Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.70 n.7 Johannesburg 2015
CLINICAL REVIEW
Medical emergencies in dental practices in South Africa
CP QwenI; N MizraII
IMScDent, MChD, FICD, FCD(SA). Professor Emeritus, Department of Oral Rehabilitation, School of Oral Health Science, Faculty of Health Sciences, University of the Witwatersrand
IIBDS, MScDent. Private practice, Durban
SUMMARY
PURPOSE: Studies carried out in many countries have shown that dentists were not confident in managing medical emergencies, and that some did not have any emergency drugs and equipment in their practice or had never had any form of practical training. No studies on the prevalence of medical emergencies for dental practices in South Africa have been published
METHOD: An email survey was carried out. Sample size was calculated to be at least 239, and 267 respondents participated. The questionnaire comprised demographics; equipment and drugs possessed; number of medical emergencies experienced over a 12 month period; self-evaluation on specific medical procedures; and opinions on the need for training of dentists in managing medical emergencies
RESULTS: The results in general agreed with those of similar surveys carried out in other countries, and gave rise to similar concerns, in that there are many practitioners who are clearly ill-equipped to deal with medical emergencies. Most respondents felt they required more formal training
CONCLUSIONS: It is recommended that medical emergency courses should be part of all undergraduate curricula; that medical emergency courses should be included as part of CPD accreditation requirements; and that as there is no South African list of recommended equipment and drugs, this should be developed and regularly revised, most suitably by the South African Dental Association
INTRODUCTION
A medical emergency may occur at any time, and can be life threatening if left or incorrectly treated.1,2,3 In patients with medical conditions, any stress and anxiety associated with a dental visit may increase their risk of having a medical emergency.4 The ability of a dentist to recognise a problem quickly, and initiate treatment, reduces the risk of morbidity and mortality.
According to the American Dental Association (ADA), three out of four practitioners have experienced a medical emergency, and one in twenty general dental practitioners will have a patient with a cardiac arrest in their lifetime.6 Studies carried out in many countries have shown that dentists were not confident in managing medical emergencies, and that some dentists did not have any emergency drugs and equipment in their practice7,8 or had never had any form of practical training in resuscitation.9 In other studies, dentists agreed that there was a need for further training and that hands-on courses would improve their preparedness.10,11
However, a lack of information on the prevalence of medical emergencies can make it difficult to formulate continuous education courses for general dental practitioners.5,8 A search of the literature revealed that there appear to have been no studies on the prevalence of medical emergencies for dental practices in South Africa. Elsewhere, a wide variety of emergency incidents has been reported with much variation as to the most prevalent. It has been pointed out that as the average age of patients is rising in many countries, and that these patients are likely to be on medication for cardiovascular, pulmonary and endocrine disorders, the risk of side effects and acute decompensation is increasing.12
Whatever the prevalence, emergency equipment and drugs should be available. Chapman in 19977 reported that 14% of dentists did not keep any emergency drugs or equipment and Müller et al in 20088 found that 5% of dentists had no equipment to treat emergencies.
Furthermore, a number of studies have shown that dentists did not feel prepared to handle all medical emergencies5,13,14,15 and others have provided evidence of the need for ongoing training in medical emergencies.2,6,12,16 The ADA recommended that as procedures and drugs are continuously being updated, dentists should undergo training at least once a year.6
It is clear from the above that dentists should have the appropriate drugs and equipment in their practices, and the skills to use them, but also need to undergo regular training, to effectively manage medical emergencies that may occur in a dental practice. It is not known to what extent dentists in South Africa conform to such requirements. The aims of this study were therefore to determine the prevalence of medical emergencies in a sample of dentists in private practice and to assess their capacity to deal with such emergencies.
METHOD
A questionnaire* was devised using previous studies, guidelines from the UK Resuscitation Council3 and the Guide to Preparedness for Medical Emergencies from the ADA.6 The latter required dentists to have numerous emergency drugs and equipment available in their dental practices, and this guide was used to draw up the list of emergency equipment and drugs for the questionnaire. Ethical approval was obtained from the Human Research Ethics Committee (M110410).
*The Questionnaire is available from the authors on request.
