Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.70 no.5 Johannesburg Jun. 2015
CASE REPORT
Keratocystic odontogenic tumour masquerading as a mucosal antral cyst
R CarimI; F MahomedII; S NgwenyaIII; E RikhotsoIV
IBChD. Department of Orthodontics, School of Oral Health Sciences, Faculty of Health Sciences, University of Pretoria, Pretoria, South Africa
IIMDent. Department of Oral Pathology, School of Oral Health Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIMDent. Department of Oral Pathology, School of Oral Health Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVMDent, FCMFOS(SA). Department of Maxillofacial and Oral Surgery, School of Oral Health Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
Keratocystic odontogenic tumour (KCOT) is of clinical importance because of its pronounced tendency to recur. Among the factors that complicate KCOT management are its protean radiological presentations. KCOT showing involvement of the maxillary antrum in the absence of an associated impacted tooth is exceptionally rare. In these instances an odontogenic source of the lesion is often not suspected and the clinico-radiological features may be misinterpreted. We report such a case and highlight pertinent clinical and radiological features of antral KCOT.
INTRODUCTION
Keratocystic odontogenic tumour (KCOT), traditionally known as odontogenic keratocyst, received its new title as KCOT by the World Health Organisation (WHO) in order to emphasise its neoplastic biological nature.1 The most common location is the mandible wherein 75%-85% of KCOTs develop.2 Of the maxillary lesions < 1% show involvement of the maxillary antrum.3 KCOT is of clinical importance because of its tendency to recur. Furthermore, its protean radiological presentations may lead to confusion with other jaw lesions, leading to underdiagnosis and undertreatment, thereby resulting in avoidable recurrences. Most KCOTs that involve the maxillary antrum are associated with an impacted tooth and mimic a dentigerous cyst.4 KCOT showing involvement of the maxillary antrum in the absence of an associated impacted tooth is distinctly uncommon. In such cases an odontogenic source of the lesion may not be suspected on clinical and radiologic grounds. We report such a case and highlight pertinent clinical and radiologic features to reduce the dearth of knowledge regarding KCOT with sinus involvement.
CASE REPORT
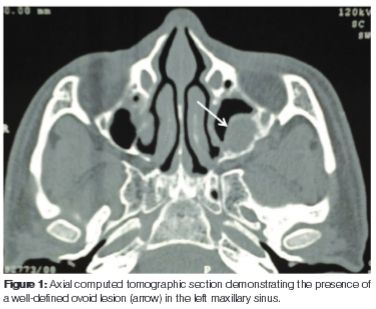
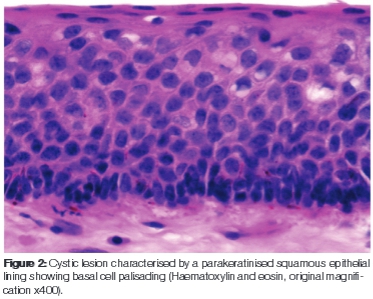
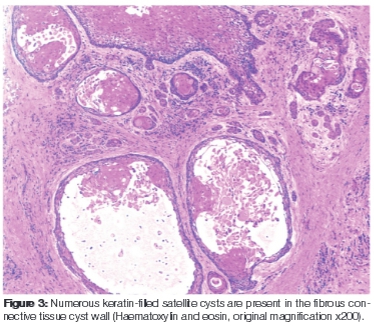
A 55-year-old male patient presented with a painless, expansile lesion in the left maxillary sinus area of approximately four months duration. Plain films showed opacification in the left maxillary sinus region. Computed tomography revealed a well-defined, rounded, homogenous lesion, benign in appearance, in the left maxillary sinus region. The lesion had caused thinning of the medial wall of the nasal cavity. Based on the clinico-radio-logical presentation, a provisional diagnosis of a cyst of the maxillary antrum was made (Figure 1). An incisional biopsy was performed and the tissue was submitted for histopathology. A diagnosis of KCOT was made (Figures 2 and 3). The lesion was subsequently enucleated via a Caldwell-Luc procedure and supplemental cryotherapy was performed (Figure 4). The patient showed no signs of nevoid basal cell carcinoma syndrome. There were no signs of recurrence at a six year follow-up.

