Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.69 n.10 Johannesburg Nov. 2014
RESEARCH
Knowledge, attitudes and practices of oral health care workers in Lesotho regarding the management of patients with oral manifestations of HIV/AIDS
K J RamphomaI; S NaidooII
IBChD (UWC). MChD (Comm Dent) (UWC). Department of Community Oral Health, University of the Western Cape, Tygerberg
IIBDS (Lon), LDS.RCS (Eng), MDPH (Lon), DDPH.RCS (Eng), MChD (Comm Dent), PhD (US), Dip lint Research Ethics (UCT). Senior Professor and Principal Specialist, Department of Community Oral Health, University of the Western Cape, Tygerberg
ABSTRACT
Lesotho has the third highest prevalence of HIV In the world with an estimated 23% of the adult population infected. At least 70% of people living with HIV/AIDS (PLWHA) have presented with oral manifestation of HIV as the first sign of the disease. Oral health workers regularly encounter patients presenting with oral lesions associated with HIV disease and therefore need to have adequate knowledge of these conditions for diagnosis and management. The aim of the present study was to determine the knowledge, attitudes and practices of oral health care workers (OHCW) of Lesotho regarding the management of oral manifestations of HIV/AIDS. A descriptive cross-sectional survey was conducted on all 46 OHCW in 26 public and private care facilities in all ten districts of Lesotho. A self-administered questionnaire was used to gather information. The response rate was 100%. Nearly all (94.7%) agreed that oral lesions are common in people living with HIV and/or AIDS. The majority (91.3%) named oral candidiasis (OC) as the most common lesion found in PLWHA while Kaposi's Sarcoma (KS) (34.7%) and Oral Hairy Leukoplakia (OHL) (32.6%) were mentioned as the least common oral lesions of HIV. Most correctly identified the images of oral candidiasis (97.8%), angular cheilitis (86.9%) and herpes zoster (80.4%). Only 16.7% felt they had comprehensive knowledge of oral HIV lesions, although 84.8% reported having previously received training. Almost three quarters (71%) reported that there was no need to treat HIV positive patients differently from HIV negative patients. OHCW in Lesotho demonstrated high confidence levels in their competence in managing dental patients with oral lesions associated with HIV, however, they lacked an in-depth knowledge in this regard. Amongst this group there is a need for comprehensive training with regards to diagnosis and management of oral lesions of HIV including the training of other cadres of health care workers together with nurses and community health workers.
Key words: HIV/AIDS, oral health care workers, knowledge, attitudes, practises
ACRONYMS
HAART: Highly active anti retroviral therapy
KAP: knowledge, attitude and practice
KS: Kaposi's sarcoma
OC: oral candidiasis
OHCW: oral health care workers
OHL: oral hairy leukoplakia
PLWHA: people living with HIV/AIDS
INTRODUCTION
Sub-Saharan Africa is home to an estimated 22.5 million HIV infected people out of 33.3 million globally.1 Lesotho has a high adult prevalence (23.6%) of HIV/AIDS, estimated to be the third highest in the world, with nearly a quarter of the adult population infected with HIV.2,3 It has been reported that HIV/AIDS-related infections account for about 10% of all causes of morbidity in males, 13% in females and 6% in children under the age of 12 years in Lesotho.4 Regardless of the wealth of information on oral manifestations of HIV, little is known about the knowledge of oral health care workers (OHCW) and the efficacy of their management of oral HIV lesions in a poorly resourced country such as Lesotho. Dentists and OHCW in general have been identified as being central in providing not only holistic treatment but in preventing the on-going transmission of HIV disease.5 The importance of OHCW is that they are in an ideal position to identify, diagnose, manage and treat HIV-associated oral lesions. Moreover, they have the responsibility, not only to themselves but also to their patients, to be up-to-date with the evolving HIV/AIDS pandemic and related issues.5,6 Knowledge of the HIV disease process, its oral manifestations and modes of transmission is strongly associated with readiness to provide treatment to patients.7,8,9
If OHCW were skilled in this regard, they would be well positioned to diagnose and identify the signs and symptoms of oral manifestations of HIV/AIDS at an early stage. Moreover, they would be able to prevent the spread of HIV infection as well as the progression of the disease and the debilitating consequences if it is left untreated. In addition, they will be able to refer patients for the initiation of HAART treatment, resulting in decreased morbidity and mortality and consequent improvement in quality of life of PLWHA.
