Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.70 no.7 Johannesburg 2015
RESEARCH
The knowledge, attitude and practice of edentulous patients attending a dental institute in India regarding care of their dental prostheses
K ShigliI; M HebbalII; S SajjanIII; N AgrawalIV
IProfessor and Head, Department of Prosthodontics, Bharati Vidyapeeth Deemed University Dental College and Hospital, Sangli, Maharashtra
IIProfessor, Department of Public Health Dentistry, K.L.E.V.K. Institute of Dental Sciences, Belgaum, Karnataka
IIIProfessor and Head, Department of Prosthodontics, Vishnu Dental College, Bhimavarum, Andhra Pradesh
IVAssistant Professor, Department of Periodontics and Community Dentistry, Dr. Z A Dental College, AMU, Aligarh
ABSTRACT
AIM: The role of a dentist does not end with the placement of the prosthesis, for the care of the denture is equally important. This study aimed to assess knowledge, attitude and practice regarding care of complete dentures
METHODS: The sample comprised 192 complete denture patients visiting the Department of Prosthodontics. A questionnaire assessed their socio-demographic status (Kuppuswamy's socio-economic classification), denture use, denture cleaning and knowledge of denture care. Data was subjected to descriptive statistical analysis
RESULTS: 69.8% patients had only one set of complete dentures; 77.1% and 25.5% patients removed their dentures at night and during the day respectively. All reported cleaning their prostheses daily; 94.7% patients employed a tooth brush, 5.3% used denture brush and 3.6% used denture cleansers. 35.9% patients did not know about the estimated life expectancy of complete dentures and only 10.9% patients had knowledge of items to be avoided to prevent staining of dentures
CONCLUSION: Instruction on how to care for complete dentures should be given special attention by the dentists during insertion. Follow up and reinforcement of denture home care should be done periodically to ensure durable performance of dentures as well as maintenance of good oral health
Key words: Knowledge, Attitude, Complete Denture, Denture maintenance.
INTRODUCTION
The proportion of older people in the population is increasing faster than is any other age group.1 India will soon become home to the second largest number of older people in the world.2 The number of people in the 60-plus age group in India is expected to increase to 100 million in 2013 and to 198 million by 2030.3 This increase in life expectancy can be attributed to improved medical facilities and the dental needs of this section of the population require special attention.4
A dental prosthesis should restore aesthetics and function. The quality of the prosthesis needs to be regularly monitored as it functions within a changing oral environment comprising the saliva, the oral musculature and the supporting tissues. Microbial plaque on dentures has the potential to be harmful to both the oral mucosa and to general health.5,6 The microporous surface of an acrylic resin denture base provides an environment that harbours opportunistic microorganisms. Denture cleaning is necessary to remove such invaders, as well as extrinsic stains and soft and hard deposits.5
The role of dentists does not end with the placement of the prosthesis. Measures must be taken to ensure that any dental prosthesis is properly taken care of by the patient, thereby contributing to the health of the foundation area, the supporting tissues and to the success of the treatment.7 A neglected dental prosthesis not only represents a lack of patient knowledge but also highlights a potential lack of motivation on the part of the dentist.
However, many complete denture patients tend to think that being in the state of edentulism does not require any specific oral hygiene measures and do not return to the dentist for regular denture maintenance.8 Therefore, in the endeavour to assess the extent of this problem, the present study was carried out to assess the knowledge and attitude of denture-wearing patients as well as practices related to the care of dental prostheses.
MATERIALS AND METHODS
Participants were selected from amongst the completely edentulous patients attending the Department of Prostho-dontics, Modern Dental College and Research Centre, In-dore, Madhya Pradesh, India from March to October 2011.
Ethical clearance was obtained from the Institute before starting the study. The patients who fulfilled the following inclusion criteria were considered for the study: completely edentulous patients with at least two months of denture wearing who had given informed consent for their inclusion in the study. All the patients were independent, hence no other person was involved in the maintenance of denture hygiene. Patients were excluded if they had limited mental or physical abilities and if they were wearing a single complete denture. A questionnaire, was designed to assess the socio-demographic status, denture use, denture cleaning and denture home care knowledge of the patient.
