Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.70 no.1 Johannesburg Fev. 2015
RESEARCH
Evaluation of two different-gauge dental needles for the presence of blood following the application of local anesthesia by dental students
MJ KotzeI; W LabuschagneII
IMSc Odont (in Oral Surgery). Senior Lecturer, Department of Maxillo-Facial and Oral Surgery, School of Dentistry, Faculty of Health Sciences, University of Pretoria, South Africa
IIAdv University Dipl(Health Studies), Operational Manager (Infection Control, Occupational Health and Quality Assurance) School of Dentistry, Faculty of Health Sciences, University of Pretoria. South Africa
SUMMARY
Blood-borne virus transmissions from patient to dental health care personnel are occupational hazards following needle stick injury.
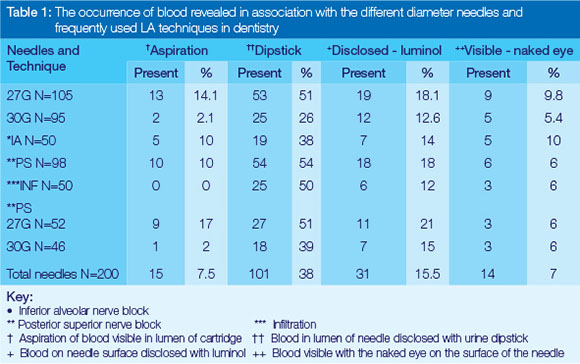
AIMS AND OBJECTIVES: Three local anesthetic (LA) techniques frequently used in the extraction of teeth were evaluated and compared for the presence of blood in the cartridge, needle lumen and needle surface when either 27G or 30G needles were used.
DESIGN AND METHODS: The histogram function of Photoshop computer software identified differences in grey-scale value of the different blood parameters on photographs of urine dipsticks moistened with the first drop of liquid from the needle after the injection had been given and luminol spray was used to expose small quantities of blood on the surface of the needle. Blood visible to the naked eye in the LA cartridge was noted.
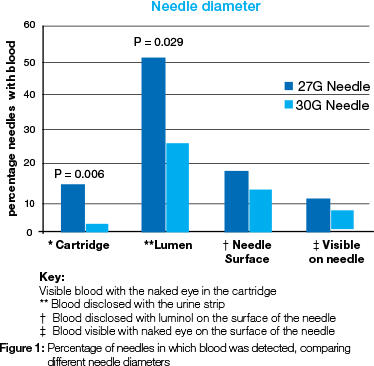
RESULTS: A statistically significant association was found between needle diameter and visible blood in the cartridge (P=0.006), and the presence of blood in the needle lumen (P=0.029), especially with the 27G needle.
CONCLUSION: There was a statistically significant difference in the presence of blood in the lumen (36%) and in the cartridge (29%) between 27G and 30G needles following the administration of LA to a patient.
INTRODUCTION
Several published reports have examined occupational injuries and their prevalence in dental healthcare settings across different provider populations,1-3 while other studies have assessed needle stick injuries (NSI) amongst dental students4-7 who are regarded as high risk for NSI.4,8,9 That susceptibility is generally assumed to be the result of a lack of experience in the handling of needles after administration of local anesthesia (LA). NSI as occupational hazards carry a general risk of transmission of 30% for Hepatitis B virus (HBV), of 3% for hepatitis C virus (HCV), and of 0.3% for human immunodeficiency virus (HIV).2,3,10,11 Dental professionals are at low occupational risk for HIV infection.12,13 The danger of viral infection in the operating room remains the same as a decade ago, even though attention to this issue has decreased.14 Percutaneous exposures result from injuries by any sharp object used in dentistry and surgery - such as contaminated needles, burs, scalpels, exposed ends of dental wires or other sharps (eg. broken glass), that penetrate or break skin. These injuries can occur at any time during dental treatment, especially when personnel use, disassemble or dispose of needles.4 The transmission risk is influenced by the type and number of microorganisms present in the blood, presence of visible blood on the needle, depth of the injury and size and type of needle used.15 One third of all reported sharps injuries in dental practice are due to the use of non-disposable dental syringes, with most injuries being sustained during removal and disposal of the disposable needle from the non-disposable syringe.