It has been established that the presence of oral lesions associated with HIV in persons who may otherwise appear healthy may be indicative of the early clinical signs of HIV infection. Oral HIV lesions may also predict disease progression and may act as clinical markers for staging and classification of HIV.10-12 Several studies have shown that oral manifestations of HIV/AIDS occur in as many as 70-90% of all HIV/AIDS cases in both children and adults, and these conditions may be prevented or treated with regular dental care.11-16 If left untreated, these lesions may cause discomfort and dysfunction, and can impact negatively on the oral health quality of life of an individual.17,18
It has been reported that many people living with HIV/AIDS do not receive adequate oral care treatment. Some of the identified barriers to care include financial problems, lack of confidentiality, socio-psychological factors such as prejudice and discrimination among dental health workers.13-15 The high prevalence of HIV and its oral manifestations warrants that all OHCW should be well-equipped with the appropriate knowledge and skills in the management of PLWHA.
METHODOLOGY
This was a descriptive cross-sectional study conducted during two weeks in July 2012 using a self-administered questionnaire and visual aids. Participants (n=46) were oral health care workers in Lesotho from 26 public and private dental health care facilities from all 10 districts of Lesotho. Respondents included dentists (n=26), dental therapists (n=4), oral hygienists (n=1), dental assistants (n=10), nurse assistants (n=3) and denta technologists (n=1), all trained to perform dental Employn work. Ethical approval was obtained from the University of the Western Cape Senate Research Ethics Committee and the Research and Ethics Committee of the Ministry of Health and Social Welfare, Planning and Development Unit of Lesotho.
The questionnaire comprised of four sections and consisted of 18 questions eliciting socio-demographic information, knowledge regarding oral manifestations of HIV, attitudes concerning the management of PLWHA and behavioural practices on the subject of oral manifestations of HIV/AIDS. Section A consisted of independent variables such as age, sex, qualification, years of experience as an OHCW, employment status, and employment sector. Knowledge questions related to the identification of oral lesions and the description thereof. Visual references used were seven unlabelled images of common oral lesions associated with HIV/AIDS. Furthermore, participants were questioned on the different sources of their knowledge and education regarding these oral conditions. Most questions in the attitude section were on the willingness of OHCW to treat PLWHA, their reactions to treating them, their thoughts about referring such patients and if they felt PLWHA needed to be treated differently from patients who are not HIV-infected. Behavioural practice questions pertained to instructions given to patients when they present with different oral conditions such as toothache, bleeding gums and oral ulcers.
Data was captured using a Microsoft Excel spread sheet before it was imported into the R Statistical Package. In the statistical evaluation, frequency distributions and means were generated. Regression analysis was used to analyse the relationship between continuous variables while the relationship between nominal variables was investigated using contingency tables (2x2) and chi-squared tests. In addition, Fisher's exact test was applied to each of the 2x2 contingency tables on dependent and independent variables. To identify associate variables, a significance level of 5% (p<0.05) was used.
RESULTS
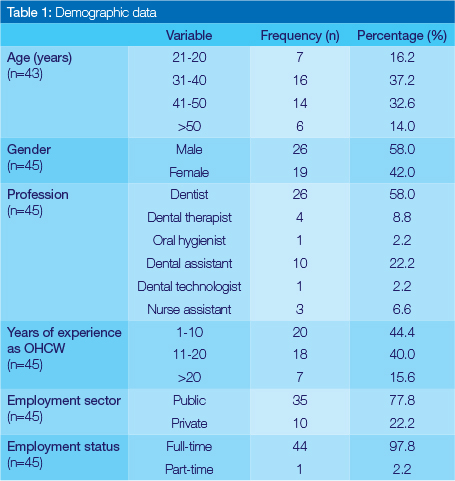
The response rate of the study was 100%. Study sites included 26 facilities throughout the country, and these were district hospitals (n=10), satellite filter clinics (n=3), health centre (n=1), missionary hospitals (n=5), military hospitals (n=1) and private practices (n=6) all of which offer dental services. The majority (58.0%) of the respondents were male. The age range of the sample was between 25 and 73 years with the mean age of 41 years. Nearly two thirds (58.0%) were qualified dentists. The number of years of experience ranged from 2 to 45 years (mean 13.5 years). Just over three quarters (77.8%) worked in the public sector and nearly all (97.8%) worked full-time (Table 1).
