Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.70 n.2 Johannesburg Mar. 2015
CLINICAL CASE REPORT
Congenital granular cell tumour: An unusual antenatal presentation with a 12- year follow-up
N PrabhuI; J McDonaldII; D CassIII; H ColemanIV; AC CameronV
IBDS MDS MPhil MRACDS FRACDS. Staff Specialist and Clinical Senior Lecturer, Paediatric Dentistry, Westmead Hospital Westmead, NSW, Australia
IIMB BS (Hons) FANZCA. Visiting Medical Officer, Anaesthesia. Westmead Hospital and the Children's Hospital, Westmead, NSW, Australia
IIIMB BS PhD FRACS. Professor of Paediatric Surgery, The Children's Hospital at Westmead, Westmead, NSW, Australia
IVBDS, BChD (Hons), MDent (Oral Path), FCPath (Oral Path), NZDRE, FFOP (RCPA), FICD Institute of Clinical Pathology and Medical Research and The University of Sydney, Westmead Hospital, Westmead, NSW, Australia
VBDS(Hons) MDSc FDSRCS(Eng) FRACDS. Clinical Associate Professor and Head, Department of Paediatric Dentistry & Orthodontics, Westmead Hospital, Westmead, NSW, Australia
ABSTRACT
Congenital epulis, also known as congenital granular-cell tumour (CGCT) is a rare benign entity that occurs in neonates. The size and prominent location of the lesion(s) in the oral cavity ensures early recognition. This paper aims to provide a comprehensive background of this rare lesion and discusses the presentation in a neonate diagnosed at 35 weeks on a routine ultrasound. Oral health practitioners should be aware that these lesions may cause dental developmental anomalies at the site where they occur.
Key words: Congenital epulis in newborn, Granular cell tumour, EXIT procedure
INTRODUCTION
The congenital granular-cell tumour (CGCT) is a rare benign lesion of unknown origin found only in neonates. It has also been documented as a congenital epulis, granular cell tumour of infancy or epulis of the newborn. Since the first reported case by Neumann in 1871, about 200 cases have been cited in the dental literature.1 Its origin is uncertain but is thought to arise from the undifferentiated mesenchymal/stromal cells and is therefore thought to be non-odontogenic in origin.
The CGCT occurs ten times more frequently in females than in males.2 It appears sporadically with no known familial patterns of inheritance.3,4 Generally, the medical histories of the mothers reveal uncomplicated pregnancies, full term gestations and normal parturitions. Most affected children have been reported in Caucasian women.5 Although it usually presents as an isolated finding at birth, cases with strong associations with polyhydramnios, neurofibromatosis, XXX chromosome and polydactyly have also been reported.6,7 Occasionally, the lesions may be detected prenatally on a routine ultrasound examination but the findings are usually non-specific. Antenatal detection of this lesion has been reported in five cases during the 2nd and 3rd trimester by means of ultrasound examination8 with the earliest reported antepartum identification being made at the 29.5 week of gestation.9
The typical clinical appearance is that of a solitary, firm, pedunculated, flesh-pink coloured nodule located in the incisor or canine region of the alveolar ridge.10 The maxilla is three times more commonly affected than the mandible and multiple lesions (10%) have been reported by some authors.10,11 They vary in size ranging from several millimeters up to 9.0 centimeters in diameter, with larger tumours often showing superficial ulceration due to frictional trauma associated with bottle-feeding.4 Pathologic and radiographic investigations have confirmed that these are soft tissue tumours with no involvement of the underlying bone.12 Aesthetically, the CGCT may be alarming to parents because of a large size and aggressive appearance. Complications include dyspnoea, respiratory obstruction, cyanosis and an inability to close the mouth leading to difficulty in sucking and swallowing.1,9