After a pilot study to validate the questionnaire, it comprised the following parts:
1. Demographics.
2. Emergency drugs and equipment possessed.
3. Number of medical emergencies experienced over a 12 month period.
4. Self-evaluation on specific medical procedures.
5. Opinion on the need for training of dentists in managing medical emergencies.
Respondents were asked to record the number of medical emergencies that had occurred in their dental practices in the past 12 months.
The study population was dentists whose email addresses were provided by the South African Dental Association. There were 2,517 email addresses, the majority of which were in Gauteng. Although it has been reported that email surveys had a lower response rate when compared with postal surveys, time and financial considerations made this more favourable.16 It also enabled a larger geographical area to be accessed with the use of minimum resources. Reminder emails were sent out on four occasions to all the dentists, to improve the response rate. Procedures for determining sample size for continuous and categorical variables using Cochran's formulae17 were used to calculate the sample size based on a study population of 2,517. At a confidence level of 95% and a width of the confidence interval of 5, a sample size of 239 was required.
Inclusion criteria were dentists with a minimum of one year experience in private dental practice and dental specialists. Excluded were maxillo-facial and oral surgeons (it was assumed that they would have had extensive training during post-graduate studies) and dentists working in hospitals and clinics.
Descriptive statistics were used to summarise the demographics, incidence of medical emergencies occurring in private practice, as well as the equipment and drugs used by the dentists in medical emergencies. The average scores, in Part 4 of the questionnaire, were used to determine which statements were the most and least important in the need for training in emergency management.
RESULTS
The final response was 10.5% or 267 respondents. Table 1 shows the location of the practices responding, and Table 2 the experience of the respondents. Eighty four percent (224) of the dentists had been practicing for longer than 5 years. Ninety three percent of respondents were general dental practitioners and 7% were specialists in oral medicine and periodontics (9), orthodontics (8), prosthodontics (7), and there was one community dentist, who was in private practice.
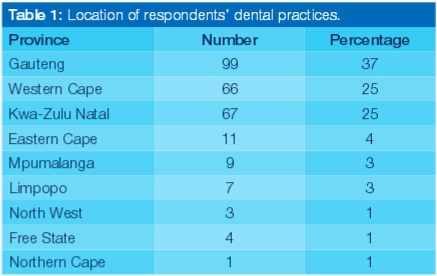
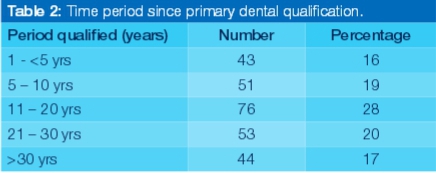
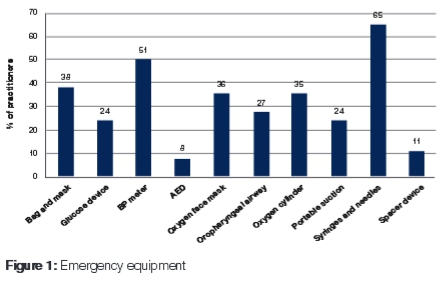
Figure 1 shows the percentages of the recommended emergency equipment which were available in the dental practices. Only three respondents (1%) stated they had all the equipment required in their practice, but 39 respondents (15%) had no equipment to treat medical emergencies. More than half of the respondents had sterile syringes (65%) and blood pressure meters (51%) in their practices. Only 10% (32 respondents) had at least half of the required equipment.
Less than 3% (8) reported that they had all the emergency drugs available in their practices (Figure 2) and 32% (66) had none. Half of the required emergency drugs were available in only 10% (26) of practices.