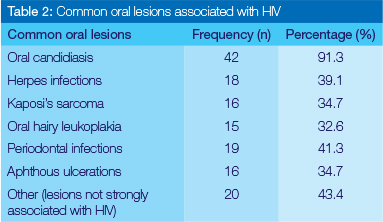
Participants were asked a closed-ended question to state whether oral lesions are common in PLWHA, and the vast majority (94.7%) agreed that these lesions are common. They were further asked to list the five most common oral lesions associated with HIV and to rank according to frequency. Oral candidiasis was ranked as the most common oral manifestation (91.3%) while oral hairy leukoplakia was listed as the least common oral lesion in HIV (32.6%).
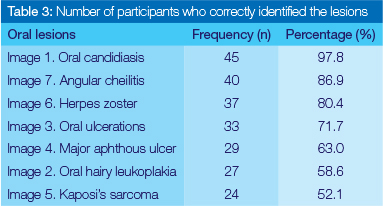
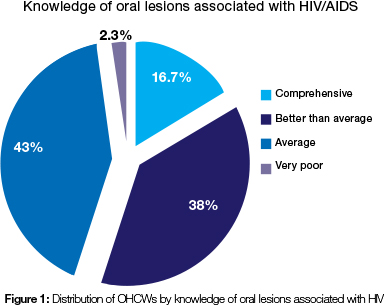
Participants were given seven unlabelled images of lesions strongly associated with HIV and asked to identify the lesions. Oral candidiasis was correctly identified by most respondents (97.8%), angular cheilitis by 86.9% and herpes zoster by 80.4%. Just over half (52.1%) of respondents correctly identified Kaposi's Sarcoma (Table 2, 3). When asked to rate their HIV knowledge, less than a fifth (16.7%) of the respondents felt that they had a comprehensive knowledge of the oral manifestations of HIV while almost half said they had average knowledge of oral HIV (Figure 1).
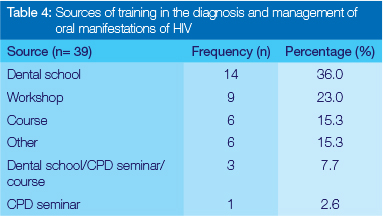
Eighty five percent (n=39) reported having received training in the diagnosis of oral lesions associated with HIV - the majority while they were at Dental School. Those participants who were not dentists, dental therapists or oral hygienists, had received training mainly from the attendance at workshops (Table 4). Despite this background, nearly all respondents (91.1%) said they felt they still required further training in understanding the oral manifestations of HIV.
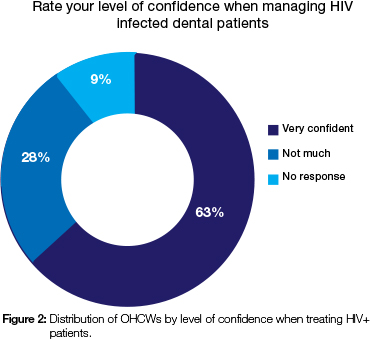
When asked about their attitudes when managing PLWHA, almost all participants (93.4%) said they did not mind treating PLWHA while 6.6% said they were not sure. The majority (95.7%) felt that patients who are HIV positive should be referred for dental treatment and more than half the participants (57.0%) said referrals should be to public dental clinics. More than two thirds (71.0%) reported that it was not necessary to treat PLWHA differently from HIV negative patients. Almost all participants (95.7%) reported having knowingly treated an HIV positive patient in the past six months and nearly two thirds (59.0%) perceived the risk of contracting HIV in the dental clinic to be high. Approximately two thirds (63.0%) reported that they felt very confident in the management of dental patients with HIV/AIDS (Figure 2).
Participants were asked if they would give the same treatment and/or advice to both HIV+ and HIV- patients presenting with the same dental diseases to which the majority reported that they would (70.0%). Almost all (90.7% n=39) said they gave the same treatment for patients presenting with dry mouth, regardless of the HIV status. Most respondents did not treat HIV positive patients any differently from HIV negative dental patients with more than two thirds giving the same treatment for any dental condition (Table 5, Figure 3).
