Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Dental Journal
versión On-line ISSN 0375-1562
versión impresa ISSN 0011-8516
S. Afr. dent. j. vol.70 no.5 Johannesburg jun. 2015
CLINICAL COMMUNICATION
Thirty six years of periodontal care: A case report
A VolchanskyI; WG EvansII; P Cleaton-JonesIII
IBDS PhD. Department of Oral Medicine and Periodontology, School of Oral Health Sciences, University of the Witwatersrand, Johannesburg
IIBDS Dip Orth. Department of Orthodontics, and Paediatric Dentistry, School of Oral Health Sciences, University of the Witwatersrand, Johannesburg
IIIMB BCh, PhD, DSc(Dent). Steve Biko Centre for Bioethics, School of Clinical Medicine, University of the Witwatersrand, Johannesburg
ABSTRACT
INTRODUCTION: In 1978 a 15 year old male was referred to a periodontal practice complaining of bleeding gums.
CASE PRESENTATION: There was Necrotizing Ulcerative Gingivitis (NUG) (called Vincent's Infection at the time) superimposed upon Altered Passive Eruption (APE; then termed Delayed Passive Eruption). Immediate treatment was a course of Metronidazole followed by scaling and oral hygiene instruction. In 1981 a gingivectomy was carried out around the maxillary incisors and canines. The patient has been seen thereafter at intervals for oral hygiene care, prophylaxis and scaling (SPT; Supportive Periodontal Treatment) most recently in 2014.
CONCLUSION: The potentially devastating effects of NUG combined with APE were successfully managed and oral health has subsequently been maintained through a programme of regular periodontal care. APE may be a predisposing factor to NUG, an acute necrotic lesion which, provided there are no systemic compromising complications, responds well to anti-microbial therapy combined with professional plaque and calculus removal, improved oral hygiene and meticulous home care.
CASE PRESENTATION
In August 1978 a fifteen year old male was referred to a periodontal practice. His main complaint was swollen, bleeding gums, a problem which had persisted for the past 18 months. On consulting the patient's father, it was established that there was no relevant medical history, or known underlying predisposing factors, the young man was not on any medication, there was no history of trauma, and no known allergies. The patient was an occasional mouth breather, but there was no indication of sinus involvement.
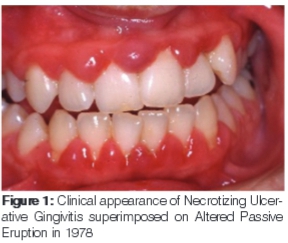
Clinically there was marked gingival hyperplasia, papillary ulceration, sub-gingival calculus and "altered passive eruption" (APE, then termed Delayed Passive Eruption). The gingivae bled on instrumentation and were tender to palpation. Probing and determining pocket depths were difficult, causing considerable pain. The appearance, however, was that of pseudo-pockets. This picture matched the clinical description presented in a 1974 publication "Delayed Passive Eruption - a predisposing factor to Vincent's infection?"1 The authors concluded "that patients between the ages of 15 and 35 years of age having Delayed Passive Eruption be instructed in meticulous oral hygiene as the risk of developing Vincent's infection (Necrotizing Ulcerative Gingivitis, NUG) is high."1 A tentative diagnosis of NUG was made (Figure 1).
Treatment: The patient was placed on a course of Metronidazole, one 200mg tablet t.d.s. with meals, for three days. He was instructed to return one week later to commence periodontal treatment, but returned only one month later.
Treatment then continued with a thorough scaling and instruction in home care. Whilst there had been an improvement in the severity of the gingival infection, the patient was instructed, as a precaution, to use chlorhexidine gluconate mouth wash. Scaling was continued the following week. The patient then attended for treatment at three to four monthly intervals, at which appointments scaling was repeated and the importance of home care, particularly flossing, was emphasized.
In June 1980, two years after the initial consultation, there was still concern that the teeth appeared to have not yet fully erupted (Figure 2). The patient was now seventeen, and discussion ensued on the need to reduce the gingival over-growth.

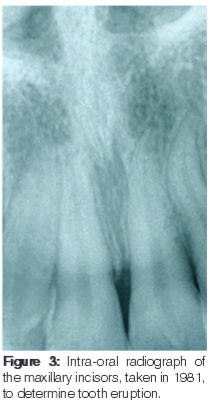
The following year (1981) a radiograph was taken (Figure 3) that showed the extent of the incisor eruption and the distance between the cemento-enamel junction and the alveolar margin. These established that APE was indeed an issue so a gingivectomy was performed around the maxillary incisors and canines. Regular maintenance visits then ensued at intervals between three to six months. After a period of eighteen months (in 1983), the patient complained of an infection and discomfort that was managed by the administration of an antibiotic (caps Tetremel 250mgms) and chlorhexidine gluconate mouth washes. Another year passed, and the periodontal condition was described as fair in 1984.
For all the ensuing years, visits to the practice have been regular every three to six months. In 1993 (Figure 4) the patient presented with tender gums. The cause was diagnosed as mouth breathing and plaque accumulation. He was also inclined to be vigorous rather than thorough with his tooth brushing. This accounted for some of the attachment loss as seen in Figure 5, particularly on the buccal aspect of the canines.


To the best of the knowledge of the attending clinician (AV), the patient has not required any other dental attention. Over the years, however, there has been further imbrication of the incisors and attachment loss.
At the most recent visit in November 2014 (Figure 6), only a mild gingival inflammation was observed. Whilst some further attachment loss had occurred, there was no gingival bleeding, and there were no probing depths greater than 3mm.

