Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.69 no.9 Johannesburg Out. 2014
CLINICAL WINDOW
What's new for the clinician? Summaries of and excerpts from recently published papers
Compiled and edited by WG Evans
1. Dental sealants and restorations and urinary bisphenol: a concentrations in children in the 2003 -2004 National Health and Nutrition Examination Survey (USA).
C McKinney; T Rue; S Sathyanarayana; M Martin; AL Seminario; T DeRouen
Whilst bisphenol A (BPA) is not an actual ingredient of the bisphenol A-glycidal methacrylates (bis-GMA), it is thought to occur as a trace material resulting from the manufacturing process or as a result of degradation of bis-GMA. Hence there is a risk of exposure to BPA in patients having dental sealants or composite restorations and indeed raised levels of BPA have been shown in saliva and in urine after patients had received bis-GMA compounds even when BPA was not an active ingredient.
BPA has been identified as an agent disrupting endocrines, altering hormonal function. This can affect neurodevelopment, reproductive development and metabolic processes. Young patients could be at these risks. Recognising the increasing public concern and awareness of the adverse effects of BPA the authors undertook a survey based on data accumulated during the 2003/2004 National Health and Nutrition Examination Survey (NHANES), hypothesising that a greater number of dental sealants or composite restorations would be associated with higher levels of urinary BPA.
After sorting the initial sample (n=2517) for age (6 to 19) and missing data, a final sample of 1001 participants was identified, all of whom had data available on either or both dental sealants and restorations. As regards the extent of sealant application only occlusal surfaces were included whilst restorations involving any surface were considered, recognising also that the records did not identify the restorative material used. The teeth evaluated were premolar and first permanent molars.
Basic design variables and potential confounders were recorded. There was an adjustment for creatinine levels to account for urinary dilution. As there are other potential sources of BPA the research took account of exposure such as the number of restaurant meals per week, number of school lunches per week, amount of bottled water consumed and various demographic co-variates. Comprehensive statistical analyses took account of all these variables and adjusted the data accordingly.
ACRONYMS
BPA: bisphenol A
bis-GMA: bisphenol A-glycidal methacrylates
Children with seven to 16 sealants had geometric mean concentrations of BPA, 25 percent higher than those in children having no sealants. An increase of ten sealants was associated with increases of 18 percent of the geometric mean BPA concentration. In children having between seven and 42 restorations, the geometric mean values were five and 20 percent higher than those with no restorations, depending on whether the analyses were adjusted or not.
Although there were observed relations between the urinary levels of BPA and the numbers of sealants and/or restorations, no significant associations were shown. A previous study on adults had shown significant increases in urinary BPA nine to 30 hours after placement of restorations, whilst a small study based on 19 children had demonstrated raised levels two weeks after four or more sealants or composites.
The current study did not have data on the types of sealants and restorations. It may be suggested that at least some of the materials did not have BPA derivatives, which would bias the results towards finding no association. The study did not confirm nor refute the possibility that degradation of dental sealants or restorations increases BPA concentrations. Recent studies have suggested that greater exposure to GMA-based dental composite is associated with worse psychosocial function and adverse reproductive development. The authors conclude that their study does not provide convincing evidence that the presence of sealants is NOT associated with higher levels of BPA and that therefore careful attention should continue to be paid to this issue.
Reference
1. McKinney C, Rue T, Sathyanarayana S, Martin M, Seminario AL , DeRouen T. Dental sealants and restorations and urinary bisphenol A concentrations in children in the 2003 -2004 National Health and Nutrition Examination Survey. The Journal of the American Dental Association 2014; 145(7) : 745 - 50. [ Links ]
2. The temporomandibular opening index, report of headache and TMD, and implications for screening in general practice: an initial study.
VJ Miller; VV Karic; R Ofec; SR Nehete; A Smidt
The temporomandibular opening index is derived by contrasting the measurements of the passive and voluntary openings of the mouth in the formula:
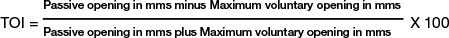
Passive opening is guided by pressure from thumb and finger against the jaws to an endfeel position.
Maximum voluntary opening is that position achieved by the patient in stretching opening to capacity.
The TOI has been shown to be useful in distinguishing myogenous from arthrogenous Temporomandibular dysfunction (TMD). Both forms are characterised by pain , by joint sounds and by limitation of mandibular movement. The pain in the myogenous group is predominantly muscular in origin, whilst the arthrogenous source of pain is the joint. Apart from a number of associated symptoms such as earache, tinnitus, allodynia and chronic fatigue, TMD has been identified as a factor in patients who suffer headaches. Both migraine and tension headaches appear to be associated with TMD and treatment for TMD can contribute towards relief from headaches. However, there has been sparse attention paid to possible differences in the relationships of headache in myogenous as compared with arthrogenous TMD. Certainly patients with a high TOI in a myogenous pain presentation had more severe problems than those with a low TOI. The study was therefore designed to test the null hypothesis that there is no difference between myogenous, arthrogenous and control TMD patients with regard to reported headache.
ACRONYMS
TMD: Temporomandibular dysfunction
VRS: Verbal Rating Scales
The study included 66 patients who presented with TMD in comparison with a control group of 20 patients with no signs or symptoms of TMD. In all patients there was a normal complement of teeth, and no gross caries or severe periodontal disease was present. Those with systemic disease were however excluded as there could be an element of comorbidity. Data feedback from all patients was recorded on simple four point Verbal Rating Scales (VRS) which requested details on frequency and severity. Those patients who reported headaches were then divided into myogenous and arthrogenous groups. Seventeen myogenous TMD patients were assessed on a VRS for intensity and frequency of headaches. The Severity and Frequency scores were added to provide a composite Headache score, which could range from zero to six. These patients were then further divided according to their TOI scores, a high group having TOI scores greater than 8% and a low having scores below 8%. Statistical analysis was completed with the aid of SPSS Statistics software, and included multiple logistic regression analysis, a Mann-Whitney test and a two tailed test with □ = .01.
Age and myogenous TMD were shown to be significantly associated with reported headache whilst no such relationship was found for arthrogenous TMD . The Mann-Whitney test demonstrated a significant difference in the reporting of headache between the high and low TOI groups.
Taking into account the small sample size it is wise to be cautious in interpreting the results as indicating that there are two distinct groups of myogenous patients. It is likely that a comorbidity effect Is influencing the results. The more severe the headache In the high TOI group, the greater muscle contraction and hence higher pain perception. The muscle contraction reduces voluntary mouth opening but allows greater endfeel distance and hence a higher TOI.
The TOI is a useful clinical assessment allowing quick and decisive screening. High TOI levels In a patient will be associated with more severe TMD symptoms.
Reference
1. Miller VJ, Karic VV, Ofec R, Nehete SR, Smidt A, The temporomandibular opening Index, report of headache and TMD, and Implications for screening In general practice. An Initial study. Quintessence International 2014;45 (7) : 605-11. [ Links ]