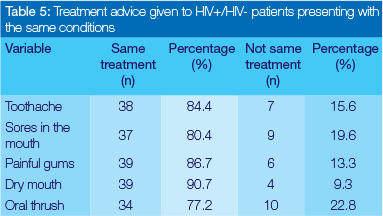

For common oral conditions found in HIV-infected and non-HIV infected patients, over two thirds of OHCW administer the same treatment with a slight difference in patients presenting with oral thrush where 22.8% (n=10) said they would not give the same treatment/advice.
Further correlations were performed between selected demographic characteristics (age, years of experience and employment sector) and selected questions on the knowledge, attitudes and practice sections. One question was considered for each of the KAP sections for correlations. The cross-tabulations were used to determine if there were any significant associations between the selected variables and the different KAP sections. The Fisher's exact test of association was applied to 2x2 contingency tables and the significance was set at p=0.05. The results are reported with the exact p-values.
Cross-tabulations were performed to determine the relationship between the age of OHCW and their knowledge of oral lesions associated with HIV with the purpose of determining whether age increased knowledge of HIV-associated lesions. The median age of 39 years old was used for this association instead of the mean due to the skewed nature of the data caused by the presence of outliers. OHCW were categorized in two groups of <39 and >39 years. The results show that the majority of the participants from both age groups who had previously seen oral candidiasis could correctly identify it. However, a greater proportion of participants above >39 years old (n=5) could not correctly identify angular cheilitis despite the fact that only one of them had not seen the lesion previously (p=0.021) as compared with the <39 year old group who all correctly identified the lesion. It was also observed that not all participants who had seen the lesions previously were able to correctly identify them. However, some who claimed they had not seen some lesions before were in fact able to identify them correctly. A correlation made between the two employment sectors of OHCWs (private and public) and their knowledge with regards to the ability to identify oral HIV lesions revealed several significant findings. OHCW in the public sector encounter patients presenting with oral manifestations of HIV more frequently than their counterparts in the private sector: candidiasis (n=34; p =0.048), oral hairy leukoplakia (n=28; p=0.023), herpetic gingivostomatitis (n=32; p=0.005) and herpes zoster (n=30; p=0.0149). In addition, public sector workers had a significantly better ability to correctly identity herpetic gin-givostomatitis (n=29; p = 0.030) and herpes zoster (n=31; p=0.0257) than those in the private sector (Table 6).
DISCUSSION
The present study sought to determine the knowledge, attitudes and practices of oral health care workers in Lesotho regarding the management of oral HIV/AIDS related lesions. All the participants consented and completed the questionnaires. While most countries legally permit dentists and dental therapists to perform invasive dental procedures such as dental extractions, minor dental surgeries and restorations, in Lesotho, due to the dire shortage of OHCW, oral hygienists, dental assistants, dental technologists as well as nurse assistants are also entrusted with clinical responsibilities.
The majority of the participants (44.4%) had a range of 1-10 years of experience and this may be due to the fact that most qualified dentists are emigrants who work in Lesotho immediately after they attain their dental degrees in their countries and often are on short-term contracts.
The results of the present study revealed that OHCW demonstrated a fair knowledge of oral manifestations of HIV with nearly all in agreement that oral lesions are a common finding in PLWHA and this concurs with the literature.13,19,20 This was also in agreement with the findings of other studies conducted in Lesotho confirming the high prevalence of oral lesions in PLWHA.14,21,22 The majority listed oral candidiasis as the most common oral lesion associated with HIV, which also highlights the high prevalence of this lesion in PLWHA in Lesotho. This result was similar to the findings of several studies.22,23,24,25,26
Oral lesions of HIV such as periodontal infections, herpes infections, Kaposi's sarcoma and Oral hairy leukoplakia are classified as lesions strongly associated with HIV.28 However, fewer than half of the OHCW listed these l esions as l ess common than documented in the literature. This result concurred with the results of another South African study where less than 50% of the participants named oral hairy leukoplakia, herpes infections and periodontal diseases as common lesions of HIV, with the exception of Kaposi's sarcoma.24 This was contrary to the findings in the Kenyan study where more than half of all the participants correctly identified periodontal infections, herpes infections, Kaposi's sarcoma and oral hairy leukoplakia as lesions strongly associated with HIV.23 This could be due to the fact that the study participants were all dentists.
The presence of Kaposi's sarcoma is indicative of disease progression and high mortality. A study conducted in PHC facilities in South Africa revealed the significance of early diagnosis and timely access to HAART and chemotherapy for patients with KS.29 Lack of adequate knowledge of this lesion by OHCW may lead to a delayed diagnosis resulting in detrimental effects, including morbidity and mortality.