The pathogenesis of CGCT is controversial and remains unknown. Odontogenic and epithelial origins, previously suggested, have now been discounted and more recent ultrastructural findings implicate gingival stromal cells in the histogenesis of this lesion.3 Clinical observations of a lack of postnatal growth, instances of spontaneous regression and non-recurrence after incomplete resection are consistent with this hypothesis.1,13
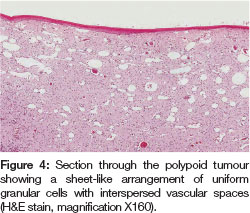
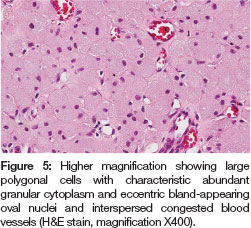
A provisional diagnosis of CGCT is often made at birth with a definitive diagnosis usually confirmed following histologi-cal examination and immune-histochemical staining. Histo-logically, the lesion consists of large eosinophilic granular cells within a vascular fibrous stroma. The lesional cells are positive for lysozyme, HLA-DR, macrophage marker CD68 and negative for S-100 protein as well as epithelial markers.1 S-100 protein antigen negativity, which is specific for Schwann cells, excludes a neurogenic etiology and aids in distinguishing between the CGCT and the granular cell tumour that appears after birth.3,14
CASE REPORT
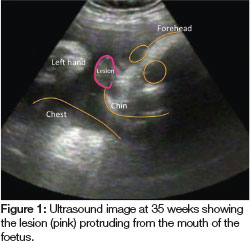
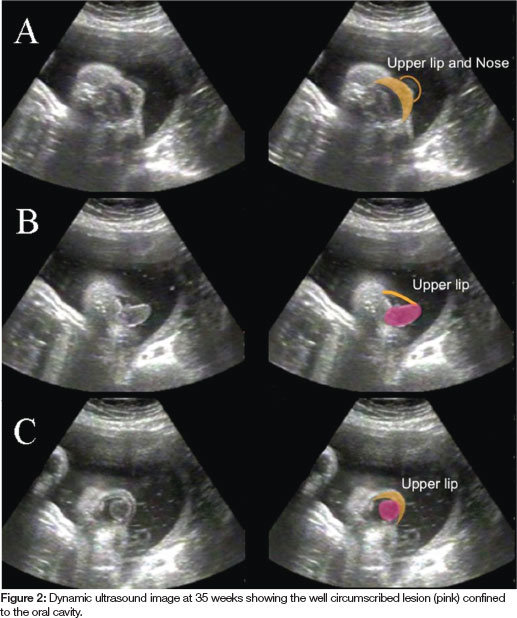
A 32 year old woman of Middle Eastern origin, gravida 4, was booked for an elective Caesarean section. After a normal screening ultrasound at 19 weeks gestation, examination of a second ultrasound at 35 weeks found a tumour extending from the mouth of the foetus (Figure 1). A large component of the lesion was confined to the mouth, but was also observed to extend 1-2cm beyond the lips on dynamic ultrasound. The well-circumscribed lesion appeared to arise from the maxillary alveolar process and its posterior extent was confined to the oral cavity (Figures 2A-C). The head was turned to the right during most of the time of the scan and on other occasions it was hyper extended in the sagittal plane. There appeared to be a swelling of the left cheek, which could have been continuous with the oral tumour. The neck and trachea appeared to be within normal anatomical limits.
A multidisciplinary meeting that included an obstetrician, paediatric surgeon, neonatologist and an anaesthetist was convened and the decision was made to deliver the baby electively by caesarean section using an EXIT (Ex Utero Intrapartum Treatment) Procedure.15 This unique technique is used to maintain foetal-placental circulation during partial delivery of the foetus with a potentially life threatening upper airway obstruction. Unfortunately, the patient went into labour the night before this planned operation and so the EXIT procedure was carried out as an emergency. Following general anaesthesia, the baby was intubated by a paediatric anaesthetist when the head came in view but before placental separation was made. A paediatric surgeon was on stand-by in the event that a surgical airway was required. Intubation was not difficult once the laryngoscope was placed past the tumour. After the baby was delivered, the endotracheal tube was kept in-situ until the tumour was surgically removed later on that day.