Socio-demographic status included personal details, habit history and Kuppuswamy's socioeconomic classification9 (which takes into account the level of education, monthly income and occupation) was used to determine the socioeconomic status of the patients.
The following data were collected: the age of the patient, the number of previous sets of dentures, the frequency of replacing dentures, nocturnal denture wear, denture removal during day, how the dentures were stored, denture-related ulceration, use of adhesives, presence of other denture wearers in the family and the history of any denture repairs.
With regard to denture cleaning the following data were recorded: the schedule of cleaning the dental prostheses, if it was performed within or outside the mouth, the use of tooth/denture brush or other cleaning aids, perception after wearing the cleaned denture and whether denture polishing was ever carried out.
The patients' knowledge on the life expectancy of complete dentures, and their knowledge of food items that may cause denture staining was recorded. Questionnaire by Barbosa et al.10 was modified according to Indian scenario and used for the study. A pilot study on ten patients was carried out to check the feasibility of the study and the questions were modified accordingly.
A single trained investigator (K. S.) recorded the answers to the questionnaire. The data was compiled and subjected to descriptive statistical analysis.
RESULTS
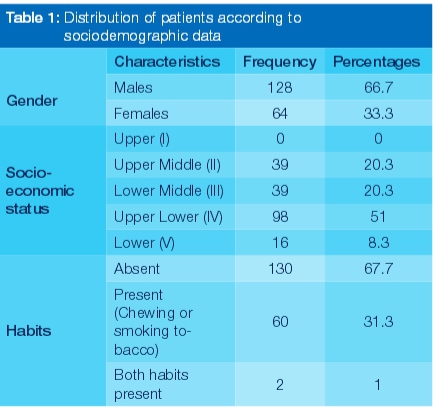
A total of 192 patients participated in the study and included 66.7% males and 33.3% females. The age range was 38-95 years (mean age 64.55). 51% of the patients were categorized as having upper lower socioeconomic status, 20.3% as the upper middle and lower middle whilst 8.3% were placed in the lower socioeconomic status. 67.7% of the patients in the study did not have smoking or tobacco chewing habits (Table 1).
48.4% patients had been using dentures for more than one year but less than 5 years and 33.9% for more than 5 years. 69.8% patients reported using only one set of complete dentures and 1.6% had a history of having five sets of complete dentures. Of the 58 patients who reported using more than one set, 60.3% patients reported changing their dentures within five years. 77.1% removed their dentures at night, and of these 148 patients, 89.9% kept their prostheses in water, 4.1% in an empty box, and 6.1% either tied the dentures in a cloth, or placed them in a pocket or on a table. Of the surveyed population, 25.5% removed their prostheses during the day while 74.5% did not. Among the 49 patients who removed the prostheses during the day 71.4% kept the teeth in water. 76.6% patients did not report ulceration with dentures. Most of the patients (94.3%) did not use denture adhesive. The majority of the patients did not have a family member who was also a denture wearer. The dentures of 58 (30.2%) patients had been repaired and of these, 41.4% reported fracture of the mandibular denture (Table 2).
All 192 patients reported cleaning their prostheses daily, and 86.5% of the sample cleaned the prostheses outside the mouth. 53.6% cleaned the prostheses twice a day. Of the 150 patients using a brush, 94.7% patients employed a tooth brush to clean the prostheses whereas a denture brush was used by 5.3%. The most popular cleaning aids were toothpaste 26.6%, soap 25% and denture cleanser 3.6%. Other aids used included tooth powder, salt and lemon, ash and bleaching liquid. 58.3% patients could appreciate the difference when wearing clean dentures, and "feeling clean" was reported by 89.3% of these 112 patients. None of the 192 patients had their dentures polished by a dentist (Table 3). There was a statistically significant relationship between gender and frequency of denture cleaning (p=.007). There was a statistically nonsignificant difference between social class and frequency of denture cleaning (p=0.072).