Attempts were made to encourage the more general use of disposable syringes in dentistry,16 but the non-disposable syringe is still popular and widely used. A study estimates that 53 percent of needle stick injuries could be prevented by use of a dental safety syringe.17 Studies have tended to focus on in vitro NSI models and the influence of different types of gloves.18-20 In a previously documented ex vivo study, thicker gauge needles were reported to typically be used for intra-venous injections, intra muscular injections and veni-puncture.21 The transfer of blood is also documented from ex vivo studies in which needles were dipped into labelled blood.18,22 A recent study confirmed that half the number of needles evaluated following the administration of LA contained less than 10% blood in the needle lumen.23 Another study demonstrated 1μΙ_ blood in the lumen of a 22G needle after it was dipped into blood and the contents evaluated.24 However, the literature focuses mostly on the prevalence of NSI, possibly associated with the difficulty in demonstrating the minute quantity of blood which may be present on the surface and in the lumen of a small-gauge needle.
The choice of the needle for administering LA is exclusively that of the operator, taking into consideration the common principle of a 27G needle for inferior alveolar nerve block (IA) and 30G needles for the remaining techniques. No differences have been shown between these needles with respect to efficacy, pain, aspiration, location (mandibular, maxillary posterior, maxillary anterior, and palatal), injection side, patient gender, treating dentist, or overall.25-27 Needle fracture during the application of LA is very rare, but still occurs,28 in the majority of cases during inferior alveolar nerve block, when it may be caused either by a faulty injection technique, pre-bending the needle, incorrect choice of hypodermic needle dimension, abrupt movement of the patient or inserting the needle up to the hub (which is its weakest spot).28,29
The aim of this study was to evaluate and compare the presence of blood on the surface and in the lumen of two different-gauge dental needles following administration of LA by dental students using three different techniques in administering the anaesthetic. Commercially available urine test strips, digital photography and a well-documented forensic method were used to detect the presence of blood in the lumen and on the external surface of the needle.23
METHODS
This study was approved in 2012 by the Research Ethics Committee, University of Pretoria Faculty of Health Sciences- approval 225/2012 - and was conducted from January 2013 to August 2013, following a method previously described in full.23
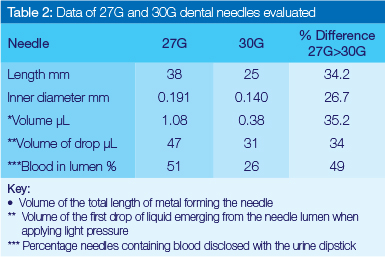
Patients were selected at random with no exclusions such as health conditions, purpose of treatment and outcome of treatment (surgical or uncomplicated extraction). The age of the patients varied between 5 and 75 years with the highest frequency in the groups 21-30 and 41-30 years. Aspirating syringes (Sterilife®, Anthogyr SAS, 2 237 avenue, André-Lasquin, 74700 Sallanches France) were used for the delivery of the LA solution. Needles (N=200) were collected after anaesthetics had been administered by students to 93 male (46.5 percent) and 107 (53.5 percent) female patients. The needles used were 27G (N=105) and 30G (N=95). The needle length was 38mm for the 27G needle and 25mm for the 30G needle. The average volume of a drop of LA, produced by gentle pressure on the plunger, was determined by weighing 35 drops of LA on an electronic scale and using the known density to calculate volume. The 27G needle delivered a drop of average volume 47μL ±3 and the 30G needle, a drop of 31μL ±4. Three frequently used LA techniques in dentistry in cases requiring extraction of teeth were used, namely, the inferior alveolar and long buccal nerve block (IA) (N=50), posterior superior and greater palatine nerve block (PS) (N=100) and buccal and palatal or labial (INF) infiltration (N=50) (Table 1). The number of 30G needles used per technique was IA 10, PS 47 and INF 37. For the 27G needle, 39 needles were used for IA, 53 for PS and 13 for INF (Table 2). The students were asked not to discard any of the solution from the needle after the administration of the LA, but simply to remove it from the tissue without pressure on the syringe plunger. This produced a negative pressure, thereby inducing a positive aspiration with fluid flowing into the needle. The effect was noted when visible blood was aspirated into the ampoule after the application of LA, ranging from a weak rosy colouring to a vigorous spurt of blood.30 The aspiration was considered positive when a reddish colouring appeared inside the anesthetic cartridge. The age and gender of the patient were noted, as well as possible blood visible on the surface of the needle.