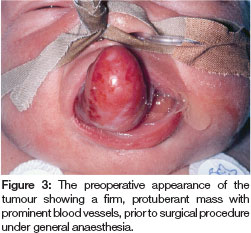
The infant was transferred to the Neonatal Intensive Care Unit at the Children's Hospital at Westmead for observation and a consultation was requested from the specialists in Paediatric Dentistry and Paediatric Surgery. The lesion measured 4x2x2 cms and arose from the alveolus on the right side of the maxillary alveolar gum pad (Figure 3). It was firm on palpation and the surrounding mucosa appeared normal. Large arterial feeder vessels were noted and were consistent with a vascular supply to a lesion of this size. The child was taken to the operating room the following evening to undergo an excisional biopsy of the lesion. The stalk of the lesion was tied off and the tumour completely excised. Haemorrhage was controlled with diathermy. There were no postoperative complications and the child was then transferred back to her mother in the postnatal ward where she was able to successfully breast feed. Healing was uneventful and the upper primary teeth erupted through the site of the surgery at approximately eight months of age.
Multiple sections of the lesion stained with hematoxylin and eosin were examined. They showed large polygonal cells containing granular eosinophilic cytoplasm and eccentrically placed nuclei located within a delicate fibrovas-cular connective tissue stroma (Figures 4,5). A diagnosis of CGCT was made.
The patient continued to maintain her recall appointments with the hospital for many years and there has been no recurrence of the lesion, the most recent being her 12 year follow-up appointment (Figure 6).

DISCUSSION
Although the clinical presentation of a CGCT can be visually striking due to its size and reddish appearance, it is benign and does not recur following complete surgical excision. The lesions vary in size they and are not known to cause any damage to the developing dentition. Diagnosis is always confirmed by histological examination. The aetiology is unknown and most authors suggest a mescenchymal rather than an odontogenic origin.3,16 With advancement in imaging technology, oropharyngeal lesions may be diagnosed prenatally by the utilisation of ultrasonography or magnetic resonance imaging.1718 However, they are rarely detected before the third trimester.16 Postnatal imaging such as conventional radiography and computed tomography allow an evaluation of the degree of calcification of the mass, the presence of any bony defect and the intracranial extent of the lesion.19,20
The management of CGCT's depends on the extent of the tumour and the site of origin with no standard protocols having been documented in the current literature. They have a potential to complicate general anaesthesia by interfering with endotracheal intubation. The treatment options are either simple, conservative excision especially when major feeding or obstructive respiratory problems arise or a wait-and-watch approach due to the possibility of spontaneous involution or regression in smaller lesions.11,21 If the latter fails, then a non-radical excision at the tumour base is preferred at the age of 4-6 weeks. Wide radical excision is not required nor recommended due to the possibility of damage to the future development of the dentition and disfigurement of the soft tissues.4 Some clinicians have excised the lesion using carbon dioxide lasers.13 Regular follow-up is recommended to ensure early detection of very rare malignant transformation of the residual elements as well as to monitor the normal development of the facial bones and dentition.14 The antepartum identification of the lesion in this case made it possible to organise a multidisciplinary team to ensure maintenance of an adequate airway and early surgical intervention thereby resulting in a favourable outcome for the patient.
Declaration: No conflict of interest was declared.