35.9% of the sample did not know for how many years a denture should be used. 56.3% of the patients were self taught regarding the maintenance of their dentures. 10.9% of the patients knew what items had to be avoided to prevent staining of dentures and 38.1% attributed staining to tobacco (Table 4).
DISCUSSION
Complete denture wearers should be educated regarding prostheses care and maintenance to ensure health and function of the supporting structures. This study assessed edentulous patients' knowledge, attitude and practice regarding care of their complete denture prostheses.
The present study showed that 33.9% patients had been using the same complete dentures for more than 5 years in comparison with the results of Chowdhary et al.11and Barbosa et al.10who have, respectively, reported 8% and 78% usage of the same complete dentures for more than 5 years. Chowdhary et al. conducted the study in 125 complete denture wearers at HKES S Nijalingappa Institute of Dental Science, Gulbarga, Karnataka, India while Barbosa et al. surveyed 150 complete denture wearers at the Federal University of Bahia School of Dentistry, Brazil. The considerable difference in the findings of the two studies may be attributable to variation in the sample populations.
69.8% patients reported using only one set of complete dentures during their life. The remaining patients used more than one set, 60.3% reported changing their dentures within five years and 1.7% reported changing dentures after using them for more than 25 years. This is in stark contrast to a study by Nevalainen et al.12which found 64% subjects had a denture -wearing history of over 30 years. The disparity may be related to the age of the patients as the latter study was conducted on the elderly, over 75 years. Older denture wearers manage well with their dentures and are often reluctant to obtain a new set.12 This may be an indirect measure of an opportunity for a dentist to educate his/her patients regarding denture care.
Of the surveyed population 22.9% patients did not remove their dentures at night which is a finding close to the report of a previous study by Chowdhary et al.11, where 36% slept with their prostheses in place. However, other studies found that most of their patients wore their dentures through the night.8,10 Patients may fear that removal of dentures may result in collapse of the facial tissues.14
There is agreement of the important need to leave dentures out of the mouth for a minimum of six of every 24 hours to ensure regenerative blood supply, a relief of pressure and a break in parafunctional habits to allow the tissues to recover.15-18
Most of those who slept without their dentures kept them in water, a finding similar to that reported by Barreiro et al. This may demonstrate that patients knew that this practice avoided dimensional changes of the acrylic resin due to dehydration.13
This study found that a quarter (25.5%) of the patients removed their dentures during the day. Barbosa et a/. and Chowdhary et al. recorded much higher incidences of this habit (54% and 67.2% respectively). Among those who did take out their dentures during the day, 71.4% placed them in water, a finding disparate from previous studies which had reported an incidence of 35.2% and 86.5% respectively.10,11
Chowdhary et al. had recorded a relatively high occurrence of ulceration related to dentures (50.4%), whilst this study found that most patients had not suffered this problem.
Denture adhesive was used by 4.7% patients, somewhat more than had required this aid in another study (1.3%)10 but less than the 14.5% found by Chowdhary et al.11 Extended use of denture adhesives should not be considered without periodic assessment of denture quality and health of the supporting tissues by a prosthodontist.19
The lack of awareness regarding the care of the prostheses among most of the patients may possibly be due to their not having a denture-wearing family member with whom to share experiences.