Oral hairy leukoplakia is similarly strongly associated with HIV and its presence signposts progression to AIDS. A probable explanation for OHCW describing these lesions as uncommon may indicate that the lesions are not encountered as frequently as oral candidiasis and herpes infections, or may signify a lack of knowledge of these lesions and their association with HIV/AIDS. Regardless, these findings suggest that OHCWs require further training to prevent delayed diagnosis, which may lead to poor health and quality of life caused by discomfort, dysfunction and disability.18
While 84% of the participants reported to have received training in the diagnosis of oral lesions of HIV, less than a fifth perceived that they had comprehensive knowledge of oral HIV lesions. Just over a third felt their knowledge was 'better than average' and nearly all expressed the need for further training in this regard. In a study on South African dentists, 71% of the respondents thought they had adequate knowledge of HIV.24 This may be attributed to the fact that the study was conducted only on dentists as opposed to all other cadres of OHCW. There is a need for training and education in the management of PLWHA on a continuous basis and in the form of regular refresher courses.
Participants were asked to identify seven unlabelled photographic images depicting oral lesions strongly associated with HIV. The images correctly identified by the majority of participants were oral candidiasis, angular cheilitis herpes zoster and oral ulcerations respectively. Just over half of the participants correctly identified Kaposi's sarcoma and oral hairy leukoplakia, which are lesions strongly associated with HIV. Even though some of these lesions were listed by the participants in the questionnaire as less commonly associated with HIV, slightly higher proportions were able to identify them correctly when provided with the visual images. This result may be due to increased uptake of HAART therapy, which significantly reduces the prevalence of oral lesions of HIV.10,29-32 It may also indicate poor practical knowledge and perhaps a low appreciation of the significance of history taking in identifying specific oral lesions, because the onset of some conditions as expressed by patients will often aid the diagnosis. Nearly all participants in the present study correctly identified oral candidiasis as the most common oral HIV lesion and this finding is similar to other studies.23,24,33
Many of the correlations conducted showed statistically insignificant results and this may likely be attributed to the small sample population of the study (n=46), even though this was representative of the whole population of OHCW in Lesotho. There were statistically significant results between knowledge and employment sector suggesting that participants working in the public sector more frequently encountered common oral lesions associated with HIV and were more able of correctly identifying them than were their private practice colleagues. The association between knowledge and years of experience showed that the knowledge of HIV by OHCW increases with an increase in the number of years of experience, however, the results were not statistically significant.
In the current study, almost all participants showed a willingness to treat PLWHA, which may be explained by the current wealth of knowledge of HIV and its routes of transmission and the appropriate infection control measures. The high response rate on willingness to treat concurred with other studies.8,9,23,35,36 Furthermore, knowledge regarding the risk of transmission of HIV and the use of infection control measures has been identified by some as factors associated with a willingness to treat HIV/AIDS patients where the OHCW may otherwise have been fearful regarding cross-infection.7,9,36 The high willingness reported in the present study may indicate the fact that OHCW are cognizant of their ethical obligation in providing treatment to all patients. A South African study reported similar findings where 81.5% of the participants were willing to treat PLWHA based on their professional responsibility.26
While the vast majority of OHCW of Lesotho showed willingness to treat HIV/AIDS patients, a surprising 59% believed that the risk of contracting HIV in the dental clinic was high. This general misconception is consistent with other studies.9,23,37 More than two thirds reported that there was no need to treat HIV-positive patients differently while those who disagreed felt that on account of their immunocompromised state and prescribed drugs, special care was needed. Many of those who felt HIV-positive patients needed to be referred named public dental clinics and dedicated HIV clinics as facilities to which patients should be referred. This was also consistent with other findings where participants felt patients must be referred to dedicated clinics, academic hospitals and to dentists with special training.23,24
Though it is the responsibility of OHCW to effectively manage the oral health conditions of PLWHA just as they would for any other patient, the challenges with PLWHA are many, including possible neglect of oral hygiene due to pain and discomfort. This, however, does not justify poor management of PLWHA.32,38 Generally, one would not adapt the dental treatment of a patient merely based on their HIV status, however, certain considerations such as the referral of the patient for further management may be necessary due to the patient's immunocompromised state.