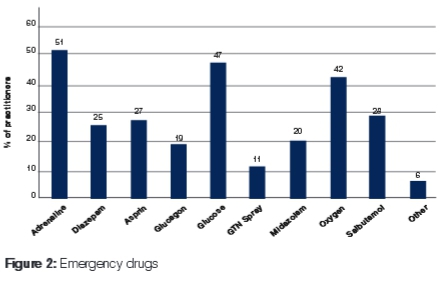
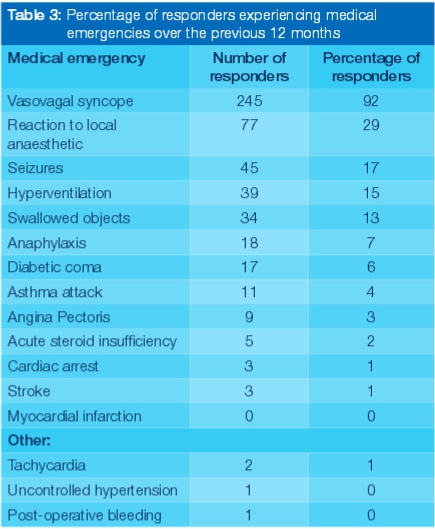
Table 3 shows the reported occurrence of a medical emergency over the previous 12 months. Nineteen percent (52) of respondents had encountered at least one medical emergency and 44% (117) having none. However, 37% (98) had experienced multiple emergencies over that period. Other reported medical emergencies encountered that were not in the questionnaire were tachycardia, uncontrolled hypertension, and post-operative bleeding.
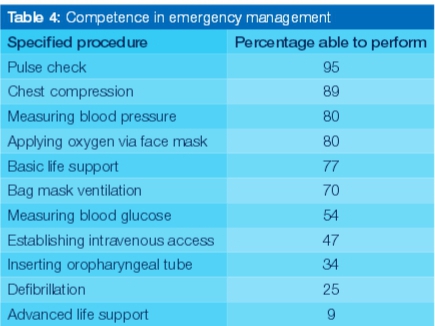
The respondents were given a list of 11 emergency management procedures and were asked to acknowledge whether they were competent in performing each specific procedure (Table 4). Only 9% were able to perform the procedures for Advanced Life Support. One respondent could not perform any of the procedures. In response to whether any respondents had undergone further training, 30% indicated that they had.
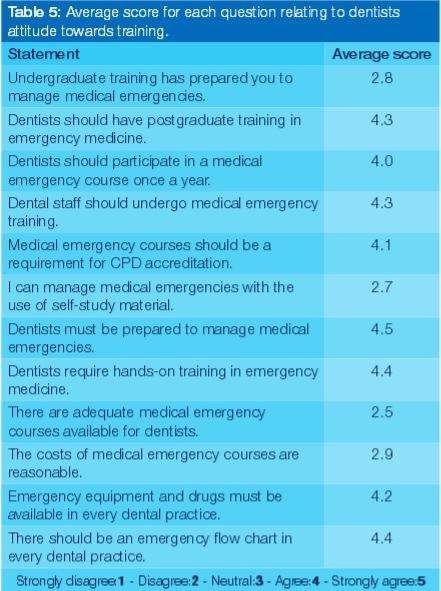
Finally, respondents were requested to rate statements relating to emergency training on a scale of 1 (strongly disagree) to 5 (strongly agree). Averages were then calculated for each statement as shown in Table 5. Scores between 2.5 and 3.0 indicate an overall response to the statement as being neutral, which applied to only four questions. The remaining statements produced an average score above 4.0, indicating that most participants were in agreement or strong agreement with those statements.
DISCUSSION
In the USA, the UK and Australia, medical emergency management procedures are continuously updated by their Resuscitation Councils to ensure the provision of more efficient treatment to patients in a medical emergency. However, this process is not current in South Africa. The lack of a medical emergency programmes for dentists at a post-graduate level could account for the fact that only 30% of the respondents in this study had undertaken any further studies.
Most of the respondents (82%) had more than five years' working experience. It was therefore expected that they had adequate knowledge of practice management, as well as of what drugs and equipment should be kept in their practices. However, 15% had no emergency equipment which is similar to the 14% of Australian respondents.7 A German study8 showed that only 5% of respondents did not have any emergency equipment. Eight percent of current respondents did have a defibrillator, which was favourable in comparison with the German study8 where only 2% owned a defibrillator. A defibrillator is vital for the treatment of patients with cardiac arrests, and South Africa has been ranked the 6th highest country regarding the incidence of cardiac arrest in patients.18 Oxygen tanks (95%) and salbutamol inhalers (70%) were the most common equipment kept in dental practices in Great Britain19 but only 40% of respondents in this South African survey had an oxygen tank.