Most of the patients in this study had never required to have their dentures repaired. The few who did had mainly experienced fractures of the mandibular denture, a finding consonant with results reported by Naik.20 The smaller surface area of the mandibular denture and patient negligence during insertion, removal and cleaning are the contributory factors most responsible.20
All patients reported cleaning their dentures daily. The results are similar to those reported in the literature (more than 70% cleaned their dentures daily).8,10,11,21-23 Most patients cleaned their dentures twice a day which is similar to the findings of Chowdhary et al.11 and Barbosa et al.10 where (majority of patients cleaned their prostheses once a day and three or more times a day respectively). This frequency of denture cleaning would not, however, necessarily indicate clean prostheses.24 Almost all patients employed a tooth brush to clean the denture, as also recorded by Chowdhary et al.11
and Barbosa et al.10 A denture brush was used by only 5.3% patients. Superior cleansing could be expected with a brush specifically designed for complete dentures.25 The majority of the patients used tooth paste to clean the dentures in common with other reported data.8,10,11,22,26 Patients reported using tooth powder, salt, lemon, ash and bleaching liquid to clean their prostheses probably because these are cheap and easily available.10
It is generally understood that abrasives in tooth paste would abrade the dentures. However a study by Himabindu et al.27 showed that the soap and brush method abraded the denture more than did the tooth paste. Hence the use of tooth paste with brush could be suggested. Brushing in combination with a chemical cleansing agent can be employed as an efficient method of daily denture care.28 Patients should be encouraged to brush their dentures thoroughly after each meal or snack, outside the mouth, with a brush followed by rinsing under a tap.14 Cleansing of the intaglio (tissue contacting) surface of the denture should receive special attention during instruction on denture maintenance.25 Inaccessible areas on the intaglio surface may require the use of cottonwool swabs or a modified artist's brush to effectively remove plaque and food debris.14 On retiring at night, dentures should be brushed and immersed overnight in a denture-cleansing solution.28,14 The edentulous ridges should be thoroughly massaged once per day.14
Most of the patients did not use denture cleansers, also reported elsewhere.13 This could be attributed to economic reasons or a limited knowledge of denture cleansers. Shet-ty et al.29 suggested the use of natural products like Triphala Churna (an Ayurvedic product made from three fruits) for denture cleaning to overcome the problem of economics.
The majority appreciated the difference after wearing clean dentures which were perceived as odourless and closely adhering to the palate. None of the patients had their dentures polished by a dentist, even after using them for some years. Although the evidence is weak, dentures should be cleaned annually by a dentist using ultrasonic cleansers to minimize biofilm accumulation over time.19
Education of the denture-wearing patients is important.21 Unclean dentures may cause halitosis, inflammatory changes of the oral mucosa such as denture-induced stomatitis and also poor esthetics.6,22,30-33 Therefore, it is important for dentists to educate their patients about denture cleanliness and to stress the need for frequent recall visits.22
The majority of the patients did not know how long a complete denture should be used. Complete dentures should be reviewed annually, with consideration for replacement after five years.33 The majority of the patients attributed the knowledge of denture maintenance to themselves. Whilst the patient may have forgotten instructions imparted orally, or not followed them, the dentist may have been negligent in not ensuring compliance.32 Printed information for reference and frequent reinforcement is desirable.34
Very few patients had knowledge of which items should be avoided to prevent staining of dentures. Most attributed the cause of denture staining to tobacco usage. Extrinsic staining of acrylic resin dentures can be a major problem for many individuals especially those who smoke tobacco products or drink tea, coffee, cola or red wine. A survey of patients with complete dentures showed that drinking tea and coffee was the main cause of the denture staining.5
It could be advantageous to use the "Tell Show and Do" technique in which the dentist demonstrates the techniques of denture cleaning and the patient should be asked to repeat the process in the presence of the dentist.24 Special care should be taken to reinforce this information at regular intervals, perhaps by developing support groups to educate edentulous patients by conducting seminars and workshops.35
To summarize: the patients exhibited limited knowledge regarding care of the dentures. The majority of the patients employed a tooth brush to clean the denture and did not use denture cleansers. Most of the patients were not aware of the life span of a complete denture and attributed the knowledge of denture maintenance to themselves. Very few patients had knowledge of items to be avoided to prevent staining of dentures.
CONCLUSION
Dentists need to be more cognizant of the need to offer denture patients greater support. Instruction on how to care for complete dentures should be given special attention by the dentists during insertion. Follow up and reinforcement of denture home care should be done periodically to ensure durable performance of dentures as well as maintenance of good oral health. More attention must be given to training dental students in the education and motivation of patients regarding denture care and maintenance.