DISCUSSION
The appearance of KCOT in the maxillary antrum is an unusual presentation for this lesion. Studies of KCOT have found sinus involvement in 2(0.6%) of 312 cases, in 1(0.9%) of 106 cases and in 2(0.6%) of 326 cases.5 The incidence of KCOTs in the maxillary sinus is, therefore, probably less than 1% of all keratocysts. Even rarer is the occurrence of KCOT within the maxillary antrum in the absence of an associated impacted tooth. In such situations the clinico-radiological features may be misinterpreted as a sinus mucocele, surgical ciliated cyst, sino-nasal polyps
or tumours. Mucoceles of the paranasal sinuses are generally considered to arise from obstruction of the ostium as a result of inflammation, trauma or a neoplasm. Sinus mucoceles are most frequently found in the frontal sinus, followed by the ethmoid, sphenoid and maxillary sinus. The resected mucosa is either normal or compressed respiratory mucosa. The lesions are often expansile and can erode bone.3 The surgical ciliated cyst of the antrum, also referred to as the post-operative maxillary cyst, develops following trauma or surgery to the sinus. Radiographically, they present as well-defined unilocular or multilocular radiolucencies. Histologically, the cyst is lined by respiratory-type epithelium. The lesion may be treated by simple enucleation. Sino-nasal polyps, believed to be a complication of chronic infection, are demonstrated as smooth, soft tissue masses with downward convexity. If polyps enlarge to fill the entire sinus, they may obstruct sinus drainage and become symptomatic. Substantial bone erosion can occur with benign sino-nasal lesions such as with inverted papillomas, haemangiomas or sino-nasal polyps, which can lead to the misdiagnosis of a malignant tumour. In these cases the duration of the lesion, history of epistaxis and/or chronic rhino-sinusistis can aid in differential diagnosis.6
KCOT of the maxillary sinus should further not be confused with maxillary sinus cholesteatoma. Terminology used in the literature that refers to antral cholesteatoma includes keratoma, epidermoid cyst and keratocyst.7,8 Whilst both antral KCOT and cholesteatoma may show overlapping clinical and radiological features their histogenesis, treatment and prognosis differ significantly. Antral cholesteatoma is thought to arise from traumatic implantation of epithelium into the sinus, from migration of keratinising squamous epithelium into the area or from misplaced epithelial rests during the embryonic stage.8 KCOT arises from derivatives of the dental lamina, an embryonic structure that normally differentiates into tooth buds during odontogenesis.2 KCOTs that develop outside the tooth bearing areas of the jaw are thought to arise from ectopic dental lamina. The palisaded arrangement of hyperchromatic basal cells and parakeratinised epithelial lining of KCOT are histological features that allow accurate distinction between KCOT, antral cholesteatoma and orthokeratinising jaw cysts.1 The notorious potential for recurrence associated with KCOT is an important clinical characteristic that separates it from lesions such as the antral cholesteatoma and orthokeratinising jaw cysts which seldom recur.2
Recurrence rates of the KCOT vary between 25.0% and 62.5%.910 Most reports found recurrences within five to seven years after enucleation.9,10 Several factors have been cited as possible reasons for this relatively high rate of local recurrence for the KCOT. These include the histomorphological configuration of the KCOT which hinders complete removal following simple enucleation, the KCOTs tendency for multiplicity and association with the nevoid basal cell carcinoma syndrome. Recurrence rates may also be dependent on the type of surgical therapy employed. KCOT management necessitates enucleation or curettage followed by peripheral ostectomy or treatment of the cavity with an agent, such as liquid nitrogen or Carnoy's solution, to destroy the residual epithelial remnants or satellite cysts.11 It has been found that the combination of surgical enucleation and cryotherapy provides improved outcomes for patients.12
CONCLUSION
The detection of KCOT with maxillary sinus involvement in the absence of an associated impacted tooth may result in misdiagnosis. While computed tomographic study can accurately delineate the site, size of the lesion, composition of the lesion and extent of osseous involvement; it remains challenging to definitively diagnose KCOT on clinico-radiologic grounds alone because of its relative lack of specific clinical and radiographic characteristics. Hence correlation of the clinico-radiologic findings with a biopsy specimen examination appears to be the best way to accurately diagnose KCOT. This approach will help to determine the appropriate treatment, thereby preventing recurrences.
