of oral lesions in HIV patients related to CD4 cell count and viral load in a Venezuelan population. Med Oral Patol Oral Cir Bucal 2006; 11(1): E33-E39. [ Links ]
28. Greenspan D, Gange SJ, Phelan JA, Navazesh M, Alves M, MacPhail LA, et al. Incidence of oral lesions in HIV-1-infected women: reduction with HAART. J Dent Res 2004; 83(2): 145-50. [ Links ]
29. Ramirez-Amador V, Esquivel-Pedraza L, Sierra-Madero J, Anaya-Saavedra G, Gonzalez-Ramirez I, Ponce-de-Leon S.The changing clinical spectrum of human immunodeficiency virus (HIV)-related oral lesions in 1,000 consecutive patients: a 12-year study in a referral center in Mexico. Bull Sch Med Univ Md 2003; 82(1): 39-50. [ Links ]
30. Flanagan MA, Barasch A, Koeningsberg SR, Fine D, Houpt M. Prevalence of oral soft tissue lesions in HIV-infected minority children treated with highly active antiretroviral therapies. Pediatr Dent 2000; 22(4): 287-91. [ Links ]
31. Flint SR, Tappuni A, Leigh J, Schmidt-Westhausen AM,MacPhail L. Markers of immunodeficiency and mechanisms of HAART therapy on oral lesions. Adv. Dent Res 2006; 19(1): 146-51. [ Links ]
 Correspondence:
Correspondence:
S R Mthethwa
Sefako Makgatho Health Sciences University
PO Box D24, MEDUNSA, 0204
Tel: 012 521 5888, Fax: 012 521 4838
E-mail: Rocky.Mthethwa@smu.ac.za