The most common emergency drug available was adrenaline (51%) followed by glucose (47%) which reflected a much lower adherence than the 77% reported in Great Britain.21 Glyceryltrinitrate spray was reported to have a high level of availability (80%) in Great Britain21 compared with only 11% in South African respondents.
Overall, it appears that it is likely that dentists in South Africa have less emergency equipment and drugs when compared with dentists in Great Britain,21 Australia7 and Germany.8 A lack of basic equipment and drugs places dentists at a high risk of having a mortality or serious morbidity in their dental practice.
The most common medical emergency was syncope, reported by 92% of the respondents, and this was also the most common emergency in Northern England,5 Australia7 and Japan1 where the figures were 63%, 58% and 50% respectively. The next most common emergency experienced was the reaction to local anaesthetic (29%). Atherton et al in 199920 stated that 20% of medical emergencies occurred after the administration of local anaesthetics. Thus dentists need to have appropriate resuscitative equipment in their practices. Seventeen per cent of the respondents experienced patients with seizures. This condition requires anti-epileptic drugs such a midazolam for treatment which was stored by only 20% of the respondents.
Cardiac arrest of a patient was experienced by three of the respondents over the previous 12 months. All three dentists had blood pressure meters, sterile syringes and needles, and glucose but only one had the necessary additional equipment and drugs. Whilst 25% of respondents felt that they were able to perform defibrillation, only 8% had a defibrillator, which is the most important equipment required to restore a normal heart rhythm. If defibrillation is not provided, the patient can die within minutes.13 Balmer in 20 0821 stated "Dental undergraduates must understand the different cardiac arrest rhythms and be trained in the safe use of an AED". An alarming statistic published by Louw et al22 reported that less than half (49%) of general medical practitioners working in hospitals in the Western Cape knew the indications for defibrillation. Of concern also, is that procedures such as performing airway management (inserting an oropharyngeal tube) and establishing intravenous access were able to be carried out by only 34% and 25% respectively of respondents.
It was clear from the responses (Table 5) that the respondents felt they required more formal training. A New Zealand study stated that more than half their respondents were dissatisfied with the training they had received for medical emergencies as undergraduate students.11 The results from this study, however, showed that the respondents were neutral to whether undergraduate training prepared them for medical emergencies.
The respondents clearly felt strongly about the need for being prepared to manage medical emergencies, and that training is an important part of ensuring continued success in treating patients in such circumstances. They were uncertain or neutral to the statements which implied that there are insufficient training courses available or that dentists are unaware of training courses that could prepare them for medical emergencies. Standardising and certifying emergency training would certainly improve the competency level of dentists and prepare their staff in managing such situations.
CONCLUSION AND RECOMMENDATIONS
There were some limitations in this study, as there are in surveys of this nature, such as the uneven geographic distribution of the respondents, and the inherent biases in such a sample in that only those practitioners with access to email and interested enough in the topic would have responded. However, the results in general seem to agree with those of similar surveys carried out in other countries, and give rise to similar concerns as expressed in those studies, in that there are many practitioners who are clearly ill-equipped to deal with medical emergencies. The following recommendations are therefore made:
1. Medical emergency courses should be part of all undergraduate curricula
2. Medical emergency courses should be included as part of CPD accreditation requirements by the Health Professions Council of South Africa.
3. As there is no South African list of recommended equipment and drugs, this should be developed and regularly revised, most suitably by the South African Dental Association.
Acknowledgments: We are grateful to Dr V Karic for the inspiration of this study and its inception.