DISCUSSION
NUG is a debilitating and painful disease that left untreated may progress to severe damage to the periodontal supporting tissues and the loss of teeth. It is regarded as rare today but was a troublesome condition during the Second World War when soldiers contracted "trench mouth". Discussion at that time centered on predisposing factors. Stammers2 described local factors as gross neglect, food stagnation, calculus, over-crowding, mouth breathing, smoking and recent extractions.
Among the systemic predisposing factors, Stammers included frequent colds, possible vitamin deficiency, recent illness, pregnancy, over work and lack of exercise.2 Stress was identified as an indicator when studies were undertaken of army recruits and of students at times of examination.2 More recently, Manson and Eley have added over-hanging margins of restorations and partly erupted teeth to the local factors.3 It was thought that in developed countries NUG was primarily limited to adolescents.4 and that in less developed nations it affected younger people.5 There was consensus on the age of susceptibility of 15 to 30 years.
In 1978, the patient in this report presented with the classical symptoms of bleeding, painful gums, necrotic papillae, and fetor oris. Whilst it is not known whether he had any of the systemic predisposing conditions, the presence of APE could have been a local factor leading to the onset of NUG.1
Manson6 in 1975 recommended a treatment commencing on the first day with a thorough irrigation of the gingivae with warm water, plus sponging with cotton wool soaked in 10% hydrogen peroxide. He also recommended the use of a dilute hydrogen peroxide mouth wash, and, if the symptoms were severe, the prescription of Metronidazole 200mg tds for three days. On the fifth day of the programme, fine scaling was to be carried out and oral hygiene instruction delivered. Addy and Llewelyn reported that chlorhexidine gluconate and providone iodine mouthwashes were ineffective in the treatment of the acute phase of NUG if debridement was not performed.7 Their suggestion was that Metronidazole should be used under these circumstances.
In the treatment regime followed in the current case, the main emphasis has been on a maintenance programme, described today as Supportive Periodontology Therapy (SPT), the goals of which are to minimize the progression of the periodontal disease in patients previously treated for periodontitis / gingivitis.8 Merin has also described the programme and in 2006 wrote "The frequency of recall visits depends upon each patient. Some patients require frequent recall intervals to limit the inflammation around the teeth, while others may tolerate fewer recall visits. Most patients with periodontitis will need a long-term recall schedule, with visits for professional cleaning every 3-4 months, and close supervision of their oral hygiene procedures."9
SPT has been the treatment routine followed over thirty four years by the patient described. He has maintained reasonable oral health, has not lost any teeth and presents a healthy mouth and body ... he is a triathlon participant and a competitive oarsman!
CONCLUSIONS
A fifteen year old male presented thirty six years ago with NUG superimposed on APE. The condition was treated initially with scaling and Metronidazole 200mg t.d.s. Three years later a gingivectomy was carried out around the maxillary incisors and canines to reduce the gingival over-growth. This was followed with a maintenance programme equivalent to SPT, with an emphasis on meticulous home care. This regime has achieved the long term goal of preventing a recurrence of the condition and has successfully maintained a healthy periodontium for over three decades.
Consent
The patient gave his consent and agreed that the photographs of his teeth and gingivae may be used anonymously for academic publication.
Ethics clearance certificate No: M150156
ACRONYMS
APE: Altered Passive Eruption
DPE: Delayed Passive Eruption
NUG: Necrotizing Ulcerative Gingivitis
SPT: Supportive Periodontal Treatment
REFERENCES
1. Volchansky A, Cleaton-Jones PE. Delayed passive eruption- a predisposing factor to Vincent's infection? J Dent Assoc of South Africa. 1974;29:291-4. [ Links ]
2. Stammers AF. Vincent's infection. Observations and conclusions regarding aetiology and treatment of 1017 civilian cases. British Dental J. 1944;76:147-55; 171-7; 205-9. [ Links ]
3. Manson JD, Eley BM. Outline of Periodontics. 3rd Ed. Reed Educational and Professional Publishing, Oxford, 1995. [ Links ]
4. Giddon DB, Zackin SJ, Goldhaber P. Acute necrotizing ulcerative gingivitis in college students. JADA 1964; 68: 381. [ Links ]
5. Sheiham A. An epidemiological survey of acute ulcerative gingivitis in Nigerians. Archs Oral Biol. 1966; 11: 937-42. [ Links ]
6. Manson JD. Periodontics.: Oxford: Henry Kimpton Publishers, 1975:229. [ Links ]
7. Addy M, Llewelyn J. Use of chlorhexidine gluconate and providone iodine mouthwashes in the treatment of acute ulcerative gingivitis. J Clin. Periodontol. 1978 ; 5: 272-5. [ Links ]
8. Renvert S, Rutger Persson G. Supportive periodontal therapy. Periodontology 2000. 2004; 36: 179-95. [ Links ]
9. Merin RL. Supportive periodontal treatment. In: Neuman WG, Takai HH, Klukkevold PR and Carranza FA, editors: Carranza's Clinical Periodontology. 2006. St Louis: Saunders. Elsevier. 2006:1194. [ Links ]
 Correspondence:
Correspondence:
A Volchansky
Department of Oral Medicine and Periodontology
School of Oral Health Sciences
University of the Witwatersrand
Johannesburg
Tel: 011 442 6243
E-mail: volchans@iafrica.com