Acknowledgements
The authors would like to acknowledge:
• Dr N.S. Azhagarasan, Professor and Head, Department of Prosthodontics, Ragas Dental College and Hospital, Chennai, Tamil Nadu, for developing the questionnaire.
• Dr Gangadhar Shivappa Angadi, Professor and Head, Department of Prosthodontics, Rural Dental College, Loni, Maharashtra; Dr Chandrashekharan Nair, Professor and Head, Department of Prosthodontics, AECS Maaruti College of Dental Sciences and Research Centre, Bangalore, Karnataka, for valuable inputs to the manuscript.
• Dr Puneet Gupta, Research Consultant; Dr Vikneshan,Senior Lecturer, Department of Public Health Dentistry, Sri Sankara Dental College, Varkala, for carrying out the statistical analysis
• Dr K.P. Suresh, Scientist (Bio-statistics), National Institute of Animal Nutrition & Physiology (NIANP), Bangalore, Karnataka for assistance in coding data.
References
1. Petersen PE, Yamamoto T. Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 2005; 33: 81-92. [ Links ]
2. Kumar A, Srivastava DK, Verma A, Kumar S, Singh NP, Kaushik A. The problems of fall, risk factors and their management among geriatric population in India. IJCH 2013; 25:89-94. [ Links ]
3. http://timesofindia.indiatimes.com/home/science/Loneliness-not-obesity-biggest-killer-of-elderly/articleshow/30589605. cms accessed on 29th July, 2014. [ Links ]
4. Talwar M, Chawla HS. Geriatric dentistry: Is rethinking still required to begin undergraduate education? Indian J Dent Res 2008; 19:175-7. [ Links ]
5. Alam M, Jagger R, Vowles R, Moran J. Comparative stain removal properties of four commercially available denture cleaning products: an in vitro study. Int J Dent Hygiene 2011; 9:37-42. [ Links ]
6. Shay K. Denture hygiene: A review and update. J Contemp Dent Pract 2000; 1:28-41. [ Links ]
7. Shigli K. After-care of the complete denture patient. J Prostho-dont 2009; 18:688-93. [ Links ]
8. Peracini A, Andrade IM, Paranhos Hde F, Silva CH, de Souza RF. Behaviors and hygiene habits of complete denture wearers. Braz Dent J 2010; 21: 247-52. [ Links ]
9. Patro BK, Jeyashree K, Gupta PK. Kuppuswamy's Socioeconomic Status Scale 2010-The need for periodic revision. Indian J Pediatr 2012; 79(3):395-6. [ Links ]
10. de Castellucci Barbosa L, Ferreira MR, de Carvalho Calabrich CF, Viana AC, de Lemos MC, Lauria RA. Edentulous patients' knowledge of dental hygiene and care of prostheses. Gerod-ontology 2008; 25:99-106. [ Links ]
11. Chowdhary R, Chandraker NK. Clinical survey of denture care in denture-wearing edentulous patients of Indian population. Geriatr Gerontol Int 2011; 11:191-5. [ Links ]
12. Nevalainen MJ, Rantanen T, Närhi T, Ainamo A. Complete dentures in the prosthetic rehabilitation of elderly persons: five different criteria to evaluate the need for replacement. J Oral Rehabil 1997; 24:251-8. [ Links ]
13. Barreiro DM, Scheid PA, May LG, Unfer B, Braun KO. Evaluation of procedures employed for the maintenance of removable dentures in elderly individuals. Oral Health Prev Dent 2009; 7: 243-9. [ Links ]
14. Penhall B. Preventive measures to control further bone loss and soft tissue damage in denture wearing. Aust Dent J 1980; 25(6):319-24. [ Links ]
15. Wendt DC. How to promote and maintain good oral health in spite of wearing dentures. J Prosthet Dent 1985; 53:805-7. [ Links ]