Participants were asked to rate their confidence levels in managing PLWHA and to specify if they would provide the same treatment options and/or advice for five common oral diseases/conditions, which may be found in PLWHA and HIV-negative patients. Nearly two thirds reported high levels of confidence in managing PLWHA. They stated that they would give the same treatment to both PLWHA and the HIV-negative patients presenting with the same oral diseases. For those who opted for different treatment/advised, the reasons mentioned were positively discriminatory towards PLWHA. For example, they would provide the patient with prophylactic antibiotic cover prior to dental extraction and they would spend more time emphasizing the importance of individual oral self-care because of increased susceptibility to infections.
It has been established that severe oral ulcerations may occur in HIV-infected patients, often characterized by pain and fever. These may range from recurrent aphthous ulcers, herpes infections, cytomegalovirus infections and Epstein-Barr virus infections.17 However, a South African study reported a small prevalence (2.9%) of oral ulcerations in a group of 600 HIV-positive patients and these findings were consistent with the findings of another study, conducted in India.16,39
As regards patients presenting with sores in the mouth, the vast majority of OHCW reported that they would offer the same treatment after taking a thorough medical examination to establish the aetiology, duration and frequency of the ulcers. Different treatments suggested included advice to HIV-negative patients to go for testing and counselling, referral for blood tests to establish the causes of ulcerations and if widespread, referral to a physician for further management.
Periodontal diseases such as linear gingival erythema, necro-tizing ulcerative gingivitis, necrotizing ulcerative periodontitis and necrotizing stomatitis have been reported to be highly predictive of the underlying HIV infection in individuals who may seem otherwise healthy. Associated symptoms include bleeding gums, tooth mobility and general discomfort in the mouth.12,40 Less than half of the participants in the present study listed periodontal diseases as common lesions of HIV and almost all reported that they would not give different treatment to patients presenting with painful gums. This finding may likely indicate lack of knowledge since periodontal diseases have been described as a common finding in PLWHA. A few participants reported that they would refer such patients for HIV testing and counselling and for CD4 cell count tests.
HIV-infection may lead to a reduction in the flow of saliva, which may be indicative of salivary gland dysfunction and a side-effect of long-term HAART therapy. Furthermore, dry-mouth in PLWHA has been found to be crucial in the HIV disease progression.30,41 The management of xerostomia in PLWHA is vital considering the discomfort it causes the patient and the inability to function adequately. An overwhelming majority of the OHCW reported that they would give the same treatment or advice to both HIV+/ HIV- patients presenting with xerostomia. Less than ten per cent stated that they would probe further into the medical history of the patient specifically regarding the medications taken by patients and advise accordingly. A possible explanation for this is that OHCW may not be aware of the association between xerostomia and HIV/AIDS, or that they do not frequently encounter patients presenting with xerostomia.
The majority of respondents reported that they would provide the same treatment to both categories of patients presenting with oral candidiasis. However, others suggested that they provided different treatment options for PLWHA presenting with oral thrush, including recommending for a CD4 count test and prescribing systemic antifungal medication instead of topical antifungals. They also stated that they would recommend HIV testing and counselling for HIV-negative patients or patients whose status is unknown, and who present with oral thrush. The management practices of OHCW are in line with the recommendations for treatment of oral candidiasis where systemic antifungals such as fluconazole are especially required in cases where a definitive HIV diagnosis has been made. OHCW also mentioned the use of topical antifungals such as amphotericin B and nystatin for mild cases of candida infections, which have also been reported to be effective.17
CONCLUSION
The present study has not only highlighted the pivotal role played by OHCW in the identification, diagnosis and management of oral manifestations of HIV/AIDS but has also provided some insight into the knowledge, attitudes and practices of OHCW in Lesotho regarding the management of oral lesions associated with HIV/AIDS. In resource-limited settings such as Lesotho, the value of their role cannot be overemphasised, especially considering the high prevalence of HIV coupled with the dire shortage of human resources in health management including OHCW. It further revealed that above average knowledge yields positive attitudes and good, acceptable practices. However, further training concerning risk in the dental clinic setting is required and this may help to dispel fears and lead to more positive attitudes and an increased willingness to treat patients. The present study focussed only on OHCW and it may be useful to investigate the knowledge, attitudes and practices of other cadres of healthcare workers (nurses, community health care workers etc.) regarding their KAP of the oral manifestations of HIV/AIDS. In view of the shortage of OHCWs, it is recommended that these health professionals also be trained in the diagnosis and management of oral lesions of HIV.