EVALUATION OF NEEDLES
Immediately after the administration of the LA, pressure was applied delicately to the plunger and the first drop emerging from the needle contents was used to wet the blood parameter of a urine test strip. After one minute, standardized digital photographs were taken of the chemical pad which tested for blood on the urine test strip. For analysis, the photographs were imported into the computer programme Adobe Photoshop (V6.0; Adobe Systems Inc., San Jose, CA). This software was first used to establish a standard grey-scale value of images of the dry chemical pad for blood with the brightness and contrast tools. As the wetting of the chemical pad with the drop of LA caused colour change of the pad, the average grey-scale values could be determined. Density changes denoted the presence of blood and were divided into categories of 10%.
For the determination of the presence of blood on the surface of the needle, Blue Star® blood-finding agent was used (Bluestar, Monte-Carlo, Monaco). After the collection of the drop of liquid from the lumen of the needle, the needle was sprayed with this luminol-containing reagent. In the dark, the presence of blood shows a distinctive blue glow on the needle. The results were noted.
STATISTICAL ANALYSIS
Data were captured on an Excel spreadsheet and descriptive (frequencies, mean, and standard deviation) and comparative analyses were carried out with the use of SPSS Statistics version 21 using the Chi2-test.
RESULTS
Blood was identified in the aspiration fluid in 7.5% of the total 200 needles, in 38% by the dipstick method, in 15,5% by the Bluestar test and was visible to the eye in 7% of instances (Table 1). A statistically significant association was found between needle diameter and visible blood in the cartridge (P=0.006), and presence of blood in the needle lumen (P=0.029), especially with the 27G needle (Figure 1).
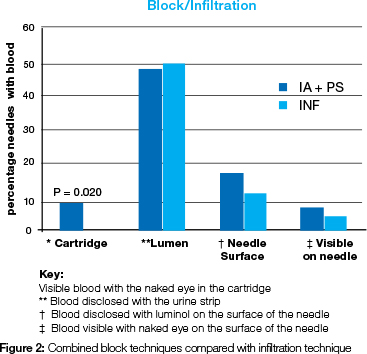
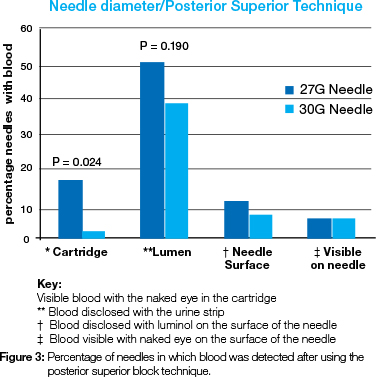
Visible aspirated blood in the cartridge was found to have a statistically significant association with the combined nerve block techniques and the infiltration technique (P=0.020) (Figure 2). The data of the different-diameter needles utilized in the PS revealed a statistically significant difference when the presence of blood in the cartridge and needle lumen was compared. More 27G needles presented aspirated blood in the cartridge, 14.8% (P=0.024) or blood in the needle lumen, 21.6 % (P=0.190), than the 30G needles (Figure 3).
No statistically significant difference was demonstrated between gender, age and LA technique used.
DISCUSSION
Visible blood was found in 7.5% of the cartridges following the administration of LA (Table 1), in accord with previous results which had shown less than 10 percent aspiration of blood.31-33 It is noteworthy that the technique used in the current study was not positive aspiration, but merely a normal backflow of fluid in response to the negative pressure in the cartridge when the plunger was released. The assessment for visible blood in the cartridge did not occur during the administering of LA, but after completion of the procedure. The origin of the visible blood in the LA cartridge was not identified and might have been from a ruptured blood vessel or from interstitial fluid. A statistically significant difference was found between needle diameters for blood visible with the naked eye in the LA cartridge (P=0.006) and for presence of blood in the needle lumen (P=0.029), the 27G needle being much more frequently implicated (Figure 1). More cartridges (64%) had blood using the wider bore needle. This finding contrasted with the results of other studies comparing aspiration and needle diameter.26,34,35 In those projects, careful evaluation of the aspirating techniques was carried out during and after the application of LA. In the current study, no special precautions or instructions were given to the students regarding aspiration so as to simulate a normal clinic or practice situation. The incidence of blood in the needle lumen and in the cartridge is therefore due to the normal flow of the liquid following the release of pressure on the plunger. Normally, the flow through a 30-gauge needle is significantly lower than flow through a 27-gauge or larger needle,36 as more resistance is experienced in the smaller-diameter needle. The volume of the 27G needle is 35.2% more than that of the 30G needle, while the diameter of the 27G needle is 26.7% larger than the diameter of the 30G needle (Table 2).
