Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.70 no.5 Johannesburg Jun. 2015
RADIOLOGY CASE
Maxillo-facial radiology case 132
CJ Nortjé
Faculty of Dentistry, University of the Western Cape. E-mail: cnortje@uwc.ac.za
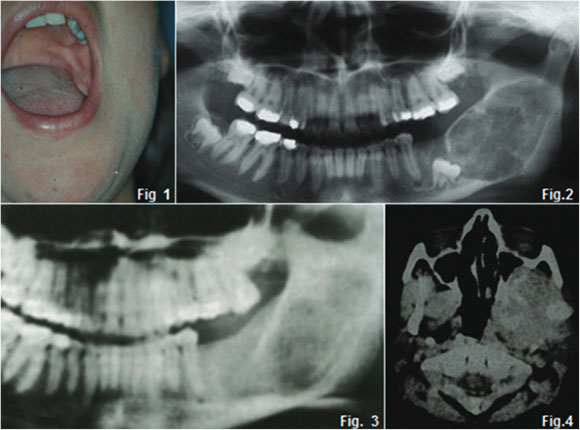
A sixteen year old female with a six year history of discomfort and pain in the left body and angle of the mandible during which time the first and second molar teeth had been extracted. Prior dental records including radiographs were not available. She had a slight clinical swelling of the left cheek (Fig. 1) Intra-oral examination revealed both buccal and lingual expansion of the mandible in the retromolar area. No lymphadenopathy was detected.1
INTERPRETATION
The pantomograph (Fig. 2) shows a well demarcated ovoid radiolucent lesion in the left body and ascending ramus of the mandible features consistent with a benign neoplasm. The unerupted third molar was displaced mesially. Anincisionalbiopsy was carried out and a histological diagnosis of chondromyxoid fibroma was made. When the tumour was removed, an easily discernible dissection plane was found and the surgeon did not have the clinical impression of malignancy. The whole area was thoroughly curetted. Histological examination of the excised specimen confirmed the initial biopsy. There were no signs of recurrence at follow-up until three years later, when the patient presented with a swelling in the same area as previously. There was no lymphadenopathy. Radiographs showed a radiolucent lesion in the same area, but with less demarcation than the initial lesion (Fig. 3). A hemimandibulectomy was performed and a vitallium splint inserted. At this stage a diagnosis of a mesenchymal chondrosarcoma was made. However, regular follow-up examinations revealed no signs of recurrence. Four years later she presented with an extensive swelling in the same area, stretching from under the skin of the left cheek to bulge into the left pharyngeal wall; it was also palpable in the suprahyoid and infratemporal regions. She was complaining of pain in this area as well as her lower back. CT showed a mass which had invaded the left maxillary sinus with destruction of its lateral wall and erosion of the lateral pterygoid plate and cranial base in the region of foramina ovale and spinosum (Fig 4). Scintigraphy revealed areas on increased uptake in the lungs and tenth thoracic vertebra. A biopsy of the affected vertebra revealed a mesenchymal chondrosarcoma with a chondromyxoid appearance in some areas. Treatment with Adriamycin combined with radiation therapy commenced but she died three years later when autopsy confirmed multiple metastases. Two major possibilities exist to explain in the course of this patient (1) a malignant transformation occurred in a correctly diagnosed chodromyxoid fibroma or (2) the initial biopsy represented a chondrosarcoma with foci similar to chondrosarcoma. Chondrosarcomas may be underdiagnosed with some frequency. Weiss and Bennet2 found that chondrosacomas in the head and neck region occur commonly in the mandibular molar area, so one should be most cautious of apparently benign cartilaginous tumour. A disturbing factor in this case for me personally is the six years of discomfort and pain the patient originally experienced. It is very important that a diagnosis is made as soon as possible when a patient presents with pain and discomfort.
References
1. F W Grotepass, G Wyma, C J Nortje and A G Farman: Chondrosarcoma initially diagnosed as a chondromyxoid fibroma: malignant transformation, Dentomaxillofac.Radiol 17: 139-43, 1988. [ Links ]
2. W W Weiss and J A Bennett: A Chondrosarcoma, a rare tumor of the jaws. J Oral Maxillofac Surg 44: 73-9, 1986. [ Links ]