References
1. UNAIDS AIDS epidemic update. Geneva, Switzerland. October 2010 [ Links ]
2. Ministry of Health and Social Welfare. National anti retroviral guidelines, July 2007 [ Links ]
3. USAID Lesotho, HIV/AIDS profile, 2009 [ Links ]
4. Government of Lesotho. Ministry of Health and Social Welfare. 2011. Lesotho Health Policy Available at: http://www.nationalplanningcycles.org [ Links ]
5. McLean AT, Wheeler EK, Cameron S, Baker D. HIV and dentistry in Australia: clinical and legal issues impacting on dental care. Australian Dental Journal. 2012; 57:256-70 [ Links ]
6. Robinson PG. Implications of HIV Disease for Oral Health Services. Adv Dent Res. 2006; 19:73-9 [ Links ]
7. McCarthy GM, Koval JJ, Morin RJ. Factors associated with dentists' willingness to treat HIV-infected patients. In: Greenspan JS, Greenspan D. The Oral Manifestations of HIV Infection. Chicago, Ill: Quintessence Publishing Co Inc.1995; 351-5 [ Links ]
8. Godin G, Naccache H, Brodeur JM, Alary M. Understanding the intention of dentists to provide dental care to HIV and AIDS patients. Community Dent Oral Epidemiol. 1999; 27: 221-7 [ Links ]
9. Irigoyen M, Zepeda M, Lopez-Camara V. Factors associated with Mexico City dentists' willingness to treat AIDS/HIV-positive patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998; 86: 169-74 [ Links ]
10. Chapple LC, Hamburger J. The significance of oral health in HIV Sex Transm Infect. 2000; 76:236-43 [ Links ]
11. Ramos-Gomez FJ, Petru A, Hilton JF. Oral manifestations and dental status in paediatric HIV infection. Int J Paed Dent. 2000; 10:3-11 [ Links ]
12. Coogan MM, Greenspan J, Challacombe SJ. (2005). Oral lesions in infection with human immunodeficiency virus. Bulletin of the World Health Organization. 2005; 83(9) 700-6 [ Links ]
13. Seacat JD, Litt MD, Adam S, Daniels MS. Dental students treating patients living with HIV/AIDS: the influence of attitudes and HIV knowledge. J Dent Ed. 2009:73 (4) 34-9 [ Links ]
14. Kamiru HN, Naidoo S. Oral HIV lesions and oral health behaviour of HIV-positive patients attending the Queen Elizabeth II Hospital, Maseru, Lesotho. SADJ: Journal of the South African Dental Association. 2002;57(11) 479-82 [ Links ]
15. Patton LL, Phelan JA, Ramos-Gomez FJ, Nittayananta W, Shiboski CH, Mbuguye TL. Prevalence and classification of HIV-associated oral lesions. Oral Dis. 2002; 8 (Suppl 2):98-109 [ Links ]
16. Arendorf TM, Bredekamp B, Cloete CAC, Sauer G. Oral manifestations of HIV infection in 600 South African patients. Journal of Oral Pathology and Medicine. 1998;27: 176-9 [ Links ]
17. Johnson NW, Glick M, Mbuguye TNL. Oral health and general health. Adv Dent Res. 2006; 19:118-21 [ Links ]
18. Yengopal V, Naidoo S. Do oral lesions associated with HIV affect quality of life? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(1): 66-73 [ Links ]
19. Nichols CM, Flaitz CM, Hicks MJ. Treating Kaposi's lesions in the HIV infected patient. J Am Dent Assoc. 1993; 124: 78-84 [ Links ]
20. Lim AA, Leo YS, Lee CC, Robinson AN. Oral manifestations of human immunodeficiency virus (HIV) - infected patients in Singapore. Annals of Academic Medicine in Singapore. 2002; 30: 600-6 [ Links ]
21. Walid EI, Nasir F, Naidoo S. Oral health knowledge, attitudes and behaviour among nursing staffing Lesotho. South African Dental Journal. 2004;59: 288-92 [ Links ]
22. Prithiviraj TG. Knowledge, attitudes and practice among Primary Health Care nurse practitioners regarding oral health and oral HIV lesions in QE II and Roma health service areas in Maseru Lesotho. Masters Thesis (MPH). University of the Witwatersrand 2012 [ Links ]