The average sensitivity of dipsticks for the detection of blood in urine is 91-100% and the specificity 65-99%.37 It can be anticipated that this sensitivity and specificity can be used for identification of blood in the liquid of the needle lumen after the administration of local anaesthesia.
No statistically significant difference was found between the three different techniques of administering LA for the occurrence of visible blood in the cartridge (Table 1). This finding differs from those of studies which found that aspiration was more frequent with the practice of the IAN technique.31-33 When the occurrence of visible blood in the cartridge was tested against the parameters of sex and age, no statistically significant differences were found. This finding supports that of a previous study.32 A statistically significant difference was demonstrated when the results of the IAN and PS were combined and compared with the result of the INF (Figure 2) but this may not be of any clinical significance, as it is well known that the blood supply is better in the area where the block technique is administered in comparison with that encountered when infiltrating. No statistically significant difference was found between the incidence of blood on the surface of a needle and needle diameter for the LA technique used, nor for the age and sex of patients (Table 1). Of the total number of needles evaluated for the presence of blood in the lumen, 38% were positive for containing blood, but only 15.5% of needles were positive when evaluated for blood on the surface as disclosed by luminol (Table 1). This latter was a surprising finding, for more blood had been expected as the needle had been embedded in blood-containing tissue. The oral epithelium, being a protective layer of the oral mucosa, probably provided a wiping effect during withdrawal of the needle from the tissue. Therefore, the absence of visible blood on the surface of a needle is not a true indicator for the presence or absence of blood following the application of LA to a patient.
In ex vivo studies, more blood was found to be present in the lumen of larger-bore hollow injection needles under evalu-ation.18,19 These results were confirmed in this in vivo study where needles were evaluated immediately following the administration of LA to a patient when there was a statistically significant (P<0.0187) greater incidence of blood visible in the LA cartridge, as well as blood present in the lumen of the 27G needle. The IA and INF were not compared because of the small sample size of different-diameter needles used for each technique - 27G mostly used for IA and 30G mostly used for INF. In a comparison involving the total number of needles evaluated, a difference was demonstrated in the presence of blood in the lumen between the 27G (51%) and the 30G (26%) needles.23 (Tables 1 and 2). The inner diameter of the 27G and 30G hollow-bore needles differs by 26.7% and the volume of the needles differs by 35.2% (Table 2). However, the presence of blood in the lumen of the 27G needle was nearly double that found in the 30G needle (Table 2). Therefore, the use of a 27G needle instead of a 30G needle almost doubles the risk of exposure to blood from a needle immediately following the administration of LA. Combining the results from the needles, the blood contents of the first drop of liquid extracted from the needle lumen was found to be low, with the majority of needles (61.5%) producing drops with less than 20% blood.23 The average volume of the first drop of liquid from the two different-diameter needles evaluated differs by 34% which implies a greater risk contracting a blood borne virus from an accidental NSI when the larger diameter 27G needle is involved.
CONCLUSION
It was possible to evaluate and compare the presence of blood in the first drop of liquid from 27G and 30G dental needles following the administering of LA using any of the three common techniques in dentistry. There was a statistically significant greater visibility of blood in the LA cartridge and more blood present in the lumen of the 27G needle following the injection. Both 27G and 30G needles are regularly used in dentistry, with no scientifically proven motivation as to preference. The selection of 30G needles for the administration of LA in dentistry, together with appropriate care to prevent needle breakage, may reduce the risk of exposure to blood by an accidental NSI... in this study by almost 36% compared with the 27G needle. However, more investigation in this regard is necessary as a difference in needle lumen diameter may exist between different types of needles.