Declaration: No conflict of interest declared.
ACRONYMS
KCOT: Keratocystic odontogenic tumour
WHO: World Health Organisation
References
1. Philipsen HP. Keratocystic odontogenic tumour. In: Barnes L, Eveson JW, Reichart P, Sidransky D, eds. World Health Organization Classification of Tumours. Pathology and Genetics. Head and Neck Tumours. IARC Press Lyon, 2005: 306-7. [ Links ]
2. Shear M, Speight PM. In: Shear M, Speight PM, eds. Cysts of the Oral and Maxillofacial Regions, 4th ed.Oxford:Blackwell Munksgaard, 2007: 45-58. [ Links ]
3. Bastaki JM, Schafer DR. Clinical pathologic conference case 4: an incidental maxillary sinus finding. Oral Surg Oral Med Oral Pathol Oral Radiol 2013;115:e44-6. [ Links ]
4. Chaudhary S, Sinha A, Barua P, Mallikarjuna R. Keratocystic odontogenic tumour (KCOT) misdiagnosed as a dentigerous cyst. BMJ Case Rep 2013;bcr2012008741. [ Links ]
5. Cioffi GA, Terezhalmy GT, Del Balso AM. Odontogenic keratocyst of the maxillary sinus. Oral Surg, Oral Med, Oral Pathol 1987;64:648-51. [ Links ]
6. Mills SE, Fechner RE, The nose, paranasal sinuses and nasopharynx In: Sternberg SS, Carter D, Mills SE, eds. Sternberg's Diagnostic Surgical Pathology, 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 1999: 885-98. [ Links ]
7. Viswanatha B. Cholesteatoma of the nose and maxillary and ethmoid sinuses: a rare complication of palatal surgery. Ear Nose Throat J 2011; 90:428-30. [ Links ]
8. Hartman JM, Stankiewicz JA. Cholesteatoma of the paranasal sinuses: Case report & review of the literature. Ear Nose Throat J 1991;70:719-25. [ Links ]
9. Madras J, Lapointe H. Keratocystic odontogenic tumour: Reclassification of the odontogenic keratocyst from cyst to tumour. J Can Dent Assoc 2008;74:165-165h. [ Links ]
10. Nakamura N, Mitsuyasu T, Mitsuyasu Y, Taketomi T, Higuchi Y, Ohishi M. Marsupialization for odontogenic keratocysts: Long-term follow-up analysis of the effects and changes in growth characteristics; Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94: 543-53. [ Links ]
11. Schmidt BL, Pogrel MA. The use of enucleation and liquid nitrogen cryotherapy in the management of odontogenic keratocysts. J Oral Maxillofac Surg 2001;59:720-5. [ Links ]
12. Kuroyanagi N, Sakuma H, Miyabe S, et al. Prognostic factors for keratocystic odontogenic tumor (odontogenic keratocyst): analysis of clinic-pathologic and immunohistochemical findings in cysts treated by enucleation. J Oral Pathol Med. 2009;38:386-92. [ Links ]
 Correspondence:
Correspondence:
R Carim
Department of Orthodontics
School of Dentistry
University of Pretoria
P.O. Box 1266
Pretoria, 0001
South Africa
Tel: +27 12 319 2555
E-mail: ridwaana.carim@gmail.com