References
1. Haas DA. Management of medical emergencies in the dental office: Conditions in each country, the extent of treatment by the dentist. Anesth Prog 2006; 53:20-4. [ Links ]
2. Regina MC, Luciane RC, Vänia CM. Brazilian dental students' perceptions about medical emergencies: A qualitative exploratory study. J Dent Educ 2008; 72:1343-9. [ Links ]
3. Greenwood M. Medical emergencies in dental practice: I.The drug box, equipment and general approach. SADJ 2009; 64:246-52. [ Links ]
4. Malamed SR Medical emergencies in the dental office, 5th ed, St Louis: Mosby 2000 [ Links ]
5. Girdler NM, Smith DG. Prevalence of emergency events in British dental practice and emergency management skills of British dentists. Resuscitation 1999; 41:159-67. [ Links ]
6. ADA Council of Scientific Affairs. Office emergencies and emergency kits. J Am Dent Assoc 2002; 133:364-5. [ Links ]
7. Chapman PJ. Medical emergencies in dental practice and choice of emergency drugs and equipment: A survey of Australian dentists. Aust Dent J 1997; 42:103-8 [ Links ]
8. Müller MP, Hansel M, Stehr SN, Weber S, Koch T. A state wide survey of medical emergency management in dental practices: incidence of emergencies and training experience. Emerg Med J 2008; 25:296-300. [ Links ]
9. Gonzaga F, Buso L, Jorge MA, Gonzaga L, Chaves MD, Almeida OP. Evaluation of knowledge and experience of dentists of Säo Paulo State, Brazil about cardiopulmonary resuscitation. Braz Dent J 2003; 14:220-2 [ Links ]
10. Atherton GJ, Pemberton, Thornhill MH. Medical emergencies: the experience of staff of a UK dental teaching hospital. Br Dent J 2000; 188:320-4. [ Links ]
11. Broadbent JM, Thomson WM. The readiness of New Zealand general dental practitioners for medical emergencies. N Z Dent J 2001; 97:82-6. [ Links ]
12. Mutzbauer TS, Rossi R, Ahnefeld FW, Sitzmann F. Emergency medical training for dental students. Anesth prog 1996; 43:37-40. [ Links ]
13. Atherton GJ, McCaul JA, Williams SA. Medical emergencies in general dental practice in great Britain Part 3: perceptions of training and competence of GDPs in their management. Br Dent J 1999b; 186:234-7. [ Links ]
14. Arsati F, Montalli V A, Flório F M, Ramacciato JC, Lopes da Cunha F et al. Brazilian dentists' attitudes about medical emergencies during dental treatment. J Dent Educ 2010; 71:661-6. [ Links ]
15. Amirchaghmaghi M, Sarabadani J, Delavarian Z, Mozafary PM, Shahri A, Dalirsani Z. The knowledge and preparedness of General Dentists about Medical Emergencies in Iran. Iran Red Crescent Med J 2010; 13:217-8. [ Links ]
16. Leece P, Bhandari M, Sprague S, Swiontkowski MF, Schemitsch EH, Tornetta P, Devereaux PJ, Guyatt G. Internet versus mailed questionnaires: A controlled comparison (2). J Med Internet Res 2004; 6:e39. [ Links ]
17. Bartlett JE, Kortlik J, Higgins C. Organizational Research: Determining appropriate sample size in survey research. Information Technology, Learning, and Performance Journal 2001; 19:43-50. [ Links ]
18. World Health Organization 2004. Statistical Information System, Cardiac arrest by country, http://www.NationMaster.com. Accessed on 14 November 2012. [ Links ]
19. Atherton GJ, McCaul JA, Williams SA. Medical emergencies in general dental practice in great Britain Part 2: drugs and equipment possessed by GDPs and used in the management of emergencies. Br Dent J 1999a; 186:125-30. [ Links ]
20. Atherton GJ, McCaul JA, Williams SA. Medical emergencies in general dental practice in great Britain Part 1: their prevalence over a 10-year period. Br Dent J 1999; 186:72-9. [ Links ]
21. Balmer MC. A dental undergraduate course for the management of medical emergencies in dental practice. Eur J Dent Educ 2008; 12:239-46. [ Links ]
22. Louw P, Maritz D, Wallis L. Emergency centres lack defibrillator knowledge. S Afr Med J 2010; 100:435-6. [ Links ]
 Correspondence:
Correspondence:
CP Owen
Departmentof Oral Rehabilitation
School of Oral Health Science
Faculty of Health Sciences
Unversity of the Witwatersrand
7 York Road, Parktown, 2193
Tel: 011 488 4861
Fax: 086 553 4800
Cell: 083 679 2205