Disclosure: None
Acknowledgements
The authors gratefully acknowledge the contributions of those who participated in this study and of the following people who contributed to the paper: Drs. L. Snyman and C Postma, School of Dentistry, University of Pretoria, for the statistical analysis; Prof. K-W. Bütow, Emeritus Professor, School of Dentistry, University of Pretoria, for editing the manuscript; and Ms. B. English, the scientific editor in the research office of the Faculty of Health Sciences, University of Pretoria.
ACRONYMS
HBV: hepatitis B virus
HCV: hepatitis C virus
HIV: human immunodeficiency virus
INF: buccal and palatal or labial infiltration
IA: inferior alveolar nerve block
LA: local anaesthetic
NSI: needle stick injuries
PS: posterior superior and greater palatine nerve block
References
1. Siew C, Chang SB, Gruninger SE, Verrusio AC, Neidle EA. Self reported percutaneous injuries in dentists: implications for HBV, HIV, transmission risk J Am Dent Assoc 1992;123:36-44. [ Links ]
2. Gooch BF, Siew C, Cleveland JL, Gruninger SE, Lockwood SA, Joy ED. Occupational blood exposure and HIV infection among oral and maxillofacial surgeons. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;85:128-34. [ Links ]
3. McCarthy GM, Koval JJ, MacDonald JK. Occupational injuries and exposures among Canadian dentists: the results of a national survey. Infect Control Hosp Epidemiol 1999;20:331-6. [ Links ]
4. Gaballah K, Warbuton D, Sihmbly K, Renton T. Needle stick in-juries among dental students: risk factors and recommendations for prevention. Libyan J Med 2012;7:10.3402/ljm.v7i0.17507. [ Links ]
5. Askarian M, Malekmakan L, Memish ZA, Assadian O. Prevalence of needle stick injuries among dental, nursing and midwifery students in Shiraz, Iran. Indian J Med Sci. 2006;60:227-32. [ Links ]
6. Jaber MA. A survey of needle sticks and other sharp injuries among dental undergraduate students. Int J Infect Control 2011;7:doi: 10.3396/ijic.V7i3.022.11. [ Links ]
7. Porter KM, Scully C, Porter SR. Needle stick injuries in dental staff. Br Dent J 1989;167:265-6. [ Links ]
8. Ramos-Gomez F, Ellison J, Greenspan D, Bird W, Lowe S, Gerberding JL. Accidental exposures to blood and body fluids among health care workers in dental teaching clinics: a prospective study. J Am Dent Assoc 1997;128:1253-61. [ Links ]
9. Wicker S, Rabenau HF. Occupational exposures to bloodborne viruses among German dental professionals and students in a clinical setting. Int Arch Occup Environ Health. 2010;83:77-83. [ Links ]
10. Klein RS, Freeman K, Taylor PE, Stevens CE. Occupational risk for hepatitis C virus infection among New York City dentists. Lancet 1991;338:1539-42. [ Links ]
11. Gupta N, Tak J. Needlesticks injuries in dentistry. Kathmandu Univ Med J 2011;9:208-12. [ Links ]
12. Klein RS, Phelan JA, Freeman K, Schable C, Friedland GH, Trieger N,Steigbigel NH. Low occupational risk of human immunodeficiency virus infection among dental professionals. N Engl J Med 1988;318:86-90. [ Links ]
13. Scully C, Greenspan JS. Human immunodeficiency virus (HIV) transmission in dentistry. J Dent Res 2006;85:794-800. [ Links ]
14. Mohebati A, Davis JM, Fry DE. Current risks of occupational blood-borne viral infection. Surg Infect (Larchmt) 2010;11:325-31. [ Links ]
15. Cleveland JL, Barker L, Gooch BF, Beltrami EM, Cardo D. Use of HIV postexposure prophylaxis by dental health care personnel: An overview and updated recommendations. J Am Dent Assoc 2002;133:1619-26. [ Links ]
16. Zakrzewska JM, Greenwood I, Jackson J. Introducing safety syringes into a UK dental school-- a controlled study. Br Dent J 2001;190:88-92. [ Links ]
17. Cleveland JL, Barker LK, Cuny EJ, Panlilio AL. Preventing percutaneous injuries among dental health care personnel. JADA 2007;138:169-78. [ Links ]