23. Gachigo JN, Naido S. HIV/AIDS: the knowledge, attitudes and behaviour of dentists in Nairobi, Kenya. South African Dental Journal. 2001; 56(12):587-91 [ Links ]
24. Darling M, Arendorf T, Samaranayake LP. Oral care of HIV infected patients: the knowledge and attitudes of South African Dentists. J Dent Assoc S Afric. 1992; 47(9):399-402 [ Links ]
25. Malele-Kolisa Y. Knowledge, attitudes and practices of caregivers about oral lesions in HIV positive patients in NGOs / CBOs in Region, Johannesburg, Gauteng. Thesis (MChD) University of the Wit-watersrand. South Africa 2009 [ Links ]
26. Rudolph MJ, Ogunbodede EO. HIV infection and oral health care in South Africa. South African Dental Journal. 1999; 54(12):594-601 [ Links ]
27. EC-Clearinghouse on Oral Problems related to HIV Infection. WHO Collaborating Centre on Oral Manifestations of the Immunodeficiency Virus. Classification and diagnostic criteria for oral lesions in HIV infection. J Oral Pathol Med. 1993; 22:289-91 [ Links ]
28. Chu KM, Mahlangeni G, Swanne S, Ford NP, Boulle A, Van Cutsem G. AIDS-associated Kaposi's sarcoma is linked to advanced disease and high mortality in a primary care HIV programme in South Africa. Journal of the International AIDS Society. 2010; 13(23):2-5 [ Links ]
29. Frezzini C, Leao JC, Porter S. Current trends of HIV disease of the mouth. J Oral Pathol Med. 2005; 34(9):513-31 [ Links ]
30. Scully C, Laskaris, Porter SR. Oral manifestations of HIV infection and their management. I. More common lesions. Oral Surg, Oral Med, Oral Pathol. 1991;71(2): 158-64 [ Links ]
31. Johnson NW. The mouth in HIV/AIDS: markers of disease status and management challenges for the dental profession. Australian Dental Journal. 2010; 55(1): 85-102 [ Links ]
32. Agbelusi GA, Wright AA. Oral lesions as indicators among routine dental patients in Lagos Nigeria. Oral Diseases. 2005; 11:370-3 [ Links ]
33. Kitaura H, Adachi K, Kobayashi K, Yamada T. Knowledge and attitudes of Japanese dental health care workers towards HIV related disease. Journal of Dentistry. 1997; 25(3-4): 279-83 [ Links ]
34. Bennett ME, Weyant RJ, Wallisch J, Green G. A national survey: Dentists' attitudes towards the treatment of HIV-positive patients. JADA. 1995;126: 509-14 [ Links ]
35. Bodhade A, Dive A, Khandekar S, Dhoble A, Moharil R, Gayakwad R, Tekade S. Factors associated with refusal to treat HIV-infected patients: national survey of Dentists in India, Science Journal of Public Health. 2013;1(2):51-5 [ Links ]
36. Kaste LM, Bednarshe H. The third decade of HIV/AIDS: A brief epi-demiologic update for Dentistry. Journal of Canadian Dental Association. 2007; 73(10): 941-44 [ Links ]
37. Diz-Dios P, Fernandez-Feijoo J, Vazquez-Garcia E. Tooth extraction in HIV sero-positive patients. Int Dent J. 1999; 49: 317-21 [ Links ]
38. Ranganathan K, Hemalatha R. Oral lesions in HIV infection in developing countries. An overview. Adv Dent Res. 2006; 19: 63-8 [ Links ]
39. Nokta M. Oral manifestations associated with HIV infection. The science of HIV medicine. Curr HIV / AIDS Rep. 2008; 5: 5-12 [ Links ]
40. Younai FS, Marcus M, Freed JR, Coulter ID, Cunningham W, Der-Martirosian C, Guzman-Bercerra, N, Shapiro M. Journal of Oral Surg, Oral Med, Oral Path. 2001; 2(6): 629-636 [ Links ]
 Correspondence:
Correspondence:
S Naidoo
Faculty of Dentistry
University of the Western Cape
Private Bag X1 Tygerberg, 7505
Tel: 021 937 3095
Fax: 021 931 2287
E-mail: suenaidoo@uwc.ac.za