References
1. Leocata P, Bifaretti G, Saltarelli S, Corbacelli A, Ventura L. Congenital (granular cell) epulis of the newborn: A case report with immunohistochemical study on the histogenesis. Ann Saudi Med 1999; 119(6): 527-9. [ Links ]
2. Fuhr AH, Krogh PH. Congenital epulis of the newborn: centennial review of the literature and a report of case. J Oral Surg 1972; 30(1): 30-5. [ Links ]
3. Lack EE, Perez-Atayde AR, McGill TJ, Vawter GF. Gingival granular cell tumour of the newborn (congenital "epulis"): ul-trastructural observations relating to histogenesis. Hum Pathol 1982; 13(7): 686-9. [ Links ]
4. Lapid O, Shaco-Levy R, Krieger Y, Kachko L, Sagi A. Congenital epulis. Pediatrics 2001; 107(2): E22. [ Links ]
5. Anderson PJ, Kirkland P, Schafler K, Moss AL. Congenital gingival granular cell tumour. J R Soc Med 1996; 89(1): 53P-4P. [ Links ]
6. Chindia ML, Awange DO. Congenital epulis of the newborn: a report of two cases. Br Dent J 1994; 176(11): 426-8. [ Links ]
7. Kim ES, Gross TL. Prenatal ultrasound detection of a congenital epulis in a triple X female fetus: a case report. Prenat Diagn 19(8): 774-6, 1991. [ Links ]
8. Pellicano M, Zullo F, Catizone C, et al. Prenatal diagnosis of congenital granular cell epulis. Ultrasound Obstet Gynecol 1998; 11(2): 144-6. [ Links ]
9. Kumar P, Kim HH, Zahtz GD, Valderrama E, Steele AM. Obstructive congenital epulis: prenatal diagnosis and perinatal management. Laryngoscope 2002; 112(11): 1935-9. [ Links ]
10. Bowe JJ. Congenital epulis tumour. Case report. Plast Reconstr Surg 1974; 53(2): 227-9. [ Links ]
11. O'Brian FV, Pielou WD. Congenital epulis: its natural history. Arch Dis Child 1971; 46(248): 559-60. [ Links ]
12. Kershisnik M, Batsakis JG, Mackay B. Granular cell tumours. Ann Otol Rhinol Laryngol 1994; 103(5 Pt 1): 416-9. [ Links ]
13. Dash JK, Sahoo PK, Das SN. Congenital granular cell lesion "congenital epulis"--report of a case. J Indian Soc Pedod Prev Dent 2004; 22(2): 63-7. [ Links ]
14. Parmigiani S, Giordano G, Fellegara G, Brevi B, Magnani C. A rare case of multiple congenital epulis. J Matern Fetal Neonatal Med 2004; 16 Suppl 2: 55-8. [ Links ]
15. Zerella JT, Finberg FJ. Obstruction of the neonatal airway from teratomas. Surg Gynecol Obstet 1990; 170(2): 126-31. [ Links ]
16. Kupers AM, Andriessen P, van Kempen MJ, et al. Congenital epulis of the jaw: a series of five cases and review of literature. Pediatr Surg Int 2009; 25(2): 207-10. [ Links ]
17. Bilen BT, Alaybeyoglu N, Arslan A, et al. Obstructive congenital gingival granular cell tumour. Int J Pediatr Otorhinolaryngol 2004; 68(12): 1567-71. [ Links ]
18. Roy S, Sinsky A, Williams B, Desilets V, Patenaude YG. Congenital epulis: prenatal imaging with MRI and ultrasound. Pediatr Radiol 2003; 33(11): 800-3. [ Links ]
19. Fister P, Volavsek M, Novosel Sever M, Jazbec J. A newborn baby with a tumour protruding from the mouth. Diagnosis: congenital gingival granular cell tumour. Acta Dermatovenerol Alp Panonica Adriat 2007; 16(3): 128-30. [ Links ]
20. Valente A, Grant C, Orr JD, Brereton RJ. Neonatal tonsillar teratoma. J Pediatr Surg 1988; 23(4): 364-6. [ Links ]
21. Witman PM, Rogers RS, 3rd. Pediatric oral medicine. Dermatol Clin 2003; 21(1): 157-70. [ Links ]
 Correspondence:
Correspondence:
N prabhu
Paediatric Dentistry,Westmead Hospital
Westmead, NSW, Australia.
Tel: +61 2 9845 7446. Fax: +61 2 9845 8306
E-mail: Neeta.Prabhu@health.nsw.gov.au