18. Krikorian R, Lozach-Perlant A, Ferrier-Rembert A, Hoerner P, Sonntag P, Garin D, Crance JM. Standardization of needlestick injury and evaluation of a novel virus-inhibiting protective glove. J Hosp Infect 2007;66:339-45. [ Links ]
19. Mansouri M, Tidley M, Sanati A, Roberts C. Comparison of blood transmission through latex and nitrile glove materials. Occup Med-C 2010;60:205-10. [ Links ]
20. Bennett NT, Howard RJ. Quantity of blood inoculated in a needlestick injury from suture needles. Obstet Gynecol Surv 1994;49:398. [ Links ]
21. Adegboye AA, Moss GB, Soyinka F, Kreiss JK. The epidemiology of needlestick and sharp instrument accidents in a Nigerian hospital. Infect Control Hosp Epidemiol 1994 15:27-31. [ Links ]
22. Wittmann A, Kralj N, Kòver J, Gasthaus K, Hofmann F. Study of blood contact in simulated surgical needlestick injuries with single or double latex gloving. Infect Control Hosp Epidemiol 2009;30:53-6. [ Links ]
23. Kotze MJ, Labuschagne W. A method to determine the presence of blood in and on a dental needle following the administration of local anesthesia. JADA 2014;145:557-62. [ Links ]
24. Napoli VM, M. JE. How much blood is in a needlestick? J Infect Dis 1987;155:828. [ Links ]
25. Mollen AJ, Ficara AJ, Provant DR. Needles--25 gauge versus 27 gauge-can patients really tell? Gen Dent 1981;29:417-8. [ Links ]
26. Brownbill JW, Walker PO, Bourcy BD, Keenan KM. Comparison of inferior dental nerve block injections in child patients using 30-gauge and 25-gauge short needles. Anesth Prog 1987;34:215-9. [ Links ]
27. Flanagan T, Wahl MJ, Schmitt MM, Wahl JA. Size doesn't matter: needle gauge and injection pain. Gen Dent 2007;55:216-7. [ Links ]
28. Malamed SF, Reed K, Poorsattar S. Needle breakage: Incidence and prevention. Dent Clin North Am 2010;54:745-56. [ Links ]
29. Augello M, von Jackowski J, Gràtz KW, Jacobsen C. Needle breakage during local anesthesia in the oral cavity--a retrospective of the last 50 years with guidelines for treatment and prevention. Clin Oral Investig 2011;15:3-8. [ Links ]
30. Vasconcelos BC do E, Freitas KC de M, Canuto MR. Frequency of positive aspirations in anesthesia of the inferior alveolar nerve by the direct technique. Med Oral Patol Oral Cir Bucal. 2008;13:E371-74. [ Links ]
31. Danielsson K, Evers H, Nordenram A. Aspiration in oral local anaesthesia: frequency of blood in cartridges in undergraduate student material. Swed Dent J 1984;8:265-9. [ Links ]
32. Delgado-Molina E, Bueno-Lafuente S, Berini-Aytés L, Gay-Escoda C. Comparative study of different syringes in positive aspiration during inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:557-60. [ Links ]
33. Lehtinen R, Aarnisalo T. Aspiration in local anesthesia: Comparison between disposable self-aspirating and usual syringes. Acta Odontol Scand 1977;35:9-11. [ Links ]
34. Trapp LD, Davies RO. Aspiration as a function of hypodermic needle internal diameter in the in-vivo human upper limb. Anesth Prog 1980;27:49-51. [ Links ]
35. Delgado-Molina E, Tamarit-Borrás M, Berini-Aytés L, Gay-Escoda C. Evaluation and comparison of 2 needle models in terms of blood aspiration during truncal block of the inferior alveolar nerve. J Oral Maxillofac Surg 2003;61:1011-5. [ Links ]
36. Cooley RL, Robison SF. Comparative evaluation of the 30 gauge dental needle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1979;48:400-4. [ Links ]
37. Simmerville JA, Maxted WC, Pahira JJ. Urinalysis: A comprehensive review. Am Fam Physician 2005;15;71:1153-62. [ Links ]
 Correspondence:
Correspondence:
MJ Kotze
Department of Maxillo-Facial and Oral Surgery
School of Dentistry
Faculty of Health Sciences
University of Pretoria
South Africa
P.O.Box 1266
Pretoria, 0001.
Tel: +27 12 319 2528 Fax: +27 12 319 2172
E-mail: thinus.kotze@up.ac.za