16. Tarbet WJ. Denture plaque: quiet destroyer. J Prosthet Dent 1982; 48: 647-52. [ Links ]
17. Duncan JP, Taylor TD. Simplified complete dentures. Dent Clin N Am 2004; 48:625-40. [ Links ]
18. Marcus PA, Joshi A, Jones JA, Morgano SM. Complete eden-tulism and denture use for elders in New England. J Prosthet Dent 1996; 76:260-6. [ Links ]
19. Felton D, Cooper L, Duqum I, Minsley G, Guckes A, Haug S et al. Evidence-based guidelines for the care and maintenance of complete dentures. J Am Dent Assoc 2011; 142:1 S-20S. [ Links ]
20. Naik AV. Complete denture fractures: A clinical study. J Indian Prosthodont Soc 2009; 9:148-50. [ Links ]
21. Hoad-Reddick G, Grant AA, Griffiths CS. Investigation into the cleanliness of dentures in an elderly population. J Prosthet Dent 1990; 64:48-52. [ Links ]
22. Dikbas I, Koksal T, Calikkocaoglu S. Investigation of the cleanliness of dentures in a university hospital. Int J Prosthodont 2006; 19:294-8. [ Links ]
23. Navabi N, Gholamhoseinian A, Baghaei B, Hashemipour MA. Risk factors associated with denture stomatitis in healthy subjects attending a dental school in Southeast Iran. Sultan Qa-boos Univ Med J 2013; 13:574-80. [ Links ]
24. Nevalainen MJ, Närhi TO, Ainamo A. Oral mucosal lesions and oral hygiene habits in the home-living elderly. J Oral Rehabil 1997; 24:332-7. [ Links ]
25. Paranhos HFO, Silva-Lovato CH, Souza RF, Cruz PC, Freitas KM, Peracini A. Effects of mechanical and chemical methods on denture biofilm accumulation. J Oral Rehabil 2007; 34:606-12. [ Links ]
26. Takamiya AS, Monteiro DR, Baräo VA, Pero AC, Compagnoni MA, Barbosa DB. Complete denture hygiene and nocturnal wearing habits among patients attending the Prosthodontic Department in a Dental University in Brazil. Gerodontology 2011; 28:91-6. [ Links ]
27. Himabindu K, Chandrasekharan Nair K, Jayakar Shetty. Effect of different tooth brushes and tooth pastes on the surface roughness of denture base acrylic resin. TPDI 2011; 2:27-9. [ Links ]
28. Nikawa H, Hamada T, Yamashiro H, Kumagai H. A review of in vitro and in vivo methods to evaluate the efficacy of denture cleansers. Int J Prosthodont 1999; 12:153-9. [ Links ]
29. Shetty PJ, Hegde V, Gomes L. Anticandidal efficacy of denture cleansing tablet, Triphala, Aloe vera, and Cashew leaf on complete dentures of institutionalized elderly. J Ayurveda In-tegr Med 2014; 5(1):11-4. [ Links ]
30. Abelson DC. Denture plaque and denture cleansers. J Pros-thet Dent 1981; 45:376-9. [ Links ]
31. Adeymi AA, Jarad F, Pender N, Higham SM. Assessing the efficacy of denture cleaners with quantitative light-induced fluorescence (QLF). Eur J Prosthodont Restor Dent 2007; 15:165-70. [ Links ]
32. Jagger DC, Harrison A. Denture cleansing--the best approach. Br Dent J 1995; 178:413-7. [ Links ]
33. Cabot LB, Roberts BJ. Aftercare for the complete denture patient. Br Dent J 1984; 157:72-5. [ Links ]
34. Bauman R. Survey of dentists' attitudes regarding instructions for home care for patients who wear dentures. J Am Dent Assoc 1980; 100:206-8. [ Links ]
35. http://www.essindia.org/about_us.html accessed on 29th July, 2014. [ Links ]
 Correspondence:
Correspondence:
K Shigli
B-1, Staff Quarters
Bharati Vidyapeeth Dental College and Hospital
Sangli-Miraj Road,Wanlesswadi, Sangli-416416
Maharashtra, India
E-mail: kamalshigli@yahoo.co.in













